Fracture of the upper jaw - symptoms and treatment
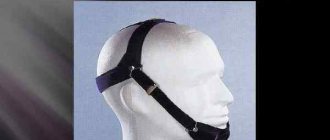
When providing first aid to the patient, it is necessary to stop the bleeding and prevent aspiration (penetration into the respiratory tract) of blood and vomit. If the lower jaw is not damaged and there are a sufficient number of teeth on both jaws, it is necessary to apply a sling-like bandage, pressing the lower jaw to the upper jaw, or perform immobilization (immobilization) with a rigid chin sling [4].
If there is a risk of respiratory failure, immediate insertion of an airway is required to maintain the conductivity of the airways [1]. In addition, it is necessary to provide pain relief and quickly transport the patient to specialized medical institutions. The most important thing at this stage is to preserve the life and health of the patient.
There are many methods of non-surgical treatment of fractures of the upper jaw, for example, various types of bandages and external fixations, which are currently practically not used.
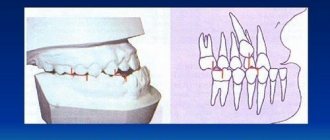
The most common method of orthopedic treatment of fractures is bimaxillary splinting - the application of splints and brackets to the dentition with reposition of fragments and fixation of the bite in the patient’s usual position. This method is conservative and low-traumatic, but in some cases it does not allow obtaining good fixation of fragments of the upper jaw, especially in high and complex fractures. On average, fractures of the upper jaw require immobilization and limitation of chewing load for a period of 4-5 weeks.
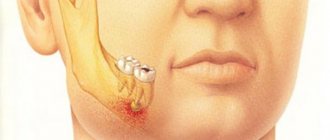
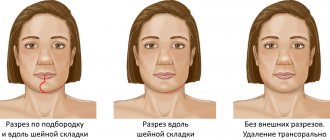
The most modern and adequate treatment method at the moment is osteosynthesis (fixation with titanium bone structures) of fractures of the upper jaw. This is a surgical procedure performed through intraoral incisions. With this treatment option, it is possible to accurately compare and fix the fragments to create conditions for their fusion [7].
In the treatment of high fractures, a coronal approach is also used, which allows for cosmetic and wide access to the bones of the entire midface and orbits [5]. Timely implementation of osteosynthesis allows you to prevent late postoperative complications, facilitate the patient’s rehabilitation and speed up recovery.
Fractures with gross violations of the integrity of the upper jaw and significant displacement of fragments towards the pharynx are recommended to be treated surgically. There is no clear opinion regarding other types of fractures - tactics are dictated by the patient’s condition and the specific clinical situation.
It is worth noting that it is very important to constantly wear intermaxillary fixation for tight contact of fragments and to prevent their mobility, especially under the influence of chewing load [9]. High-quality oral hygiene and patient observation by an oral and maxillofacial surgeon are also necessary.
Recovery from fractures takes from four to six weeks, depending on the nature of the fracture, the characteristics of the patient’s body and the method of treatment.
Patients with fractures of the upper jaw should eat liquid food in the early stages, and soft food in the later stages. Eating hard foods and active chewing should be limited. Other recommendations are given based on general somatic and neurological disorders (bed rest, etc.).
News
Providing first aid for injuries to the teeth or jaw.
The most common injuries to the dental system include various dental injuries, as well as closed or open fractures, bruises, and jaw dislocations. All of them require immediate treatment, since, unlike damage to other bones of the human body, their healing occurs quite problematically and over a long period and entails a high level of psychological discomfort and negative consequences. Trauma to the lower jaw is one of the most unpleasant injuries to the skeletal system.
Tooth injury
Physical damage to a tooth is divided into cracks, bruises, dislocations with displacement (partial or complete) of the tooth around its axis or to the side, fractures (of the crown or root), and these damages can be combined. Mostly, such injuries occur due to a strong blow to the jaw, but sometimes too hard food (nuts, bones, caramel, etc.) can damage the integrity of the tooth.
Signs of tooth injury:
feeling of acute pain in the area of the damaged tooth;
the position and/or size of the tooth has changed and this is noticeable to the naked eye;
in the area of the damaged tooth, as well as surrounding tissues, the gums are red or swollen;
bleeding began (in case of severe injury);
the tooth became mobile.
Of course, a microcrack in the root of a tooth may not manifest itself in this way, but over time, pathogenic bacteria will penetrate through the resulting gap into the tooth, which will subsequently lead to pulpitis (inflammation of the nerve endings of the tooth).
First aid for tooth damage
Services for the treatment of dental injuries are provided by a dentist in accordance with each specific case. In case of dislocation, splinting of teeth can be carried out, when a mobile tooth is fixed to adjacent healthy teeth by applying a medical rubber splint; when a tooth root is fractured, it is partially or completely removed; In case of fractures of the crown part of the tooth, restoration or microprosthetics is performed.
