Author:
- Elena Vitalievna Naumova, otolaryngologist, leading doctor of the clinic
3.00 (Votes: 10)
Acute tonsillitis with purulent exudate is considered the most common infection.
The disease occurs in both adults and children due to the entry of pathogenic microbes and bacteria into the oral cavity. It is not difficult to get a purulent sore throat even in the absence of direct contact with a sick person. Bacteria are spread through contact and airborne transmission, such as by sneezing or coughing in a public place or sharing household items.
Causes of pus and symptoms
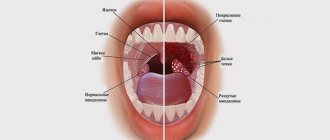
Pus on the tonsils appears in acute tonsillitis or sore throat. The causative agents of the disease and purulent plaque are bacteria.
Tonsils have a barrier and protective effect; when pathogenic microorganisms enter, they do not allow them to pass into the respiratory tract.
Plugs with pus are a symptom, not the cause of the disease; sore throat with complications develops with reduced immunity.
In acute tonsillitis, accompanied by purulent plaque, the following symptoms are observed:
- Pain in the throat that gets worse when swallowing and talking.
- The throat area becomes red and swollen, followed by pus.
- Increased body temperature often reaches 40 degrees. A sore throat causes headache, general weakness and chills.
- Enlarged and painful lymph nodes under the jaw.
Pus is formed with follicular and lacunar tonsillitis, and with the catarrhal form of the disease there are no plugs.
Forms of purulent sore throat
There are two varieties:
- Purulent sore throat, affecting the lacunae of the tonsils. The infection is localized in the upper part of the throat and does not penetrate deeper. Purulent deposits are easily separated with a spatula.
- Purulent tonsillitis affecting the lymph nodes. The infection penetrates deeper and affects the lymphoid apparatus. Purulent exudate cannot be separated manually. The condition is extremely serious and threatens the formation of a peritonsillar abscess. Urgent medical attention and hospitalization are required.
Advantages and disadvantages of the pus removal procedure
It is necessary to remove pus from the tonsils in severe cases of the disease in a medical facility. Ulcers are containers where there is a large accumulation of various bacteria. After two days of antibiotic therapy, pathogenic microorganisms are destroyed. When the infection is defeated, the pus stops secreting, and the plugs disappear after 3–4 days.
If you do not remove the inflammation from a purulent sore throat, but simply start fighting the traffic jams, the patient’s condition will only worsen. There is a risk of reappearance of purulent discharge on the tonsils, and irritation and inflammation of the mucous membrane will cause an increase in temperature.
The situation will lead to the spread of infection and damage to the mucous membrane. When you cleanse your throat with hard objects on your own, the pus seeps even deeper.
Causes of sore throat (acute tonsillitis)
The accumulation of purulent “sacs” in the tonsils occurs for various reasons. The main causative agents of tonsillitis are streptococci, but viral and fungal pathogens, staphylococci and pneumococci are also found. If the body is healthy, then the infection will not develop, but the following factors can aggravate the condition:
- Injuries to the tonsils and nasopharynx.
- Weak immunity.
- Chronic diseases of the ear, nose and throat, for example, stomatitis, caries, rhinitis, etc. foci of infection increase the proliferation of pathogens.
- Local and general hypothermia, for example, eating ice cream or drinking cold water.
- Autumn-spring vitamin deficiency.
The pathogenic factor penetrates deep into the tissues of the tonsils, forming a focus of infection.
Step-by-step procedure for removing pus from tonsils
The procedure for getting rid of purulent plaque is simple; its difficulty lies in carrying out the manipulation yourself in compliance with all sanitary standards.
How to deal with ulcers at home:
- Use a hard object to press on the area near the plug; a white liquid will appear on its surface.
- The object must be surgical tweezers, a pencil, a teaspoon handle.
- The manipulation is carried out near a mirror in a illuminated place. A person's hands must be completely free.
- It is necessary to disinfect the item by wiping it with alcohol.
- Tweezers or a spatula should be wrapped in a piece of sterile bandage, after moistening it in Furacilin or another antibacterial agent.
- The object is brought to the throat carefully, because the abscess is removed with the slightest pressure.
