- About the service
- Prices
- Consultation
- Stock
- Advantages
- Reviews
- Doctors
- Portfolio
- Licenses
- Contacts
Depulping a tooth before prosthetics in Moscow is a mandatory procedure that must be carried out in case of infection. It allows you to solve the problem without allowing further spread of the pathology. In our dental clinic, the pulp and nerve removal procedure is carried out by qualified doctors using modern technologies. At the same time, the cost is affordable, the quality of services is high. You can find out the exact price and make an appointment by phone or through the website.
Advantages of treatment at the DentBerg dental clinic in Moscow:
- the patient will not experience any discomfort during depulpation;
- the process of dental canal treatment occurs using modern equipment;
- in our dentistry we are ready to take on difficult cases;
- if necessary, after depulpation we can install a metal-ceramic crown;
- processing occurs using modern medical preparations;
- minimal risk of complications in the future;
- our dentists will remove a bundle of nerves only if indicated;
- guarantee for the services provided.
Tooth depulpation is carried out only when it is necessary to remove nervous tissue objectively. At the same time, our doctors act as carefully as possible to preserve most of the crown. They also carefully check the condition of the root canals after treatment. This allows you to avoid unpleasant situations associated with tool tips getting stuck in a tooth.
What is depulpation and what is its essence?
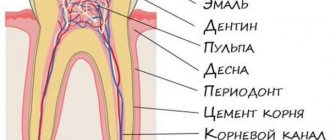
What does tooth depulpation mean? Let's break the word down into parts - “de” means “removal”, and “pulp” refers to the soft neurovascular bundle that is located inside the tooth cavity and in the root canals. That is, depulpation or depulpation is the removal of the so-called “dental nerve”. After which the “empty” areas are filled with filling mass or pins, and then closed with crowns, inlays or special fasteners for dentures. Depulpation[1] is irreversible, i.e. a new pulp does not form in place of the removed one. Dental tissues cease to receive nutrition from the inside, and the tooth itself is considered “dead.” But this does not mean at all that it will fall out soon.
Any dentist should be able to carry out this procedure, but in the field of work this is most often done by dental therapists or more specialized specialists - endodontists. That is, if a patient comes to an orthopedist for a prosthesis, then if pulp removal is necessary, he will refer the person to a dentist-therapist.
What you need to know about pulp removal before prosthetics
The standard procedure for depulping a tooth includes removing the enamel and then the pulp, cleaning the canals, using medication and filling or prosthetics. In the past, dentists were more likely to use a permanent filling or crown. Nowadays, more and more doctors use a temporary filling first to monitor the progress of treatment. And only after they are convinced that the infection process has stopped, they proceed directly to prosthetics.
It should be noted that the choice of a specific course of action directly depends on what will be more logical in a particular case. That is, the doctor makes a decision based on the overall picture and test results. In any case, before depulping, a photograph is taken.
What is the purpose of depulpation?
The goal of the procedure is to achieve several important results that will allow the patient to wear the prosthesis for a long time. Moreover, during the entire period of wearing the person will not be bothered by pain and the need to remove, for example, a crown. Let's take a closer look at what effect should be achieved:
- the pulp will not overheat during grinding of the stump and, accordingly, will not become inflamed (i.e., pulpitis will not appear under the crown),
- cariogenic bacteria will not penetrate into the pulp (i.e., pulpitis is again excluded),
- It will be possible to place pins or a core inlay into the canals: this will strengthen the restoration, i.e. it will last longer.
Don't know what type of prosthetics to choose?
We will help in the selection, advise where to read more information and compare types of prosthetics.