Jaw fracture
A jaw fracture is a serious injury to the jaw apparatus, which can lead to serious consequences. These include: concussion, disorders of chewing and swallowing functions, meningitis, etc.
A jaw fracture can look different: with or without a violation of the integrity of the cheek or other nearby tissues (an open or closed fracture, respectively); with or without displacement (respectively, complete or incomplete fracture).
Signs of a jaw fracture:
bleeding from the wound (with an open fracture);
acute unbearable pain, especially when moving the jaws;
general malaise, nausea, fainting;
unusual jaw mobility;
hematomas on the face;
violation of respiratory, swallowing and speech functions;
retraction of the tongue (with a fracture of the lower jaw).
First aid for a broken jaw
Immediately after a jaw fracture occurs, the victim must be given first aid, which includes: fixing the broken jaw immobile with a bandage, removing foreign bodies from the mouth (if any), fixing the tongue (if breathing and swallowing are difficult), by applying a cold compress ( for example, an ice pack), ensuring complete rest for the patient, calling an ambulance for transportation to the clinic.
First aid for dental trauma in children
When a child goes to the dentist with a tooth injury, the doctor first of all evaluates the overall clinical picture, finds out the date, time, and causes of the injury, and then proceeds to a thorough examination of the damaged tooth and surrounding tissues. In any case, an x-ray examination is necessary. If a baby tooth is injured, it is important during treatment not to damage the permanent tooth germ. When a permanent tooth is injured, the doctor’s main task is to preserve it.
Treatment of a jaw fracture
Therapy for injury should be carried out only by doctors, and the sooner qualified medical care is provided, the lower the risk of complications. Treatment of a jaw fracture may include the following manipulations:
- if there is a wound (rupture of soft tissues, mucous membranes), then first the bleeding stops and disinfection measures are carried out;
- manual comparison of bone fragments, giving the correct shape to the damaged jaw;
- A splint must be applied - if the jaw is fractured, it must be completely immobilized for at least one month.
Additionally, painkillers and anti-inflammatory therapy are prescribed. If a fracture of the jaw processes is diagnosed, then, most likely, surgical intervention will be prescribed, which involves the implantation of specific metal plates. Your doctor will tell you more about the operation during your consultation. Sign up on our website Dobrobut.com.
Rehabilitation after a jaw fracture includes physiotherapy, massage and facial exercises. Patients often have to relearn how to chew and speak without distorting sounds.
External means
After the cast is removed, the patient may experience pain and swelling for a long time. To get rid of these unpleasant manifestations of injury, the doctor may prescribe ointments and gels that relieve discomfort. Such drugs have important effects:
- analgesic – relieves pain, improves motor abilities;
- anti-inflammatory – improves tissue condition, relieves inflammation, redness, swelling;
- muscle relaxant – promotes muscle relaxation, relieves excessive tone, improves the effect of painkillers;
- regenerating – stimulates restoration processes, activates metabolism in damaged tissues.
External medications have much less negative effects than oral medications. Therefore, many doctors prefer ointments and gels with local action.
Recovery in a supine position
For fractures of the extremities, recovery must begin when the patient is in a supine position and cannot stand. Only an early start of rehabilitation allows you to achieve maximum results. Otherwise, the muscles become inactive and weaken, causing the bones to heal incorrectly.
The complex of therapeutic exercises for a bedridden patient includes:
- shoulder lifts;
- lifting on the forearms;
- hand rotations;
- flexion, extension, pulling the healthy leg to the chest;
- contraction and relaxation of the muscles of the legs and arms;
- raising, abducting, bringing the injured limb to the body.
At the initial stage, these exercises should be performed under the supervision of a specialist and with his help. Over time, the patient will be able to perform gymnastics independently.
Massage
Therapeutic massage after fractures involves the use of specific techniques:
- rubbing – active movements improve blood circulation and reduce pain;
- kneading – restore muscle tone, improve tendon mobility;
- stroking – light stroking movements relax muscles, improve microcirculation;
- effleurage - improves blood flow and increases muscle contractility.
The massage therapist selects a treatment course taking into account the characteristics of the injury and the exact location of the fracture. A course of therapeutic massage helps to avoid muscle atrophy and weakness, improve mobility, relieve swelling and pain.
Fracture of the lower jaw - features
This type of injury has some features:
- a fracture with displacement of bone fragments or the entire jaw is called complete;
- if the injury is of an open type, then not only the mucous membrane of the oral cavity ruptures, but also the soft tissues of the face;
- It is extremely rare that a comminuted fracture is diagnosed because it requires too much force.