After the manipulation, it is necessary to clean the tonsils from any remaining pus, so the throat is gargled with chamomile decoction, saline solution, and Furacilin. If you use hydrogen peroxide, then after the procedure you will also have to wash off this medication.
Medicinal preparations for rinsing
It is easy to get rid of purulent plugs with plain water, but it is recommended to use medications to rinse the throat. This remedy will remove plaque, destroy the causative agent of the disease and improve the condition of the mucous membrane during a sore throat.
There are several common preparations for rinsing with purulent sore throat.
- Potassium permanganate. To prepare the liquid, you will need to dissolve a couple of potassium permanganate crystals in 200 ml of warm water. The dosage is calculated for one rinse. It is recommended to filter the solution so that the grains do not scratch the already affected throat. Rinsing is carried out 4 times a day.
- Saline solution. For a sore throat, this is the most popular remedy; to prepare it, you need to dilute 1 tsp in 200 ml of warm water. soda and salt. For a quick effect, add a couple of drops of iodine to the liquid. The procedure is carried out 4 times a day, combined with other medications.
- Boric acid. To prepare the solution, pour 2.5 grams of 1% dry product into a glass of warm water. The liquid is used for rinsing with ulcers 3 to 5 times a day.
- Chlorophyllipt. The natural-based drug has an anti-inflammatory, immunostimulating and restorative effect. Add 1 tsp to a glass of warm water. medical product. It is necessary to gargle three times a day; it perfectly removes surface deposits.
- Furacilin. The drug tablet is crushed and dissolved in a glass of warm water. The product is used 2 to 4 times a day.
- Chlorhexidine. The drug has an antiseptic effect. Before using it, it is recommended to gargle with warm boiled water and brush your teeth. For the procedure, take a 0.05% solution, which you need to gargle for 30 seconds and spit it out.
It is prohibited to use different medications for purulent sore throat without first consulting a doctor. Some products can be harmful to the body. Inhalipt, due to its increased viscosity, slows down the discharge of pus.
Treatment of purulent sore throat
Purulent tonsillitis threatens serious complications from the heart, kidneys, joints and soft tissues of the neck if therapy is chosen incorrectly or treatment is started late. It is for this reason that it is important to immediately consult a doctor when the first signs of a sore throat appear.
The basic treatment regimen for acute tonsillitis with purulent exudate:
- Taking antibiotics of the penicillin group or the macrolide group. You can't do without them. General and local remedies are prescribed. Antibiotics kill pathogenic microflora and after a few days the production of pus stops, blood circulation in the tonsils is restored.
- Taking anti-inflammatory lozenges, lozenges, lozenges.
- Gargling and irrigating the throat with different solutions every hour.
- Use of local antiseptics in the form of a spray.
- Taking antipyretic drugs.
- Vitamin therapy and taking immunomodulators.
The principle of treatment of acute tonsillitis in children is similar, the only differences are in the dosage of medications. The patient needs to observe strict bed rest, talk less and gargle more often.
If the prescribed drug therapy does not have positive dynamics within several days, the patient continues treatment in the hospital.
Due to the presence of purulent plaque on the palatine tonsils, eating is difficult or completely impossible, so you can eat only pureed and liquid food, and also drink a lot of warm water to relieve symptoms of intoxication.
Traditional methods of treatment
There are many proven ways to treat purulent sore throat with homemade products and plants.
Chamomile and calendula decoction. To prepare the medicine, you will need to pour 2 tbsp into a small saucepan. l. herbs, pour 1 liter of boiling water over it and simmer the mixture over low heat for half an hour. The infusion cools for 2–3 hours, after which you need to start gargling.
Kalanchoe and aloe. Plants have anti-inflammatory properties. For the medicine you will need their leaves, which are more than three years old. The greens are crushed and squeezed, and the resulting juice is diluted with 1 glass of water. This natural product relieves swelling.
Cautions and Limitations
When treating purulent plugs on the tonsils, you should pay special attention to some restrictions. If pus remains on the tonsils when gargling, there is no way to forcefully get rid of it. Several manipulations with rinsing will help remove purulent plugs without damaging the mucous membrane. During manipulation, it is easy to damage the surface of the shell.
Purulent tonsillitis is treated only under the supervision of a physician. Therapy includes a set of rinses, medication, and traditional medicine recipes.
