Trismus is a spasmodic compression of the mandibular muscle group (masticatory, temporal, pterygoid). The jaw loses mobility, freezes in one position, and the person is unable to do anything about it. The situation is accompanied by clenching of teeth, swelling and tightening of muscles, and increased pain on palpation.
This condition belongs to the pathologies of facial myalgia. The spasm can be either unilateral or bilateral (bilateral). In the first case, facial asymmetry is observed, the face skews to one side. In the second case, the person loses the ability to eat and talk. Trismus of the lower jaw has a negative effect on the functions of the gastrointestinal tract and brings significant psycho-emotional discomfort.
Jaw Information
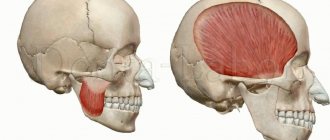
The jaws are a pair of bones that form the base of the mouth and teeth (see Figure 1).
- The maxilla is the upper jaw bone.
- The mandible is the lower jaw bone.
- The temporomandibular joint is where the lower jaw attaches to the skull.
- The masseter muscle is the muscle that connects the lower jaw to the skull.
Figure 1. Bones and muscles of the jaws
The opening and closing of the mouth is controlled by many muscles and nerves located around the jaws. Most people can open their mouth 35–55 millimeters (1.4–2.2 inches), which is the width of three fingers (see Figure 2).
Figure 2. Normal open mouth height
to come back to the beginning
Pain in the temporomandibular joint
Temporomandibular joint dysfunction (TMJ) is one of the most common causes of facial pain and is often incorrectly referred to as temporomandibular dysfunction. There are 2 main types of TMJ dysfunction: myogenic (the source of muscle pain) and arthrogenic (the source of pain is the TMJ). Understanding TMJ Dysfunction
This disorder involves the presence of the following symptoms: - pain or discomfort in or around the ear, TMJ and/or muscles of the jaw, face, temple area and neck on one or both sides.
Pain can occur unexpectedly and increase in frequency and intensity over months and years. Mouth opening with a click, crepitus, closing, restriction of opening or deviation of the lower jaw during movement, difficulty chewing, and headache are also associated with TMJ. Structure of the TMJ The
temporomandibular joint, or TMJ, is a freely rotating and sliding joint, covered with fibrocartilage, a football-shaped ball (condyle), a fibrous pad (disc), a bone socket for the pad (fossa), ligaments, tendons, blood vessels and nerves.
The disc functions as a moving shock absorber and stabilizer between the condyle and fossa. When the jaw opens, the condyle normally rotates first and then slides forward within the fossa with a disc located between the condyle and the fossa. Muscles of mastication
Muscles attached to the lower, upper jaw, skull and neck.
The muscles of mastication open, close, extend, and move your jaw, allowing you to speak, chew, and swallow. The accessory muscles of mastication (neck and shoulder muscles) stabilize the skull on the neck during chewing. Myogenic TMJ dysfunction (muscle-related)
Typically occurs due to overuse, fatigue, or tension in the masseter or accessory muscles, resulting in facial pain, headaches, and sometimes neck pain.
Arthrogenic TMJ dysfunction (joint-related)
Typically results from inflammation and degenerative changes in the hard and soft tissues of the joint.
Capsulitis or synovitis (inflammation), slipped disc (also called internal injury) and degenerative arthritis are the most common causes of TMJ dysfunction. Causes of TMJ Dysfunction The exact causes of TMJ
dysfunction are still unclear.
It is believed that the development of dysfunction is due to a combination of several severe factors, including injury and joint disease. Teeth clenching and grinding (bruxism), as well as tension in the neck and head muscles, are currently not proven causes of TMJ dysfunction, but they can aggravate the symptoms of this disease and must be taken into account in the treatment and management of patients with this pathology. It is important for patients with this dysfunction to understand that this disease can be chronic and can be very dependent on many factors, including emotional stability. Because there is no quick fix or emergency treatment for TMJ, the most successful and expert-supported treatments focus on self-monitoring and managing aggravating symptoms. Factors Associated with TMJ Dysfunction
- Trauma: Direct trauma to the jaw is associated with symptoms of dysfunction.
Direct trauma to the jaw can occur from a blow to the jaw, hyperextension (strain) of the jaw, and in some cases, compression of the jaw. Prolonged or forceful dental procedures, intubation during general anesthesia, and surgical procedures of the mouth, throat, and upper gastrointestinal tract (esophagus and stomach) can injure the TMJ. — Incorrect habits: Habits such as clenching teeth, clenching the jaw, grinding teeth (bruxism), biting lips or nails, chewing gum, and placing the jaw in abnormal positions are common. In relation to them, evidence of their involvement in the development of dysfunction has not been proven. Such habits are often associated with TMJ dysfunction and can contribute to the emergence of factors that translate into a chronic form and aggravate the existing symptoms of the pathology. — Occlusion: Dental occlusion refers to the way the teeth fit together or “bite.” Historically, dentists have viewed malocclusion as the primary cause of TMJ dysfunction. Recent studies have shown that malocclusion does not usually lead to this group of diseases, with the exception of a few cases. Each situation must be considered individually so that the doctor can make a differential diagnosis of facial pain. — Psychological factors: Many patients with TMJ dysfunction say that the onset of symptoms of the disease or worsening of its course is accompanied by an increase in emotional stress and psychological imbalance, leading to depression or anxiety. Scientific research shows that many patients with this dysfunction experience varying levels of depression and anxiety, and these levels are higher than those without this dysfunction. To date, it has not been established whether symptoms of depression or anxiety are present before the onset of TMJ dysfunction and then contribute to its formation, or whether chronic pain associated with this pathological condition leads to the formation of anxiety and depression. Many patients begin to clench and grind their teeth more frequently and intensely when they experience emotional stress, psychological imbalance, or pain. — Disorders of the temporomandibular joint: Some types of arthritis can lead to damage to the TMJ, as well as other joints. This is common in osteoarthritis developing in the aging population. Many other diseases, such as Parkinson's disease, myasthenia gravis, strokes, amyotrophic lateral sclerosis, can lead to excessive or uncontrolled movements of the masticatory muscles. — Other factors: Drug use and some prescribed medications can affect the central nervous system and muscles, and lead to TMJ dysfunction. Diagnosis of TMJ dysfunction.