A fracture of the lower jaw is characterized by the following signs:
- pronounced asymmetry of the face, which is formed due to swelling and hemorrhage in the soft tissues at the site of injury;
- acute pain when touching any part of the lower jaw, inability to talk or chew;
- mobility of fragments, if any;
- a radical change in the bite - the lower jaw may be too forward or, conversely, “retracted” deeper.
Anyone can provide first aid for the injury in question - you need to apply a bandage (place any straight object, such as a ruler, between the teeth) so that the damaged part of the jaw is motionless. If there is bleeding, it must be stopped by applying something cold, treating with hydrogen peroxide and other classical methods. Then all that remains is to wait for the ambulance team to arrive.
Working with gait
As part of rehabilitation after a leg injury, it is necessary to work on restoring gait. One of the most effective options is exercise on an exercise bike, to which the patient must be allowed by a doctor if there are no contraindications.
In addition to training on the simulator, it is also important to perform special exercises:
- grab a small object with your toes and hold it suspended;
- roll the ball with the foot of the injured limb;
- roll from toes to heels and back;
- walk backwards, sideways.
Classes should be continued until the patient’s motor functions are completely restored and swelling and pain go away.
Damage to the maxillofacial area
The development of surgical treatment methods , especially for neoplasms of the maxillofacial area, has required widespread use of orthopedic interventions in the surgical and postoperative period. Radical treatment of malignant neoplasms of the maxillofacial region improves survival rates. After surgical interventions, serious consequences remain in the form of extensive defects of the jaws and face. Severe anatomical and functional disorders that disfigure the face cause painful psychological suffering to patients.
Very often, reconstructive surgery alone is ineffective. The tasks of restoring the patient's face, chewing, swallowing functions and returning him to work, as well as to perform other important social functions, as a rule, require the use of orthopedic treatment methods. Therefore, the joint work of dentists - a surgeon and an orthopedist - comes to the fore in the complex of rehabilitation measures.
There are certain contraindications to the use of surgical methods for treating jaw fractures and performing operations on the face. Usually this is the presence in patients of severe blood diseases, the cardiovascular system, an open form of pulmonary tuberculosis, severe psycho-emotional disorders and other factors. In addition, there are injuries for which surgical treatment is impossible or ineffective. For example, in case of defects of the alveolar process or part of the palate, prosthetics are more effective than surgical restoration. In these cases, the use of orthopedic measures as the main and permanent method of treatment was shown.
The timing of restoration operations varies. Despite the tendency of surgeons to perform the operation as early as possible, a certain amount of time must be allowed when the patient is left with an unrepaired defect or deformity while awaiting surgical treatment or plastic surgery. The duration of this period can be from several months to 1 year or more. For example, reconstructive operations for facial defects after tuberculous lupus are recommended to be carried out after permanent elimination of the process, which is approximately 1 year. In such a situation, orthopedic methods are indicated as the main treatment for this period. During the surgical treatment of patients with injuries to the maxillofacial area, auxiliary tasks often arise: creating support for soft tissues, closing the postoperative wound surface, feeding patients, etc. In these cases, the use of the orthopedic method is indicated as one of the auxiliary measures in complex treatment.
Modern biomechanical studies of methods for fixing fragments of the lower jaw have made it possible to establish that dental splints, in comparison with known on-bone and intraosseous devices, are the fixators that most fully meet the conditions of functional stability of bone fragments. Dental splints should be considered as a complex retainer, consisting of an artificial (splint) and natural (tooth) retainer. Their high fixing abilities are explained by the maximum area of contact of the fixator with the bone due to the surface of the roots of the teeth to which the splint is attached. These data are consistent with the successful results of the widespread use of dental splints by dentists in the treatment of jaw fractures. All this is another justification for the indications for the use of orthopedic devices for the treatment of injuries to the maxillofacial area.
Orthopedic devices, their classification, mechanism of action
Treatment of injuries to the maxillofacial area is carried out using conservative, surgical and combined methods.
The main method of conservative treatment is orthopedic devices. With their help, they solve problems of fixation, reposition of fragments, formation of soft tissues and replacement of defects in the maxillofacial area. In accordance with these tasks (functions), devices are divided into fixing, reducing, forming, replacing and combined. In cases where one device performs several functions, they are called combined.
Based on the place of attachment, the devices are divided into intraoral (unimaxillary, bimaxillary and intermaxillary), extraoral, intra-extraoral (maxillary, mandibular).
According to the design and manufacturing method, orthopedic devices can be divided into standard and individual (non-laboratory and laboratory manufacturing).
Fixing devices
There are many designs of fixing devices. They are the main means of conservative treatment of injuries to the maxillofacial area. Most of them are used in the treatment of jaw fractures and only a few - in bone grafting.