Severe bacterial tonsillitis is accompanied by the accumulation of pus on the tonsils. But the amount of these deposits and their prevalence do not in any way affect the patient’s condition; the main symptoms of the disease are caused by the inflammatory process.
With the help of properly prescribed therapy, the pus will disappear on its own in a few days. Complex treatment, including the use of rinsing, rubbing and other methods, will help to achieve a speedy recovery for a person.
How to remove pus?
Pus is removed using several methods. For this purpose, various drugs are used. But not only they will help stop the progression of the disease. To help get rid of ulcers on the tonsils:
- surgical intervention for removal;
- physiotherapeutic treatment using laser and magnet.
Surgical treatment is the removal of tonsils. Such therapy is carried out only if the disease has become chronic.
If a person’s condition is constantly deteriorating, and it is not possible to get rid of traffic jams, then surgery will help correct the situation.
But surgical intervention is rarely performed, since even tonsils that are altered and damaged by bacteria protect the body from viruses and pathogenic microorganisms. But on the other hand, this is a source of infection in the body; it can cause endocarditis or glomerular nephritis.
Treatment using physiotherapeutic procedures is carried out to stabilize the patient's condition.
Most often prescribed:
- UHF.
- Treatment with laser.
- Magnetic therapy.
Physiotherapeutic procedures will significantly strengthen the effect of medications. But their implementation is advisable only after the inflammatory process has been completely stopped.
Doctors' recommendations
Therapy for sore throat necessarily includes gargling; if the deposits are localized deep in the crypts, it is better not to touch them so as not to provoke the development of complications. If it is necessary to remove accumulations, only a specialist in a medical institution can do this.
Opening and squeezing out purulent follicles on your own is very dangerous. At home, you cannot completely remove all the contents and clear your throat well. As a result of damage to the integrity of the mucous membrane, an unprotected wound surface is formed in the throat. It is an open gate for pathogenic bacteria to enter.
There is a high risk of developing an abscess, especially when pus penetrates deep into the tissue. Its occurrence can provoke a severe deterioration in the patient’s well-being. And the only method of getting rid of the problem is surgical intervention - opening the abscess.
Treatment of angina should be comprehensive and carried out under the supervision of a specialist. You should listen to your doctor's recommendations. This will help speed up the patient’s recovery and prevent the development of complications and side effects.
We have all encountered more than once the problem of treating a sore throat, especially in childhood. And each of us has memories left in our memory, like a fragment of a picture from a movie, a warm bed, tea with raspberries and an anxious mother who is watching you with pain in her heart, putting a cold towel to her forehead, trying to reduce the fever, because... Typically, such infectious and inflammatory diseases of the oral cavity are accompanied by high fever. So what causes a sore throat and how can you cope with the consequences of this disease so as not to provoke complications.
According to medical statistics, infectious and inflammatory diseases of the mouth and throat account for an average of 30% of the total number of diseases of the ENT organs. The main causative agents of this kind of throat infection are bacteria, the so-called pathogenic microorganisms staphylococci and streptococci, which can easily get on the mucous membrane of the throat and provoke inflammation, especially in children, who are traditionally included in the “risk group”. But in addition to pathogens of a bacterial nature, yeast-like fungi of the Candida albicans group and mold fungi of the genus Aspirgillius can also complicate the course of throat diseases, which are difficult to treat and require, first of all, diagnostic measures to identify the causative agent of the infection, both bacterial and infectious in nature, that provoked inflammation, and selection of a treatment regimen that can suppress two pathogens at the same time. And diseases such as pharyngomycosis and laryngomycosis are among the socially significant diseases, because require an individual approach to therapy.
Usually, the presence of an acceptable amount of opportunistic microorganisms produced on the mucous membranes of the nasopharynx, larynx and throat serves as a natural barrier against external infection entering the body, but as a result of exposure to external and internal factors, their volume may increase, and due to additional infection by bacteria and pathogenic microorganisms , diseases of an infectious and bacterial nature can develop, including those aggravated by a fungal infection, such as mycosis of the throat or candidiasis.
It should be noted that fungi of the genus Candida are quite widespread and, as a result, the possibility of getting this infection in public places through shared objects, food, including by airborne droplets is quite high. In addition, the development of this type of infection can be caused by such reasons as uncontrolled and long-term use of antibiotics without special indications, less often, disruption of hormonal levels and the endocrine system, reduced immunity, frequent diseases of a viral nature, childhood, incl. and incorrectly selected therapy for ENT diseases.