Consultation with an orthopedic doctor in Moscow clinics is free! Call now or request a call
Working hours: from 9:00 to 21:00 - seven days a week
When a nerve must be removed - indications
Whether tooth depulpation is necessary before prosthetics or not, only a doctor can say after a thorough examination - instrumental and x-ray. Mandatory removal of the dental nerve is necessary for the following indications:
- there are signs of pulpitis, i.e. inflammatory process of the pulp: pain, darkening of the deep layers of dentin,
- the top of the tooth is severely damaged,
- the natural crown has massive fillings,
- the patient often experiences relapses of caries,
- it is planned to install a crown with thick walls (for example, metal-ceramic): in this case, it is necessary to sharpen the stump quite strongly, which will lead to thinning of the dentinal layer (i.e., the pulp underneath will be less protected) and to its potential overheating during treatment with a drill. As a result, if depulpation is not performed, the risk of pulpitis increases and the time for re-prosthetics approaches.
Indications for removal
The more tissue that is removed during tooth preparation, the higher the risk of opening the pulp chamber. To avoid this, the nerve is removed before prosthetics. This is also done if:
- in the presence of a large cavity, due to which the dentin layer after preparation will become too thin to perform protective functions;
- when teeth move out or lengthen;
- when tilting, turning and abnormal positioning;
- in some cases in patients with periodontitis;
- with increased tooth wear of 2-3 degrees;
- when using large volume stump inlays;
- with increased tooth sensitivity that persists after treatment;
- when the neck of the tooth is exposed as a result of gum recession (loss).
In these cases, the pulp is removed even with healthy teeth. Also, manipulation is carried out in cases of root fracture, multiple caries and pulpitis (inflammation of the pulp).
When can you do without deletion?
Let's consider situations when depulpation can be abandoned, i.e. do not perform it before prosthetics:
- the stump (ground tooth tip) has thick walls,
- the pulp is not inflamed,
- in the future there is no risk of caries/pulpitis under the denture,
- overheating of dentin and pulp is excluded.
For veneers and restorative inlays, you can, in principle, do without depulpation altogether, as well as for thin ceramic crowns - but only if all the requirements just outlined are met.
What happens to a pulpless tooth?
Depulpation significantly reduces the risk of complications, but it has its drawbacks.
- Change in enamel color. Teeth become more dull and unnatural.
- Changes in the properties of enamel: when exposed to negative factors, it begins to collapse.
In other words, the tooth loses its natural properties, so to protect it, a crown is installed.
Contraindications to the procedure
Contraindication is children's age. Or rather, a milk bite - here it is forbidden to go through root canals with instruments, because... the developing rudiments of permanent teeth can be damaged. Intolerance or prohibition of the administration of anesthesia is also a contraindication. As well as serious mental disorders, when a person can unknowingly harm himself during dental procedures.
Read on the topic: indications and contraindications for installing dentures.
How is the procedure performed?
How is tooth depulpation done? It is carried out in at least 2 visits to the clinic. In one visit, removing the pulp and immediately placing a filling or pin can be dangerous because if pathological areas remain in the cavities, then over time inflammation will develop under the prosthesis. Next, we will consider how depulpation occurs and what stages are included in it.
First visit to the doctor
First of all, the patient is given an x-ray to find out the condition of the pulp and the presence of inflammation under the roots. Then they give a “freezing” injection with an anesthetic. To remove the pulp, the dentist needs to drill out part of the hard tissues - enamel and dentin. First, the pulp is removed from the pulp chamber. And then, using special endodontic instruments, you will need to remove all the loose pulp from the canals. After this, medicine is put inside and a temporary filling is placed, which lasts for an average of 7-14 days. During the process, you need to take an x-ray to assess the quality of the work. And in the most modern clinics, canals are treated under a microscope.
If the pulp is removed using arsenic paste, the treatment technology is different. Anesthesia is not required here, because... it does not hurt. Paste is placed into the cavity and closed with a filling. After 2-3 days, the patient must return to the clinic, because... It is during this time that arsenic will “kill” the pulp bundle and may begin to negatively affect healthy tissue. If the filling falls out or is damaged, you should immediately contact the clinic.