For primary healing of bone fractures, it is necessary to ensure the functional stability of the fragments. The strength of fixation depends on the design of the device and its fixing ability. Considering the orthopedic device as a biotechnical system, it can be divided into two main parts: splinting and actually fixing. The latter ensures the connection of the entire structure of the device with the bone. For example, the splinting part of a dental wire splint consists of a wire bent to the shape of a dental arch and a ligature wire for attaching the wire arch to the teeth. The actual fixing part of the structure is the teeth, which provide connection between the splinting part and the bone. Obviously, the fixing ability of this design will depend on the stability of the connections between the tooth and the bone, the distance of the teeth in relation to the fracture line, the density of the connection of the wire arch to the teeth, the location of the arch on the teeth (at the cutting edge or chewing surface of the teeth, at the equator, at the neck of the teeth) .
With tooth mobility and severe atrophy of the alveolar bone, it is not possible to ensure reliable stability of fragments using dental splints due to the imperfection of the actual fixing part of the device design.
In such cases, the use of periodontal splints is indicated, in which the fixing ability of the structure is enhanced by increasing the area of contact of the splinting part in the form of coverage of the gums and alveolar process. In case of complete loss of teeth, the intra-alveolar part (retainer) of the device is absent; the splint is located on the alveolar processes in the form of a base plate. By connecting the base plates of the upper and lower jaws, a monoblock is obtained. However, the fixing ability of such devices is extremely low.
From a biomechanical point of view, the most optimal design is a soldered wire splint. It is attached to rings or full artificial metal crowns. The good fixing ability of this tire is explained by the reliable, almost motionless connection of all structural elements. The splinting arch is soldered to a ring or to a metal crown, which is fixed to the supporting teeth using phosphate cement. When ligating teeth with an aluminum wire arch, such a reliable connection cannot be achieved. As the splint is used, the tension in the ligature weakens, and the strength of the connection of the splinting arch decreases. The ligature irritates the gingival papilla. In addition, food debris accumulates and rots, which disrupts oral hygiene and leads to periodontal disease. These changes may be one of the causes of complications that arise during orthopedic treatment of jaw fractures. Soldered busbars do not have these disadvantages.
With the introduction of fast-hardening plastics, many different designs of dental splints have appeared. However, in terms of their fixing abilities, they are inferior to soldered splints in a very important parameter - the quality of the connection between the splinting part of the device and the supporting teeth. A gap remains between the surface of the tooth and the plastic, which is a receptacle for food debris and microbes. Long-term use of such tires is contraindicated.
The designs of dental splints are constantly being improved. By introducing actuator loops into a splinting aluminum wire arch, they try to create compression of fragments in the treatment of mandibular fractures.
The real possibility of immobilization with the creation of compression of fragments with a dental splint appeared with the introduction of alloys with a “shape memory” effect. A dental splint on rings or crowns made of wire with thermomechanical “memory” allows not only to strengthen fragments, but also to maintain constant pressure between the ends of the fragments.
Fixing devices used in osteoplastic operations are a dental structure consisting of a system of welded crowns, connecting locking bushings, and rods.
Extraoral apparatuses consist of a chin sling (plaster, plastic, standard or customized) and a head cap (gauze, plaster, standard strips of belt or ribbon). The chin sling is connected to the head cap using a bandage or elastic cord.
Intraoral apparatuses consist of an intraoral part with extraoral levers and a head cap, which are interconnected by elastic traction or rigid fixing devices.
AST. Rehearsal devices
There are one-stage and gradual reposition. One-time reposition is carried out manually, and gradual reposition is carried out using hardware.
In cases where it is not possible to compare the fragments manually, reduction devices are used. The mechanism of their action is based on the principles of traction, pressure on displaced fragments. Reduction devices can be mechanical or functional. Mechanically operating reduction devices consist of 2 parts - supporting and acting. The supporting parts are crowns, mouthguards, rings, base plates, and a head cap.
The active part of the apparatus are devices that develop certain forces: rubber rings, an elastic bracket, screws. In a functionally functioning reduction apparatus, the force of muscle contraction is used to reposition fragments, which is transmitted through guide planes to the fragments, displacing them in the desired direction. A classic example of such a device is the Vankevich tire. With the jaws closed, it also serves as a fixation device for fractures of the lower jaws with toothless fragments.
Forming apparatus
These devices are designed to temporarily maintain the shape of the face, create rigid support, prevent cicatricial changes in soft tissues and their consequences (displacement of fragments due to tightening forces, deformation of the prosthetic bed, etc.). Forming devices are used before and during reconstructive surgical interventions.
