Causes
In the history of dentistry, about four hundred theories of the occurrence of caries are known. Among the recognized ones are chemical-parasitic, physical-chemical, trophic, but none of them fully explains the etiology of the disease. Today it is believed that pathology develops against the background of the interaction of a chain of internal and external factors. This happens when demineralization processes in enamel prevail over remineralization. It is believed that the development of caries is directly related to the microflora in the oral cavity, where streptococci live.
Causes and types of complications
The culprits in the development of caries and its complications are streptococcus bacteria – Streptococcus sanguis, mutans, viridans. These pathogenic microorganisms oxidize and destroy tooth enamel, and then penetrate deep into the hard tissue through the dentin canals.
In the absence of proper treatment, the infection affects the coronal part of the soft tissue, the pulp, and the first stage of complicated caries occurs - acute pulpitis.
Pulpitis
When the infection reaches the pulp, an inflammatory process begins in the neurovascular bundle of the tooth in the form of:
- acute focal;
- diffuse (general) pulpitis,
a characteristic symptom of which is severe, throbbing pain in the tooth and increased sensitivity to cold.
If you do not go to the dentist with pulpitis in the first 2-3 days, the acute stage of the complication becomes chronic and develops:
- fibrous;
- hypertrophic;
- concretory;
- or gangrenous chronic pulpitis.
With chronic pulpitis, the inflamed tissue of the neurovascular bundle degenerates and is gradually destroyed, dentin formation in the tooth stops, and it becomes dead.
Over time, decay processes reach the peri-apical tissues and ligamentous apparatus - periodontium.
Periodontitis
Between the root of the tooth and the alveolus there are periodontal tissues, they act as a shock absorber during chewing and hold the tooth in the socket.
With periodontal inflammation, periodontitis, the integrity of the tooth ligaments is disrupted, the jawbone becomes infected and damaged.
Symptoms of acute periodontitis:
- acute pain when biting or touching a tooth with the tongue;
- pain is transmitted along the trigeminal nerve - to the temple and jaw;
- general malaise, deterioration of health;
- increase in body temperature to 37-38 degrees.
The acute phase with severe pain lasts from 2 to 14 days, after which the disease takes on a chronic form.
With chronic fibrous or granulating periodontitis, a fistula, that is, a through hole, can form in the gum. Patients also complain of a feeling of the diseased tooth moving out of its row and attacks of aching pain.
Granuloma
An advanced form of chronic periodontitis, granulomatous, leads to the formation of a capsule with exudate (pus) at the apex of the tooth - granulomas.
The gums of the diseased tooth become inflamed, patients complain of a feeling of bulging bone and persistent, severe pain.
A granuloma that is not eliminated in time can cause the formation of gumboil or a cyst at the root of the tooth.
Multiple caries
Another common type of complication is multiple (acute, blooming) caries, in which the infection simultaneously affects the coronal part of eight or more teeth.
In record time, caries destroys the enamel-dentin junction, penetrates the pulp and leads to tooth loss. The infection affects the cement on the roots of adjacent teeth, and the patient feels as if the entire dental arch hurts. Most often, multiple caries is detected in people with diabetes and preschool children.
Pathogenesis of caries: mechanism of disease development
Streptococci form colonies in the oral cavity - so-called dental plaques. This process goes through three stages:
- Formation of acellular organic film on the surface of the enamel - pellicles. The process takes up to several hours. The basis of the film is glycoproteins and other proteins in saliva.
- Collection of microorganisms and epithelial cells on the surface of the pellicle with subsequent growth of bacterial colonies. Continues for several days.
- Formation of mature dental plaque.
Dental plaque includes up to 70% microorganisms and has a mesh structure with semi-permeable properties. Carbohydrates easily penetrate into it and have a destructive effect on the tooth.
How does enamel destruction occur?
When eating carbohydrate foods, the microflora of the dental plaque instantly absorbs saccharides. This leads to a “metabolic explosion” and a sharp increase in acidity. After half an hour, the acidic environment is neutralized by saliva, but when carbohydrates are reintroduced, the pH level under the plaque decreases again, which leads to damage to the enamel due to increased permeability.
Against the background of the formation of organic acids on the enamel, demineralization increases, and the microspaces between the crystals of enamel prisms increase. This promotes more intensive penetration of microorganisms and their metabolic products into enamel microdefects. A cone-shaped lesion is formed, which spreads into the depths of the tooth. After some time, the surface layer of enamel dissolves - caries progresses and can lead to the removal of a baby tooth if no action is taken.
How does tooth resistance affect pathological processes?
Resistance is the ability of a tooth to withstand external influences. It depends on many factors:
- type of enamel hydroxyapatite, correctness of the protein matrix, degree of mineralization of the matrix, interaction of mineral phases and protein;
- the presence of defects in the enamel, the regularity of its structure, an electrical charge on the surface that prevents or promotes the adsorption of microorganisms;
- relief of the enamel surface, depth and shape of fissures, nature of the pellicle;
- type of structure of the skull, jaws, bite, proximity of teeth and the size of the spaces between them, etc.;
- functioning of the salivary glands;
- nutritional characteristics and somatic health.