Second visit to the dentist
At the second appointment with the doctor, the medicine or arsenic paste is removed, the canals are processed, dried and sealed. Next, you again need to take an x-ray to assess the quality of the filling and the absence of “empty” areas. The patient is sent to an orthopedist, where the doctor will unseal the canal a little and place a pin, stump tab or attachment (lock) for a removable denture into it, and then take impressions for a crown or other orthopedic structure.
Operation stages
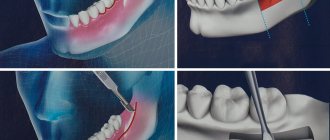
The standard technique involves performing a number of sequential manipulations:
- Antiseptic treatment of the oral cavity using bactericidal solutions to prevent infection of the exposed root canal;
- Introduction of anesthetic drugs - ultracaine or lidocaine - provided there is no allergy to the components included in their composition;
- Treatment of a carious cavity using a drill, followed by expansion of the dental canal and removal of dead tissue;
- Removing the nerve using a pulp extractor, the design of which resembles a needle with a thick handle;
- Stopping bleeding that occurs due to damage to capillary vessels - using hemostatic agents or thermal coagulation;
- Installation of a temporary filling made of composite material, which after a certain period is replaced with a permanent inlay.
One of the common methods of nerve devitalization is arsenic loading. Modern techniques make it possible to exclude the procedure from the protocol, but some experts consider it advisable.
Useful tips
Removing a nerve from a dental canal is a stressful situation against which the body requires a gentle regime. Compliance with medical instructions facilitates rehabilitation:
- During the first week after surgery, it is recommended to refrain from physical activity, including training in sports sections;
- Staying in the fresh air, especially in windy weather, should be reduced to a minimum;
- Due to the increased sensitivity of the jaw region, it is necessary to exclude hot foods from the diet and also avoid cold drinks.
In addition, doctors recommend giving up smoking and drinking alcohol for a while. For preventive purposes, it is allowed to take antibacterial drugs, and in case of pain, analgesics.
What to do if the pain under the crown does not go away
Painful sensations persist in the first days after depulpation, and are characterized by a gradual decrease in intensity. Factors that cause swelling or increased sensitivity include:
- Violation of the natural anatomical structure of the root canal;
- Poor cleaning of the cavity from the remains of the pulp structure;
- Making technical errors in the manufacture of a prosthesis;
- Low quality of material taken for filling;
- Inflammation resulting from tissue damage.
If the pain syndrome worsens at night and is characterized by pulsating manifestations, it is recommended to immediately consult a dentist to eliminate the possibility of the development of pathological inflammatory processes.
The appearance of pain and its causes
Why does a tooth hurt after pulp removal? Soreness often occurs after the anesthetic injection wears off. Pain after the procedure occurs for several reasons - normal and pathological. Here you need to understand the nature of the pain and what it is talking about.
For example, if the pain is tolerable or can be easily eliminated with painkillers, if it weakens every day, then this is a variant of the norm. After all, during the passage and expansion of the channels, healthy tissues were slightly injured, and pain is a natural reaction of the body. How long can a tooth without a nerve hurt after the procedure? On average, the discomfort goes away completely in 7-14 days. But in some patients it persists for 4-6 weeks and then disappears.
Read on the topic: what to do if a tooth hurts under a crown - causes of pain and methods for eliminating it.
The pathology is considered to be severe pain for several days, which is practically not relieved by pills. And also the reappearance of pain a few days or weeks after a period of painlessness. Symptoms such as severe redness and swelling of the gums, fever, headache, and bad breath should alert you. These signs most likely indicate that the depulpation was carried out incorrectly and inflammation began under the prosthesis. Or aggressive caries develops under the crown. Dental care is needed here, otherwise complications may arise - periodontitis, for example.
Why is it necessary to depulp a tooth during prosthetics, indications for the procedure
The need for pulp removal is a controversial issue with considerable debate among many dentists. On the one hand, every doctor tries to preserve living teeth, if there is even the slightest opportunity for this, because a tooth without a nerve becomes fragile: the nutrition of the enamel is lost. In addition, the “empty” tooth becomes insensitive and will not be able to give a signal about caries or other diseases.