The design of the devices can be very diverse depending on the area of damage and its anatomical and physiological characteristics. In the design of the forming apparatus, one can distinguish the forming part and the fixing devices.
Replacement devices (prostheses)
Prostheses used in maxillofacial orthopedics can be divided into dentoalveolar, maxillary, facial, and combined. When resection of the jaws, prostheses are used, which are called post-resection. There are immediate, immediate and remote prosthetics. It is legitimate to divide prostheses into surgical and postoperative.
Dental prosthetics is inextricably linked with maxillofacial prosthetics. Advances in clinical practice, materials science, and technology for manufacturing dentures have a positive impact on the development of maxillofacial prosthetics. For example, methods for restoring dentition defects with solid-cast clasp dentures have found application in the design of resection dentures and dentures restoring dentoalveolar defects.
Replacement devices also include orthopedic devices used for palate defects. This is primarily a protective plate - used for palate plastic surgery; obturators - used for congenital and acquired palate defects.
Combined devices
For reposition, fixation, shaping and replacement, a single design that can reliably solve all problems is advisable. An example of such a design is an apparatus consisting of soldered crowns with levers, fixing locking devices and a forming plate.
Dental, dentoalveolar and jaw prostheses, in addition to their replacement function, often serve as a forming apparatus.
The results of orthopedic treatment of maxillofacial injuries largely depend on the reliability of fixation of the devices.
When solving this problem, you should adhere to the following rules:
- use the preserved natural teeth as support as much as possible, connecting them into blocks, using well-known techniques for splinting teeth;
- make maximum use of the retention properties of alveolar processes, bone fragments, soft tissues, skin, cartilage that limit the defect (for example, the cutaneous-cartilaginous part of the lower nasal passage and part of the soft palate, preserved even after total resections of the upper jaw, serve as a good support for strengthening the prosthesis);
- apply surgical methods to strengthen prostheses and devices in the absence of conditions for their fixation in a conservative way;
- use the head and upper body as a support for orthopedic devices if the possibilities of intraoral fixation have been exhausted;
- use external supports (for example, a system of traction of the upper jaw through blocks with the patient in a horizontal position on the bed).
Clasps, rings, crowns, telescopic crowns, mouthguards, ligature binding, springs, magnets, spectacle frames, sling-shaped bandages, and corsets can be used as fixing devices for maxillofacial devices. The correct selection and application of these devices adequately to clinical situations allows us to achieve success in the orthopedic treatment of injuries to the maxillofacial area.
Orthopedic treatment methods for injuries of the maxillofacial area
Dislocations and fractures of teeth
- Tooth dislocations
Treatment of complete dislocation is combined (tooth replantation followed by fixation), and treatment of incomplete dislocation is conservative. In fresh cases of incomplete dislocation, the tooth is set with the fingers and strengthened in the alveolus, fixing it with a dental splint. As a result of untimely reduction of a dislocation or subluxation, the tooth remains in an incorrect position (rotation around an axis, palatoglossal, vestibular position). In such cases, orthodontic intervention is required.
- Tooth fractures
The previously mentioned factors can also cause tooth fractures. In addition, enamel hypoplasia and dental caries often create conditions for tooth fracture. Root fractures can occur from corrosion of metal pins.
Clinical diagnosis includes: anamnesis, examination of the soft tissues of the lips and cheeks, teeth, manual examination of the teeth, alveolar processes. To clarify the diagnosis and draw up a treatment plan, it is necessary to conduct x-ray studies of the alveolar process and electroodontic diagnostics.
Fractures of teeth occur in the area of the crown, root, crown and root; microfractures of cement are distinguished, when sections of cement with attached perforating (Sharpey) fibers peel off from the dentin of the root. The most common fractures of the tooth crown are within the enamel, enamel and dentin with exposure of the pulp. The fracture line can be transverse, oblique and longitudinal. If the fracture line is transverse or oblique, passing closer to the cutting or chewing surface, the fragment is usually lost. In these cases, tooth restoration is indicated by prosthetics with inlays and artificial crowns. When opening the pulp, orthopedic measures are carried out after appropriate therapeutic preparation of the tooth.
For fractures at the neck of the tooth, often resulting from cervical caries, often associated with an artificial crown that does not tightly cover the neck of the tooth, removal of the broken part and restoration using a stump pin insert and an artificial crown are indicated.
A root fracture is clinically manifested by tooth mobility and pain when biting. The fracture line is clearly visible on dental x-rays. Sometimes, in order to trace the fracture line along its entire length, it is necessary to have x-rays obtained in different projections.
The main method of treating root fractures is to strengthen the tooth using a dental splint. Healing of tooth fractures occurs after 1 1/2-2 months. There are 4 types of fracture healing.