The structure of enamel is formed at the genetic level and depends on mineralization processes.
Saliva
Saliva is the environment in which teeth are constantly present. Under favorable conditions, the processes of demineralization and remineralization occur harmoniously in it. If its composition is violated, a failure occurs. In combination with other cariogenic factors, changes in the composition of saliva provoke the formation of new lesions.
A change in the composition of saliva in an unfavorable direction occurs after taking sugar and easily digestible carbohydrates. To avoid this process, it is necessary to eliminate carbohydrates from the diet or get rid of dental plaque.
Other pathological causes contributing to the development of caries
The condition of the mother during pregnancy is of decisive importance for the health of the enamel. With toxicosis, carbohydrate metabolism disorders, gastrointestinal and thyroid diseases, chronic hypoxia, the mineralization of primary teeth in a child in the womb slows down.
Especially often, caries occurs immediately after teething in premature babies who are bottle-fed, as well as those who have suffered serious illnesses during the first year of life. The hardness of dental tissue depends on the state of the child’s digestive tract, the amount of fluoride in drinking water, and concomitant diseases during the first years of life.
Even the condition of the pulp affects the solubility of enamel. If the latter retains high functional activity, the enamel will remain hard. In turn, the condition of the pulp worsens after infectious diseases. In such children and adults, caries develops more often and more intensely, which is associated with a decrease in the immunological reactivity of the body.
Diagnostic methods
To accurately determine the nature of dental damage, doctors use many methods. The main types of diagnostics include:
| Inspection of the tooth surface with staining to identify carious spots. |
| Probing. Allows you to determine the depth of the carious cavity, assess the condition of the pulp chamber, the density of the affected tissue, and the degree of pain. |
| Electroodontometry. A test to determine the degree of excitability of the pulp. Normally, in an inflamed or necrotic state, it reacts differently to irritation. |
| Percussion (tapping). In case of caries, the procedure is painful for the patient; a healthy person will not pay attention to it. |
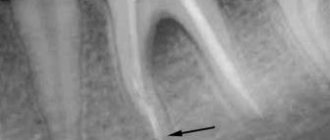
| X-ray. Using interproximal radiography, it is possible to identify hidden caries and determine the depth and extent of tooth damage. The method is used only in combination with other diagnostic methods. |
These methods are applied only to carious teeth; healthy teeth are not subject to unnecessary diagnostics. Only a doctor with special education can determine what the research should be like. The patient can assist by providing the results of previously performed diagnostics. Using them, dentists determine how long ago the problems arose, how quickly dental caries and its complications develop.
Complications of caries
The destroyer of tooth enamel and dentin, caries, can lead to tooth loss and also cause severe inflammation of the pulp, peri-apical tissues and jaw.
Cariogenic bacteria streptococci, which form hollow cavities in untreated teeth, tend to infect the connective tissues that make up most of our organs. And this is fraught with the development of diseases such as endocarditis, chronic tonsillitis, lymphadenitis and abscess.
How quickly advanced forms of caries develop
Typically, from the moment a carious spot appears on the enamel to the formation of deep caries, it takes from 1 to 4 years; the infection affects root canals 2 times faster.
But there are cases when complete tooth destruction and the formation of complications occur in just 3-4 months; this is acute caries. The reason for this is individual resistance, that is, the susceptibility of teeth to caries.
Signs that caries has reached the deep layers of dentin:
- the appearance of short-term pain;
- increased sensitivity to cold and hot;
- bad breath.
And not always, when the form is neglected, the tongue rests on a deep relief cavity in the tooth - sometimes it is just a small hole in the enamel, behind which lies an almost completely destroyed tooth.
Risk factors for deep caries
Deep tooth decay with caries most often occurs in the presence of the following risk factors:
- Poor oral hygiene.
- Abuse of sweet and carbohydrate foods.
- Lack of calcium, fluorine, phosphorus, vitamin D in the body.
- Chronic pathologies of the gastrointestinal tract.
- Disturbances in the functioning of the endocrine and immune systems.
- Genetic background.
And, of course, one of the main reasons for the development of deep caries is late diagnosis and untimely treatment.
Forms of deep caries
Deep caries can occur in two forms - acute and chronic. Each has its own characteristics. Acute deep caries is characterized by rapid development and can affect a large area of the tooth in a short time. Upon superficial examination, the cavity in the tooth appears small. But further diagnostics show that this is deep-stage caries, and it has almost reached the tooth root. It is acute caries that is most often accompanied by a complication in the form of pulpitis. Therefore, when treating it, the dentist has to not only prepare the tooth and put a filling on the dental crown, but also remove the nerve and fill the canals.
Chronic deep caries, unlike acute caries, is a slow, sluggish process. Although most of the tooth with this form is destroyed, the carious cavity is smaller in area than with acute caries. The patient may complain of periodic aching pain, which does not depend on external stimuli and occurs on its own.
Depending on the affected area, deep caries can be divided into cervical, fissure or located on the front incisors.