On the other hand, the pulp is exposed during prosthetics, and, sooner or later, makes itself felt. Also, after the installation of a dental implant, pain symptoms may occur, the cause of which can only be understood after removing the artificial tooth, which will then be unusable.
Depulping a tooth before prosthetics is 100% necessary for:
- advanced caries that affects the pulp;
- inflammation in the pulp chamber or periodontitis;
- teeth tilted more than 10 degrees;
- presence of enamel hypersensitivity;
- having low, small teeth or their abnormal alignment.
How long will a tooth last with and without a nerve?
It all depends on the skill of the doctor, on how competently he assessed the future functionality of the tooth with or without the preserved nerve. If metabolic processes are maintained in the supporting unit (i.e., while the pulp is preserved), then its service life is expected to be longer than that of the pulpless one. When all the conditions on the part of the dentist are met, and the patient treats the restorations with care, then, if the nerve is preserved, the support under the prosthesis can last on average 8-10 years (under a single crown) and about 7 years under an extended structure. If a tooth is “dead,” then its service life is shorter by an average of 30%, i.e. about 5 years.
But if the prosthetics are performed poorly, if the patient does not take good care of the prostheses, then the nerve may become inflamed - and very soon treatment and a new orthopedic design will be required.
Does the shade of dental tissue change after the procedure?
Does the tooth darken after depulpation? Yes, over time the color will change - it will become gray and lifeless, because the tissues do not receive nutrition from the inside. But the pulpless unit is covered with a prosthesis - so the change in shade will be completely invisible from the outside. If the color of the prosthesis itself has changed, then the reason for this may be the following:
- the use of low-quality materials for manufacturing or non-compliance with its technology,
- staining from coffee, wine, food coloring, tobacco,
- formation of plaque and stone due to poor oral hygiene.
When is depulpation prescribed?
An intervention of this kind is necessary when it is necessary to stop pathological processes in the soft tissues of the tooth. Indications for the procedure are:
- sharp pain followed by prolonged aching pain;
- caries, which destroyed the protective tissues of the tooth and caused inflammatory processes in the pulp;
- pulpitis, requiring complete or partial removal of the pulp;
- periodontitis;
- mechanical damage to the tooth, which resulted in exposure of the neurovascular bundle;
- prosthetics;
- dental defects;
- there is excessive tooth wear;
Before carrying out the depulpation procedure, the specialist must conduct a visual and instrumental examination of the patient. After collecting an anamnesis, taking into account the analysis of x-rays, the doctor determines the feasibility of the manipulation.
Important: Sometimes before depulping, professional teeth cleaning is carried out: removing plaque and tartar. Manipulations are recommended if without them it is not possible to obtain a long-term result.
Prosthetics after tooth depulpation
After removing the tissues that fill the tooth cavity, containing blood vessels and nerves, the tooth is considered “dead.” He becomes vulnerable and brittle. To prevent the destruction of the dental element in the future, the doctor recommends installing a crown on it after depulping the tooth. When filling, the pulp is replaced with a composite material. The sealed element of the dentition, along with other teeth, participates in the processes of chewing food and is subjected to significant loads. To prevent staining of the filling, it is covered with a crown.
Depulpation of teeth during prosthetics
But there is also the exact opposite process. If the patient wishes to install a permanent denture, the specialist must examine the teeth that will be involved in the procedure. In some cases, the dentist prescribes pulpotomy of all or some elements of the dentition:
- with increased tooth sensitivity;
- in case of deformation and incorrect positioning of the tooth in the row;
- with initial signs of pulpitis;
- for chronic caries.
Depulpation before prosthetics is carried out, since after installing a permanent prosthesis, it will be more difficult to treat the tooth; you will need to remove the bridge or crown, which is a traumatic factor. In addition, under the bridge, pathological processes can develop much faster and be more widespread.