Type A : fragments are closely juxtaposed with each other, healing ends with mineralization of the tooth root tissue.
Type B: healing occurs with the formation of pseudarthrosis. The gap along the fracture line is filled with connective tissue. The radiograph shows an uncalcified band between the fragments.
Type C : connective tissue and bone tissue grow between the fragments. The x-ray shows the bone between the fragments.
Type D : the space between the fragments is filled with granulation tissue: either from the inflamed pulp or from gingival tissue. The type of healing depends on the position of the fragments, immobilization of the teeth, and pulp viability.
- Fractures of the alveolar ridge
Treatment of alveolar bone fractures is mainly conservative. It includes repositioning the fragment, fixing it and treating damage to soft tissues and teeth.
Reposition of the fragment in case of fresh fractures can be carried out manually, in case of old fractures - by the method of bloody reposition or with the help of orthopedic devices. When the fractured alveolar process with teeth is displaced to the palatal side, reposition can be performed using a palatal release plate with a screw. The mechanism of action of the device is to gradually move the fragment due to the pressing force of the screw. The same problem can be solved by using an orthodontic apparatus by pulling the fragment towards the wire arch. In a similar way, it is possible to reposition a vertically displaced fragment.
If the fragment is displaced to the vestibular side, reposition can be carried out using an orthodontic apparatus, in particular a vestibular sliding arch fixed on the molars.
Fixation of the fragment can be carried out with any dental splint: bent, wire, soldered wire on crowns or rings, made of quick-hardening plastic.
- Fractures of the body of the upper jaw
Non-gunshot fractures of the upper jaw are described in textbooks on surgical dentistry. Clinical features and treatment principles are given in accordance with Le Fort's classification, based on the location of fractures along lines corresponding to weak points. Orthopedic treatment of fractures of the upper jaw consists of repositioning the upper jaw and immobilizing it with intra-extraoral devices.
In the first type (Le Fort I), when it is possible to manually set the upper jaw into the correct position, intra-extraoral devices supported on the head can be used to immobilize fragments: a solid-bent wire splint (according to Ya. M. Zbarzh), a dentogingival splint with extraoral levers, soldered splint with extraoral levers. The choice of design for the intraoral part of the apparatus depends on the presence of teeth and the condition of the periodontium. If there are a large number of stable teeth, the intraoral part of the device can be made in the form of a wire dental splint, and in the case of multiple absences of teeth or mobility of existing teeth - in the form of a dentogingival splint. In toothless areas of the dentition, the dentogingival splint will consist entirely of a plastic base with imprints of antagonist teeth. In case of multiple or complete absence of teeth, surgical treatment methods are indicated.
Orthopedic treatment of a Le Fort type II fracture is carried out in a similar manner if the fracture was not displaced.
In the treatment of fractures of the upper jaw with posterior displacement | di there is a need to stretch it anteriorly. In such cases, the design of the apparatus consists of an intraoral part, a head plaster cast with a metal rod located in front of the patient's face. The free end of the rod is curved in the form of a hook at the level of the front teeth. The intraoral part of the device can be either in the form of a dental (bent, soldered) wire splint, or in the form of a dentogingival splint, but regardless of the design, in the anterior section of the splint, in the area of the incisors, a hooking loop is created to connect the intraoral splint with the rod coming from the head bandage .
The extraoral supporting part of the device can be located not only on the head, but also on the torso.
Orthopedic treatment of upper jaw fractures of type Le Fort II, especially Le Fort III, should be carried out very carefully, taking into account the general condition of the patient. At the same time, it is necessary to remember the priority of treatment measures according to vital indications.
- Fractures of the lower jaw
The main goal of treating fractures of the lower jaw is to restore its anatomical integrity and function. It is known that the best therapeutic effect is observed with early connection to the function of the damaged organ. This approach involves treating fractures in conditions of lower jaw function, which is achieved by reliable (rigid) fixation of fragments with a single-jaw splint, timely transition from intermaxillary to single-jaw fixation and early therapeutic exercises.
With intermaxillary fixation, due to prolonged immobility of the lower jaw, functional disorders occur in the temporomandibular joint. Depending on the timing of intermaxillary fixation, after removal of the splints, partial or complete restriction of movements of the lower jaw (contracture) is observed. Single-jaw fixation of fragments does not have these disadvantages. Moreover, the function of the lower jaw has a beneficial effect on the healing of fractures, thereby reducing the treatment time for patients.
The description of the advantages of single-jaw fixation does not make them the only way to fix fragments of the lower jaw. There are certain contraindications to them: for example, with fractures of the lower jaw in the area of the angle, when the fracture line passes through the attachment points of the masticatory muscles. In such cases, intermaxillary fixation is indicated, otherwise contracture may occur due to reflex-painful contraction of the masticatory muscles.