Fungal infections of the throat differ from the symptoms of ordinary sore throat of a bacterial nature in the appearance of plaque, which resembles cottage cheese. It is easy to remove, but underneath there is an inflamed mucous membrane, with redness and ulcers. And if a fungal throat infection is caused by fungi of the genus Aspirgillius, then such plaque is quite difficult to remove and has a yellowish tint. It should be noted that the localization of a fungal infection in the mouth and throat is also characterized by the manifestation of symptoms of a common sore throat.
It is quite difficult to detect fungus in the mouth and throat at an early stage, because... at the beginning of infection it usually does not appear, only as the colonies increase. Characteristic symptoms begin to appear gradually, in the form of discomfort, soreness, burning and dryness in the throat, and pain during swallowing. In addition, there is a presence of white plaque in the larynx, tonsils, tonsils and tongue, as well as the appearance of erosive surfaces in the form of ulcers and cracks in the mucous membrane of the throat. Traditionally, the temperature rises, headaches appear, swelling of the nasopharyngeal mucosa occurs, as well as characteristic symptoms of general poisoning and intoxication.
In children, the course of fungal tonsillitis is much more severe than in adults, because In childhood, the phenomena of intoxication in the body and pain syndrome are especially pronounced. The child becomes weakened, more capricious, and refuses to eat. In addition, when removing plaque from the mucous membranes of children, the delicate skin may be injured, and sometimes minor bleeding may occur. Also, in children there is a high probability of dysbiosis and diarrhea, due to the fact that yeast-like fungi of the genus Candida can move into the intestinal tract and provoke intoxication and characteristic symptoms of poisoning.
The initial diagnosis for the presence of fungi in the throat can first be carried out independently by examining the mouth and throat for the presence of white plaque. But it is important to remember that only a doctor can make a correct diagnosis, because... Only with the help of laboratory diagnostics can one identify the pathogen that has caused infectious and inflammatory processes in the nasopharynx and oral cavity and select the necessary treatment regimen for this disease.
Instrumental research or laboratory diagnostics includes the following studies:
1. Laboratory mycological research - analysis of biomaterial (smear from the throat), provides the most accurate determination of the pathogens that caused a fungal infection of the throat.
2. A skin test with fungal allergens is carried out by introducing a fungal allegory test under the skin. This research method is necessary to establish the most accurate diagnosis and also to identify the chronic stage of the disease.
3. An immunological test is carried out to detect antibodies to the fungus in the blood.
These studies are the most informative and will allow the specialist to choose the right tactics for treating emerging lesions of the throat mucosa with fungal colonies.
After the doctor has made the correct diagnosis and identified the causative agent of the infection, the next step towards recovery is treatment of the fungal infection. The main goal is to get rid of a large number of pathogens in the throat, restore microflora, the integrity of the mucous membranes and strengthen the immune system. Treatment of fungal tonsillitis is carried out comprehensively, combining traditional medicinal methods in conjunction with a balanced diet. First of all, antifungal agents are prescribed, and if this therapy does not give the desired effect, antibiotics are prescribed. The course of treatment can last up to 2 weeks, but in acute forms of the disease it is necessary to prescribe additional therapy in the form of vitamins, antiallergic agents and probiotics containing bifidobacteria and lactobacilli to restore normal gastrointestinal microflora. In addition, local antiseptics are additionally prescribed.
One of these drugs, which has proven itself in the treatment of ENT diseases, including purulent-inflammatory infections of the oral cavity, nasopharynx and throat, is the modern anti-inflammatory drug of plant origin Abisil, created on the basis of natural terpenoids of Siberian fir. The drug has pronounced anti-inflammatory, antibacterial, analgesic, wound-healing, and anti-exudative effects. It should be especially noted that microbiological studies of the drug Abisil revealed a wide range of antibacterial activity against gram-positive and gram-negative strains and various types of pathogenic microbes, often causing purulent-inflammatory diseases. Abisil is especially sensitive to staphylococci and streptococci, which are the main pathogens for throat diseases, in particular purulent sore throat. In addition, the drug was found to have antifungal activity against yeast-like fungi of the genus Candida and mold fungi Aspirgillus. But the most valuable thing about it is that microorganisms do not become resistant to the drug, and therefore it can also be used in complex cases when inflammation is caused by antibiotic-resistant microflora. Possessing a complex and multidirectional effect, Abisil helps to get rid of purulent sore throat in a short time, including sore throat aggravated by a fungal infection. And in most cases, when traditional therapy for the treatment of fungal tonsillitis, including the simultaneous use of antibiotics and antimycotics, does not give the desired effect, Abisil therapy acts as an alternative to antibiotic therapy and shows a positive effect in the treatment of these pathologies. In addition, Abisil helps restore the activation of the protective functions of the mucous membrane and restores the balance of the microflora of the nasopharynx, in contrast to local synthetic antiseptics, which suppress both pathogenic and conditionally pathogenic microflora of the mucous membrane of the nasopharynx and throat.
