Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Pericoronitis is a popular dental disease that most often affects the gums of the lower jaw near the wisdom tooth. This is an inflammation of the gingival structures that occurs due to teething. The main thing is not to confuse periodontal disease. As a rule, the pathology occurs in people of older age groups and is accompanied by very unpleasant symptoms.
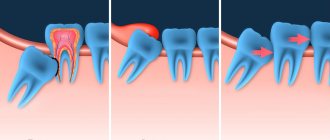
“Eight” is considered one of the most problematic teeth. Not surprisingly, these teeth appear later than all others, there is little space left for them. Therefore, often the wisdom tooth remains in the jaw without erupting. Sometimes the “figure eight” rests on neighboring teeth and cheeks, grows at an angle and causes a lot of unpleasant sensations.
Causes of pericoronitis
The disease most often results from:
- epithelial injuries due to difficult long-term tooth eruption;
- impacted (formed, but not erupted outward) teeth;
- atypically located tooth roots;
- thickening of the gum mucosa;
- accumulation of soft plaque under the hood and, accordingly, infection of tissues;
- reduction in the size of the dental arch, lack of space for teething;
The catalyst for pericoronitis of wisdom teeth is often a source of infection in the oral cavity. Very often the disease is provoked by caries, stomatitis or periodontitis. Sometimes the disease occurs against the background of ignoring the rules of personal hygiene, prolonged stress, hypovitaminosis and other conditions accompanied by decreased immunity.
Why do eights almost always grow incorrectly?
The rudiments of wisdom teeth form in all people, but they do not always erupt completely, and may not appear above the gum at all. They begin to grow last, at about 25 years of age. The problem is that eights are rudiments that we inherited from our ancestors. In ancient times, when people had to eat raw meat, their jaw system was much larger, and the wisdom teeth in it performed the function of thoroughly crushing solid food.
Evolution has greatly changed our appearance, and the jaw arches have noticeably decreased in size over time. Therefore, there is simply not enough space left for the eights, and this is one of the main reasons why in most cases they lie horizontally and grow in the wrong position. As a result, excessive pressure is exerted on neighboring elements, which leads to deformation of the entire row.
Third molars grow very slowly and often remain half under the gum - this phenomenon is called retention. When an impacted wisdom tooth is also in a horizontal position, experts diagnose it as dystopia. All this usually leads to the development of inflammatory processes in the mucous membrane and rapid destruction of dental tissues by caries.
Symptoms of tooth pericoronitis
The main clinical manifestations of dental pericoronitis may be the following symptoms:
- swelling of the soft tissue of the gums in the area of the growing tooth;
- redness of soft tissues;
- pain that worsens when eating and brushing teeth;
- pain radiating to the temple, ear or eye socket (on the affected side);
- Difficulty opening the mouth and talking due to pain and swelling;
- bad breath;
- purulent discharge from under the gingival hood;
- increase in body temperature to 37.5 degrees.
If the disease has acquired a serious form, an increase in the submandibular and parotid lymph nodes (on the affected side) is observed, as well as a significant deterioration in the patient’s well-being.
Meanwhile, the most characteristic manifestations of wisdom tooth pericoronitis are:
- swelling of the gums;
- redness of the gums;
- pain in the gum area.
Often, with acute pericoronitis, the swelling is so severe that the patient has difficulty speaking and it becomes difficult to open and close his mouth.
Types of pericoronitis
Depending on the complexity and localization of inflammation, pericoronitis is divided into:
- Spicy.
The initial stage of the disease, which is characterized by pain, hyperemia and swelling of the gums. In case of acute pericoronitis of a wisdom tooth, there is no purulent discharge and the general condition of the patient does not suffer. With proper timely treatment, this type of disease disappears in 3-5 days.
- Ulcerative.
The disease develops against the background of epithelium damaged by fusospirochetes. A characteristic symptom of ulcerative pericoronitis is the appearance of a necrotic rim along the edges of the gums. Small ulcers form on the mucous membrane. When plaque is removed from the gum surface, bleeding begins.
- Purulent
Pericoronitis, as a rule, occurs in a subacute form and is manifested by severe pain. Pus is released from the source of inflammation, and the temperature rises. In the absence of timely treatment, the disease can provoke the formation of abscesses, phlegmon and periostitis.
- Posteriormolar.
The disease develops when molars erupt incorrectly. A gingival hood forms, which then becomes infected due to the active proliferation of bacteria.
Removal Features
As a rule, operations to remove third molars are always considered difficult, since these are the teeth that usually cause more problems. The operation can be simple, provided that the “figure eight” is located on the upper jaw and does not have pronounced developmental abnormalities. In all other cases (as well as in situations where the tooth is in the upper jaw, but has strong, curved and branched roots), the operation is considered complex and must be performed by a qualified dental surgeon.
Before performing an intervention, the doctor determines possible contraindications for a particular patient, examines an x-ray of the problem area and determines the optimal tactics for the operation. The duration of the procedure ranges from 1-10 minutes for simple removal and up to 20-120 minutes for complex removal, requiring a series of manipulations and suturing of the hole.
Treatment of pericoronitis
Treatment by a dentist and surgeon should be aimed not only at eliminating the symptoms of the disease, but also at eliminating its causes. As a rule, for wisdom tooth pericoronitis, drug therapy and surgical intervention are used.
Drug treatment is the fight against microorganisms that caused the development of the infectious process. The doctor also prescribes medications that reduce pain and inflammation symptoms.
As a rule, the following groups of drugs are used to treat wisdom tooth pericoronitis:
- antiseptics, mouth rinses. The products reduce the microbial load and wash away bacterial and purulent particles.
- nonsteroidal anti-inflammatory drugs, for example, Ibuprofen, Ketorolac.