At the same time, when using intermaxillary fixation of mandibular fragments, timely transition to a single-jaw splint is important. The timing of the transition depends on the type of fracture, the nature of the displacement of fragments and the intensity of reparative processes and ranges from 10-12 to 20-30 days.
The choice of design of an orthopedic device in each specific case depends on the type of fracture, its clinical characteristics, or is determined by the sequence of therapeutic interventions. For example, in case of a median fracture of the body of the lower jaw with a sufficient number of stable teeth, manual reduction is performed on the fragments and the fragments are fixed using a single-jaw dental splint. The simplest design is a bent wire splint in the form of a smooth bracket, secured to the teeth with ligature wire.
In case of a unilateral lateral fracture of the body of the lower jaw, when a typical displacement of the fragments occurs: upward of the small one under the influence of the masticatory, medial pterygoid, temporal muscles and downward of the large one as a result of traction of the digastric, geniohyoid muscles, the design of the fixing apparatus must be strong. It must resist the pull of these muscles, ensuring the immobility of the fragments during the function of the lower jaw.
This problem is quite satisfactorily solved by the use of a single-jaw soldered wire splint on crowns or rings.
In case of a bilateral lateral fracture, when three fragments are formed, there is a danger of asphyxia due to the retraction of the tongue, which moves back down along with the middle fragment; urgent reposition and fixation of the fragments is required.
When providing first aid, you should remember the need to stretch the tongue and fix it in the forward position with an ordinary pin.
Of the possible options for immobilizing fragments in this type of mandibular fracture, the optimal one is intermaxillary fixation using dental splints: soldered wire splints with hooking loops, bent aluminum splints with hooking loops, standard Vasiliev tape splints, splints with hooking protrusions made of fast-hardening plastic. Their choice depends on specific conditions, availability of material, technological capabilities and other factors.
Fractures in the area of the angle, branches of the jaw and condylar process with slight displacement of fragments can also be treated with the listed devices that provide intermaxillary fixation. In addition to them, other devices are used to treat fractures of this location - with an articulated intermaxillary joint. This design eliminates the horizontal displacement of a large fragment during vertical movements of the lower jaw.
Treatment of multiple fractures of the lower jaw is carried out using a combined method (operative and conservative). The essence of orthopedic measures lies in the reposition of fragments, retention of individual fragments in accordance with the occlusal relationships of the dentition. Reposition of each fragment is carried out separately and only after this the fragments are fixed with a single splint. Fragmentary reduction can be performed using dental splints. To do this, splints are made with hooking loops for each fragment and a splint for the upper row of teeth. Then, using a rubber rod, the fragments are moved to the correct position. After matching, they are connected with a single wire splint and the entire block is fixed to the splint of the upper dentition according to the type of intermaxillary fixation.
Orthopedic treatment of mandibular fractures with a bone defect is carried out using all the main methods of treatment of maxillofacial orthopedics: reduction, fixation, shaping and replacement. Their sequential use in the same patient can be carried out with different devices or with one device - a combined multiple action.
When using orthopedic devices that perform one or two functions (reposition, reduction and fixation), there is a need to replace one device with another, which significantly complicates the treatment process. Therefore, it is advisable to use combined-action devices. For fractures of the lower jaw with a bone defect, when there is a sufficient number of stable teeth on the fragments, a mouth guard apparatus is used. It allows for consistent reposition of fragments, their fixation, and formation of soft tissues. The design of the device (I.M. Oksman) is known, with the help of which it is possible to carry out both reposition and fixation of fragments, and replacement of bone tissue defects. However, this does not mean at all that single- or dual-function devices have completely lost their significance.
In case of a lateral fracture of the body of the lower jaw with a bone defect and in the presence of supporting teeth on the fragments, the problems of reposition and fixation can be successfully solved using the Kurlyandsky apparatus.
Treatment of fractures of the lower jaw with a bone tissue defect in the absence of the possibility of constructing tooth-supported devices is carried out surgically or in a combined way. Among orthopedic devices, the Vankevich splint has received wide recognition.
In most cases, the outcomes of fracture treatment are favorable. For non-gunshot fractures after 4-5 weeks. the fragments heal, although the fracture gap can be determined X-ray even after 2 months.
To obtain such a favorable outcome, three main conditions must be met:
- accurate anatomical comparison of fragments;
- mechanical stability of the connection of fragments;
- preservation of blood supply to fixed fragments and function of the lower jaw.
If even one of these conditions is violated, the outcome of treatment may be unfavorable in the form of fusion of fragments in the wrong position or complete non-fusion with the formation of a false joint of the lower jaw.