The drug does not accumulate in the body, does not have teratogenic or embryotoxic effects and therefore can be used in all age groups, incl. and in children, and is indicated for use in the treatment of purulent-inflammatory throat infections. But in any case, to provide effective assistance and prescribe therapy for fungal infections of the throat, it is necessary to consult a doctor and his observation during the treatment. It should be noted that treatment with Abisil is simple and accessible. For tonsillitis, laryngitis, pharyngitis, it is recommended to irrigate the mucous membranes of the mouth with the drug 2-3 times a day after meals. This can be done using a pipette or a syringe through a special nozzle, distributing Abisil in an amount of 1-2 ml to the area of the palatine tonsils and adjacent palatine arches, larynx and pharynx. In this case, it is additionally necessary to drip 2-3 drops of the drug into the nose. The duration of treatment is 1-3 weeks. In case of chronic disease, the course of treatment can be repeated after 1-2 months. After the procedure, it is not recommended to eat, drink or rinse your mouth for 3-4 hours. For fungal infections of the oral cavity, it is recommended to treat the affected areas of the oral mucosa 3-4 times a day with a cotton swab moistened with the drug. In addition, rubbing the drug Abisil into the front of the neck, into the area of the submandibular and cervical lymph nodes is also effective. In rare cases, a short-term burning sensation may occur at the site of application of the drug, but it quickly passes. Combining the drug with other external agents is not recommended.
Another component of a full fight against fungal infections of the mouth and throat is a balanced diet, which additionally helps to get rid of mycosis. The fact is that fungi can feed on the foods that we eat and therefore, when forming a diet for the treatment of fungal sore throat, we should exclude foods that can provoke the growth of fungi, thus depriving them of additional nutrition. First of all, you should exclude alcohol, sugar, baked goods, baked goods, sweets, condensed milk, jams and preserves, dairy products, as well as canned foods containing vinegar. And the following foods must be included in the diet: meat, fish, eggs, cereals, legumes, fresh vegetables and herbs, garlic, spices, mineral water and tea.
You should pay attention to the fact that with improper therapy or neglect of the prescribed treatment by a doctor, complications of the disease can be provoked, in which the mucous membrane of the throat is destroyed and open wounds and ulcers appear on it, into which infection can re-enter and provoke secondary infection in the form of bacterial inflammation . Repeated inflammation is characterized by the appearance of abscesses and abscesses of the larynx. In addition, the development of fungi in the body can also cause a reaction in the form of an allergy, and most often, mycotic eczema can occur, which manifests itself in the form of peeling and the occurrence of inflammation and wounds on the skin. Another complication may be the occurrence of recurrent tonsillitis, which can occur frequently, once every 1-1.5 months, up to 10-12 times a year, and this is associated with the life cycle of the fungus.
What preventive measures must be taken so that the fungus in the throat does not develop further and does not develop into a chronic disease with frequent relapses. First of all, it is necessary to monitor hygiene and cleanliness of the oral cavity, and avoid contact with infected people. Take antibiotics only as prescribed by a doctor, do not self-medicate and do not take antibiotics longer than the prescribed course. Make it a rule to visit the dentist for a preventative examination of the oral cavity and begin treating the disease immediately, without delaying it for later, and do not forget to strengthen your immune system. The most important rule in the treatment of fungal infections of the oral cavity and larynx is to identify the cause of the disease, eliminate the pathogen and adhere to the therapy prescribed by the doctor and a set of preventive measures so that possible relapses and complications do not arise in the future.