Based on the speed of development of the pathological process, it is divided into compensated (relatively slow development), subcompensated (with an average speed of development) and decompensated (with a high speed of development). Objectively, any form of deep caries can be cured, but it will require varying amounts of time and effort.
How can deep caries be cured?
A disease such as deep caries can be treated in one or two visits.
The first option is carried out according to this scheme:
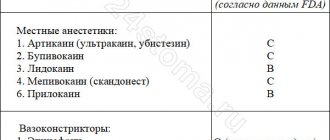
- The doctor numbs the affected tooth with a local anesthetic.
- Opens the carious cavity and, using a drill, cleans it of dead and diseased tissue until dense walls and bottom remain.
- If caries is complicated by pulpitis, endodontic treatment is carried out, that is, the dental canals are filled.
- To treat inflammation, isolate the sensitive pulp from the effects of filling material, and build up dentin, a therapeutic or insulating pad is placed at the bottom of the cavity.
- After all the above manipulations, the tooth is closed with a filling.
Treatment in two visits is carried out according to this scheme.
During the first visit, pain relief is performed, the cavity is opened and the affected tissue is removed. A medical pad is placed in the cavity and closed with a temporary filling. On the second visit after a few days or weeks, if the patient has no complaints, the temporary filling is replaced with a permanent one.
Treatment in two visits is considered preferable because it is possible to observe the condition of the tooth before installing a permanent filling. If pain, discomfort and other symptoms occur, additional therapeutic procedures can be performed to ensure that the affected tissue is completely removed. When treating a tooth in two visits, complications and relapses of caries occur much less frequently.
Prevention of caries complications
Having encountered such a problem at least once, most likely, you will no longer want to exhaust your body with toothache and shell out decent sums for complex treatment. Therefore, you should not neglect preventive measures: visit the dentist once every six months and carry out hygienic cleaning. If, nevertheless, a hole has formed in the tooth and it becomes ill, you should choose a doctor with extreme caution. Remember that the result of poor treatment will be a more serious complication of caries, which may require surgery, and, worse, tooth extraction. In addition, complicated caries requires more expensive treatment than its initial formations.
Agree, you never thought that such harmless caries can cause serious consequences, including tooth extraction. Now think about what is cheaper, faster and more painless - going to the dentist for an appointment twice a year or postponing this moment for several years, then heading straight to the dentist’s office? It’s up to you to decide, of course, but life is given to enjoy joyful moments, and not to endure toothache. And dentists are ready to help us with this!
Treatment of caries, is it painful to treat?
Caries is a slow-moving pathological process occurring in the hard tissues of teeth, which develops due to the influence of certain external and internal factors.
At the initial stage of development, caries is characterized by focal demineralization of the inorganic part of the tooth enamel and its gradual destruction, affecting the organic matrix, as a result of which this leads to a violation of the integrity of the hard tissues of the tooth with the formation of cavities in the dentin, and in the absence of timely treatment - to the occurrence of inflammatory complications with side of the pulp, leading to periodontitis.
Treatment of caries is completely painless, since all dental procedures are performed under complete anesthesia.
Epidemiology of root caries
The incidence of root caries is constantly increasing in older people. This is due to the fact that:
- There are more people with periodontal diseases, since their prevention is ineffective
- Dental care has improved, and retirees now have many more teeth in their mouths.
- Well, life expectancy has increased, where would we be without it?
Be that as it may, in our country today people suffer from root caries
- 1.3% aged 25-29 years
- and 35.2% (aged 55-64 years)
Features of diagnosing deep caries
Advanced caries often has the same clinical picture as pulpitis and some other dental diseases. Therefore, before starting treatment, the doctor must conduct a differential diagnosis and understand which pathology to treat.
Deep caries can be distinguished from focal pulpitis by a number of symptoms. With pulpitis, probing the cavity with a dental probe will cause pain only in one area - in the area of the pulp, while with deep caries pain occurs over the entire surface of the tooth.
The probing procedure will also help to distinguish deep caries from medium ones. On average, it is almost painless, because a fairly thick layer of dentin remains between the sensitive pulp and the bottom of the carious cavity. With a deep form, the tooth reacts to probing with severe pain. The method of electroodontodiagnostics helps to distinguish deep caries from fibrous pulpitis. In most cases, the doctor will order an x-ray to confirm the diagnosis.
How dangerous is caries in its advanced state?
So why is advanced caries so dangerous? Firstly, dental treatment in most cases will involve surgery, and any operation is always a risk: the risk of poor-quality treatment, the risk of swelling and other undesirable consequences. Secondly, serious exacerbations of caries will certainly affect your general well-being due to constant pain, which will be concentrated not only in the tooth area, but throughout the entire jaw, in the temples, ears and eyes, swelling of the gums and a sharp increase in temperature are also possible.
If caries is not treated and the pain is tolerated, the nerve of the tooth dies on its own and starts the process of decay in the carious cavity. The infection begins to penetrate deeper tissues, causing irreparable damage. The body begins to fight inflammation on its own, forming a granuloma around the tooth root, which can later increase in size and transform into a cyst. As you can see, the consequences of caries can be different, but one thing is clear - they are all serious and can have a significant impact on human health.