Whitening of pulpless teeth
After pulp removal, teeth become susceptible to external factors. They can quickly lose their aesthetic appeal as they darken. In this case, a color restoration procedure is recommended. It is called “endobleaching”. The essence of the manipulation is the introduction of a lightening substance into the tooth. Endobleaching is performed without pain.
Indications for tooth whitening after pulp removal are:
- filling with a coloring composition;
- darkening of dentin under the influence of dyes: tea, coffee, nicotine.
Endo-stripping involves removing the filling and cleaning the composite material from colored particles. Bleach is injected into the existing cavity, and the tooth cavity is covered with a temporary filling that will last two weeks.
When you visit the dentist again, the temporary filling and coloring material are removed. The tooth is restored with special materials. The recommended frequency is once a year.
Consequences of tooth depulpation
Sometimes after removal of the nerve, the patient feels pain in the tooth, and swelling of the gums is observed. Reaction to cold and hot food or mechanical stress can be caused by:
- the body's reflex to remove the pulp;
- poorly performed depulpation procedure;
- the presence of nerves that were not removed;
- using unsuitable filling material;
- inflammation of the gums caused by tissue trauma during treatment;
- the presence of pathological processes in the adjacent element of the dentition, when the pain radiates to the “dead” tooth.
Only a specialist can determine the cause of the pain. If the pain is caused by inflammatory processes, a specialist may prescribe antibiotics. If the sensations are caused by a poor-quality depulpation procedure, it is necessary to re-open the canals, clean them, and restore the tooth with a composite. If you ignore prolonged painful sensations, a gumboil, fistula or cyst may develop.
Tooth removal: contraindications
Dental pulpotomy is not performed for the following diagnoses and conditions:
- acute leukemia;
- chronic heart disease;
- pregnancy;
- infectious hepatitis;
- stomatitis in acute or chronic stages;
- hemorrhagic diathesis;
- inflammatory diseases of the oral cavity and upper respiratory tract.
If there are contraindications to pulp removal, the dentist should offer an alternative treatment method.
How long will a tooth last after pulpotomy?
It is important to understand that the resource of a pulpless tooth may vary from patient to patient. Even in one person, two different teeth after depulpation can “behave” differently.
If the procedure is carried out in compliance with the protocol, the canals are thoroughly cleaned, their sealing is achieved, and pathological tissue is completely removed, the tooth can last several decades. The service life of a tooth after pulpotomy increases significantly if a high-quality and reliable crown is installed on it.
How to avoid tooth depulpation?
If pathological processes are already running, it will not be possible to avoid the procedure. If left untreated, the tooth will be lost. It is possible to exclude depulpation only if the occurrence of pathological processes is prevented. In this case, prevention is the best ally.
Careful care of the oral cavity with well-chosen products, a nutritious and balanced diet, and regular visits to the dentist will help keep the elements of the dentition healthy and prevent the development of caries and other pathologies.
What complications may arise
During the process of removing the dental nerve, the following complications may occur:
- perforation of the root wall,
- exit of the instrument or filling mass beyond the root: as a result, periodontitis begins - root inflammation,
- fracture of the instrument in the root canal: such fragments are very difficult to remove, sometimes the entire tooth has to be removed.
Many dentists perform pulp removal only to insure against possible complications after prosthetics - caries or periodontitis. After all, then you will have to remove the prosthesis, treat the tooth, and then make a new prosthesis, because the old one either cannot be removed without damage, or it will not fit on a fresh filling or stump inlay. But let us repeat once again, they will not remove the nerve without clear indications.