- antimicrobial, broad-spectrum anti-inflammatory drugs, for example, Amoxicillin, Amoxiclav, Azithromycin.
Surgical intervention for wisdom tooth pericoronitis usually involves excision (removal) of the gum hood over the wisdom tooth. This tactic is chosen in case of frequent relapses of the disease, pronounced pain syndrome, and spread of the purulent process to surrounding tissues. When an area of soft tissue is excised above the surface of the crown, plaque stops accumulating, which prevents infection and progression of the disease.
Excision of the hood takes no more than 10-15 minutes and is performed under local anesthesia.
If removing the hood and conservative treatment does not lead to an improvement in the condition, it is possible to remove the wisdom tooth. Removal is also carried out in case of incorrect tooth position or significant deviation of the “figure eight” from its physiological axis. In rare cases, not only the wisdom tooth is removed, but also part of the bone tissue. After removal, in almost 100% of cases, the patient recovers completely.
It is worth noting that many patients often insist on maintaining the “eight”. Many believe that in the future a wisdom tooth may be useful if prosthetics are needed. However, such an opinion is wrong. The wisdom tooth is located the farthest away and does not bear a significant functional load, taking only 2% of the total load on the dentition. When installing a crown, the wisdom tooth will not withstand the pressure, and the prosthesis will have to be replaced very soon.
After removal of a recumbent wisdom tooth
While the anesthesia is in effect, the patient does not feel pain. But when the effect of the drug wears off, sensitivity gradually returns, and the person begins to feel pain. This pain is physiological, because the doctor cut the tissue, touched the bone, and the nerve endings were damaged. After a few days, the sensations finally subside. The following symptoms are possible:
- Mild hyperthermia;
- General malaise, weakness;
- Development of edema;
- Bleeding in the socket area.
Sometimes bleeding from the site of tooth extraction frightens a person; this is a natural reaction. The patient always thinks that he has lost more blood than actually happened. Sometimes the phenomenon continues for hours and usually stops completely by the evening. But if the nature of the bleeding remains unchanged throughout the day, the pain increases, and purulent spots appear in the socket, then the discomfort cannot be tolerated. This requires quick response measures to stop the developed inflammatory process.
Rinse
Special rinses will help relieve pain and swelling at home. However, such treatment is symptomatic. If inflammation progresses, in no case should you limit yourself to rinsing only.
The treatment for inflammation recommended by dentists is ASEPTA Active mouth rinse. This unique two-component product with a combination of “chlorhexidine + benzydamine” has an antimicrobial, anti-inflammatory effect and provides an immediate analgesic effect.
To eliminate inflammation and relieve discomfort during wisdom tooth pericoronitis, it is possible to use such medicinal herbs as:
- chamomile;
- sage;
- calendula.
Possible consequences
Pericoronitis of the wisdom tooth in the lower jaw is a rather dangerous disease, ignoring which can lead to very unpleasant consequences.
Possible complications of the disease may be:
- abscesses, phlegmon of the vestibule of the mouth, buccal area;
- periostitis;
- osteomyelitis of the jaw;
- periodontitis;
- ulcerative stomatitis;
- actinomycosis;
- paradental cysts.
In addition, if wisdom tooth pericoronitis affects the lymph nodes, if inflammation develops, the lymphatic system may become a victim of infection.
And, of course, without proper treatment, the disease can become chronic and periodically “harass” the patient with unpleasant symptoms. Inflammation can spread to neighboring healthy teeth. Therefore, in order to avoid complications, treatment of the disease should be carried out as early as possible.
If you do not remove the dystopic figure eight, there is a danger of complications
If the third molar grows at an angle, it poses a threat to the health of other teeth, so this situation requires timely medical intervention. It also creates a constant traumatic effect on the mucous membrane, which can soon provoke inflammation. If you continue to ignore the symptoms, it can lead to even more serious problems:
- purulent lesions - an open wound appears at the site of eruption, and if pathogenic microorganisms get into it, this can lead to inflammation and purulent processes. As a result, there will be a risk of developing periodontitis, abscesses and even osteomyelitis,
- bleeding - if the tooth lies deep enough and horizontally, then during its growth the vessels will be injured, which can easily provoke serious bleeding,
- curvature of the bite - figure eights displace their “neighbors”, which soon leads to deformation of the occlusion as a whole,
- There are numerous abrasions and scratches on the mucous membrane - the result of constant injury to soft tissues and a direct prerequisite for infection.
Horizontal tooth growth brings many complications.
One of the most severe complications is the development of oncology. This happens very rarely, but experts still do not exclude the possibility of this sad scenario developing. The risk in this case is due to the constant traumatic effect on the cheek from the inside, which in the future can lead to dangerous structural changes in the mucosa and the appearance of malignant neoplasms.
Prevention
As you know, it is easier to prevent a disease than to treat it. The main disease prevention measures are:
- annual dental examinations;
- timely diagnosis and treatment of impacted molars;
- maintaining oral hygiene;
- timely treatment of caries, gingivitis, periodontitis and other dental diseases;
- Regular (once every six months) professional teeth cleaning in a dental clinic.
Remember: pericoronitis without proper treatment can cause very serious complications. Therefore, if you suspect inflammation, do not delay your visit to the dentist. The doctor will help you cope with unpleasant sensations in a matter of days and prevent the development of the disease.
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
- The use of drugs from the Asepta line in the complex treatment of inflammatory periodontal diseases (N.V. Berezina E.N. Silantyeva S.M. Krivonos, Kazan State Medical Academy. Kazan.) N.V. BEREZINA, E.N. SILANTIEVA, S.M. KRIVONOS Kazan State Medical Academy