Prolonged intermaxillary fixation of fragments and other reasons can lead to contracture of the lower jaw.
- Improperly healed jaw fractures
The main reason for improper healing of jaw fractures is a violation of the principles of treatment, in particular, incorrect comparison of fragments or their unsatisfactory fixation, as a result of which secondary displacement of the fragments occurs and their fusion in the wrong position.
The morphological picture of healing of incorrectly juxtaposed and poorly fixed fragments has its own characteristics. In this condition of the fracture, cellular activity is much higher, the connection is achieved due to a large influx of fibroblasts appearing in the tissues surrounding the fracture. The resulting fibrous tissue then slowly ossifies and the fibroblasts transform into osteoblasts. Due to the displacement of fragments, the relative position of the cortical layer is disrupted. Its restoration as a single layer is slowing down, since a significant part of the tissue is resorbed and most of it is reformed from the bone.
With improperly healed fractures, it is reasonable to expect a deeper and longer-lasting restructuring in the dental system, since the direction of the load on the jaw bones changes, pressure and traction are distributed differently. First of all, spongy bone undergoes restructuring. Atrophy of underloaded and hypertrophy of newly loaded bone crossbars occurs. As a result of such restructuring, bone tissue acquires a new architectonics, adapted to new functional conditions. Restructuring also occurs in the area of periodontal tissues. Often, a functional load changing in direction and magnitude can lead to destructive processes in the periodontium.
When jaw fractures heal incorrectly, there is a risk of developing TMJ pathology due to functional overload of its elements.
Incorrectly healed fractures are clinically manifested by deformation of the jaws and disruption of the occlusal relationships of the dentition.
In case of improperly healed fractures with vertical displacement of fragments, signs of an anterior or lateral open bite are observed. Fragments displaced in the horizontal plane in the transversal direction cause the closure of the dentition as a crossbite or a pattern of palatal (lingual) displacement of a group of teeth.
Relatively minor occlusal disorders can be corrected by prosthetics. Vertical discrepancies can be leveled with both fixed and removable prostheses: metal crowns, aligners, removable dentures with a cast occlusal overlay. For transversal occlusion disorders and a small number of remaining teeth, a removable denture with a duplicated dentition is used. The closure of the teeth is ensured by artificial teeth, and natural teeth serve only as a support for the prosthesis.
Orthodontic methods can also be used to eliminate occlusal disorders. Hardware, hardware-surgical methods for correcting bite deformities can have a high positive effect in the treatment of improperly healed jaw fractures.
- False joints
The morphological picture of the healing of a fracture ending in the formation of a pseudarthrosis is sharply different from that observed with complete healing of fractures. With false joints, signs are clearly visible that indicate low reparative regeneration of bone tissue: the absence of a sufficient number of osteogenic elements in the fracture area, the state of ischemia, the proliferation of scar tissue, etc.
Orthopedic measures for pseudarthrosis as the main method of treatment are used in cases where there are contraindications to bone grafting or it is postponed for a considerable time. Contraindications to osteoplastic surgery are mainly related to the general condition of the body (weakness and exhaustion) and the patient’s refusal to undergo surgery.
The choice of prosthesis design depends on the presence and condition of the remaining teeth, the size and topography of the defect. However, there is a general principle for designing dentures for false joints: making dentures from two halves, corresponding to two fragments, and movably connecting them to each other. This design is due to the fact that a single base leads to overload of supporting tissues and teeth due to multidirectional displacement of each fragment. With a movable connection of the two halves of the prosthesis, the functional overload is reduced.
Many methods have been developed for movably connecting prosthesis bases. The original designs of prostheses were proposed by I.M. Oksman. This is a prosthesis with a single-joint connection and a two-articular connection. The first design is used for low mobility, the second for large displacement of jaw fragments.
Dental prosthetics are mandatory when treating a false joint surgically. In this case, orthopedic treatment is an integral part of complex rehabilitation therapy.
- Contracture of the lower jaw
Treatment of contractures is conservative, surgical and combined. Conservative treatment consists of medications, physiotherapeutic methods, therapeutic exercises and mechanotherapy.
Nutrition
The recovery stage must be accompanied by a proper diet. During this period, the body needs more vitamins and nutrients, which must be obtained not only from food, but also from additional vitamin supplements.
During the period of active recovery, you need to saturate your diet with:
- protein (found in poultry, fish, meat);
- calcium and silicon (can be obtained from cottage cheese, oatmeal, beets, cheese, parsley, sesame);
- vitamins B, C and D (found in maximum quantities in fish oil, liver, bananas, legumes, citrus fruits).
While recovering from a fracture, you need to give up alcohol, sweet carbonated drinks, coffee, chocolate, fatty and salty foods.