Complications
The most common complications after nerve removal before replacement are pain and swelling. Normally, these symptoms go away within a day at most. If the pain does not go away, intensifies, or swelling does not subside, you need to consult a doctor. He will conduct diagnostics to identify the causes. It could be:
- Poor quality channel cleaning
. An incorrectly chosen length of the tool does not allow you to go through the canal to the end. Remains of pulp cause inflammation - residual pulpitis. - Root canal perforation
. Through the destroyed apex, the infection penetrates into the periodontium (tissue around the tooth), causing pain. - Missing tooth canals
. All canals are not always visible on the image, and this is the only source of information for the dentist. The remaining pulp becomes inflamed, causing discomfort. - Tooth fracture
. If the anatomical shape of a tooth is not restored immediately, it may break. - Violation of sealing technology
. This may be incorrect proportions for mixing the composition or the filling material getting on soft tissues.
Sometimes, after endodontic treatment, the tooth darkens. Without pulp, no food is supplied to the tooth, and cells are not renewed. Dentin dries out and its color darkens. Another reason is that the enamel becomes porous and pigments penetrate through it more easily. Sometimes, the tooth darkens due to hemorrhage when the nerve is removed before prosthetics.
Don't be afraid, it's not dangerous. The denture will provide a protective barrier and hide discoloration.
Features of care after removal
Oral care after dental nerve removal and prosthetics must be regular and thorough. Twice a day you need to use a brush and paste, follow the correct cleaning technique (only sweeping movements). It is recommended to rinse your mouth after each meal, and also to exclude toffees, chewing gum, hard pieces of food, and not to chew nut shells or seeds. In order to promptly identify and eliminate dental problems, you should visit an orthopedic dentist at least 1-2 times a year.
“I had a crown placed on a post about 7 years ago. They did it very well and treated it under a microscope. But after the prosthetics, the dentist told me not to forget to come to them every year or every six months for an examination. At the same time, professional hygiene was carried out. I’ve never had any problems in all this time, I eat whatever I want.”
Anna, review from irecommend.ru
Advantages and disadvantages of depulpation
The advantages of tooth depulpation are that it will eliminate or almost completely minimize the risks of pathologies appearing under the prosthesis - it all depends on the skill of the dentist and the patient’s attitude towards the new smile. The disadvantage is that the tooth will become “dead”, i.e. more fragile and with a shorter service life than non-pulpless. But these shortcomings are eliminated, again, by high-quality treatment and materials, and competent care of restorations, as well as the absence of extremely high chewing loads.
Risks of tooth depulpation
Despite the fact that this operation is not uncommon in modern dentistry, several of its disadvantages can still be identified:
- after depulpation, although the tooth is preserved, it is dead inside, so the enamel becomes more fragile and less sensitive;
- if the channels are not completely cleaned or poorly disinfected, this can provoke inflammation, suppuration, abscess, the occurrence of granuloma, fistula, cyst, and flux.
Therefore, the operation is serious and requires special scrupulousness. The future fate of the tooth depends on the quality of depulpation. With proper care and patient recommendations, even without pulp, teeth can last for quite a long time.
The iOrtho clinic network provides high-quality services for correcting malocclusion with Invisalign aligners, sign up for a consultation now!
How much does depulpation cost?
How much does tooth removal cost? The cost of the procedure ranges from 3000-4000 rubles per 1 tooth in small cities, and in large cities, when treated under a microscope, from 3000-4000 rubles per 1 root canal (there can be 3-4 of them in one tooth). It is more profitable if the clinic offers turnkey installation of the prosthesis - absolutely all manipulations, examinations and materials are included in the total price.
[1] Shashmurina V.R. Biomechanical features of dental depulpation, 2022.
Author: Dulgarov Zh. G. (Thank you for your help in writing the article and the information provided)
Promotions of the DentBerg clinic
Ceramic veneer
Promotion for installation of E-Max ceramic veneer at the DentBerg clinic.
25,000 19,900 rub. More details
the promotion is valid until 12/31/2021
5% discount on dental prosthetics for pensioners
Get a 5% discount on dental prosthetics at the DentBerg clinic.
More details
the promotion is valid until 12/31/2021