Diagnosis of this disease should be part of routine practice among general practitioners and dentists.
A short set of diagnostic procedures may include: - History of the disease: complaints of pain in the jaw, headaches, neck pain, discomfort in the TMJ area, jaw closing, clenching of teeth, damage to the jaw, head, neck, as well as a history of cases of TMJ dysfunction or treatment of facial pain. - Objective examination: may include measurement of jaw opening, combined movements, jaw deviation during opening, palpation (finger pressure required) of the joint, jaw, head and neck muscles to determine pressure points and the presence of crepitus. It is also necessary to evaluate the gums, soft tissues of the mouth, teeth and make notes about the disease, the presence of dental lesions, as well as the symmetry of the jaw, face and head. If any abnormalities are found during the examination, a more detailed history should be collected and a more in-depth examination performed. Comprehensive assessment of TMJ dysfunction A comprehensive assessment may include:
- A complete analysis of all symptoms related to TMJ, head, neck, medical history, dental history, life history, heredity, psychological history.
— Comprehensive objective examination of the face, cervical spine, masticatory muscles, head and neck, neurological structures, teeth, gums, hard and soft tissues of the oral cavity. — Psychological history, including a short survey and testing. — Additional tests, including x-rays and imaging tests, biopsies, blood tests, urine tests, neurological tests, diagnostic injections. Treatment of TMJ dysfunction
Since there is no known cure for this pathology, the management of patients with symptoms of dysfunction is similar to the management of patients with other orthopedic or rheumatological disorders.
The goals of managing this group of patients are: reducing pain, adverse pressure and stress on the jaws, restoring jaw function, implementing a well-planned management program to treat the physical, emotional and psychological aspects. Management options and sequence of treatment for TMJ dysfunction are similar to other musculoskeletal diseases. As with many musculoskeletal disorders, the signs and symptoms of TMJ can be temporary and resolve on their own without developing serious long-term consequences. For these reasons, it is particularly important to try to avoid aggressive and irreversible treatment options such as surgery, major dental surgery or orthodontic treatment. Conservative management techniques include changes in behavioral habits, physical activity, medications, jaw exercises, and orthopedic devices. All of them have been found to be safe and effective treatments for cases of TMJ dysfunction. Most patients suffering from this disease achieve long-term remission with conservative therapy. Scientific studies show that in more than 50% of such patients, only a few symptoms persist or disappear completely. Self-monitoring of patients should include: - Limited jaw opening (no more than 2 fingers wide). — It is necessary to give your jaws a rest, avoiding prolonged chewing (chewing gum, bagels, tough meats). - Avoiding grinding and clenching of teeth by relaxing the jaw area and keeping the upper and lower rows of teeth at a distance. - Avoiding leaning or sleeping with the jaw resting. — Avoiding pushing movements with the tongue and chewing non-food items (nails, pens, pencils, etc.), stress, pressure on the jaw. - Use of cold, ice or moist-warm compresses, as prescribed by the attending physician or therapist. — Performing a massage of the affected muscles. - Perform gentle, limited jaw exercises as prescribed by your healthcare professional. — Use of medications as prescribed by the attending physician. Treatment options.
— Orthotics: You may be offered a brace (or a retainer known as a night watchman) that fits over your upper and lower rows of teeth.
The retainer has many different purposes, and it can be worn either constantly or part of the time, it all depends on the prescription of the attending physician. In most cases, retainers are used to separate rows of teeth, realign jaw joints, and help jaws relax. The unique style and adjustment of the brace will depend on your condition, how it changes while you wear the brace, and your overall treatment plan. Managing patients under stress.
One of the goals of treating TMJ dysfunction is to identify therapy for daily stress.
Your doctor may recommend several options for you to do this. These options include: biofeedback (biofeedback), breathing for relaxation, image management, and sometimes, referral to a specialist. Physiotherapy.
Physical therapists are specially trained professionals who assist in the rehabilitation of all types of physical injuries.
There are many treatment options that can help. These include: jaw exercises, posture training, ultrasound, electrical stimulation and mobilization. Your doctor and physical therapist will work together to formulate your treatment plan. Correcting your bite
Sometimes it is necessary to improve the way your teeth fit together.
This can be achieved in various ways. Orthodontics, usually with braces, will help move the teeth so they fit together better. In some cases, when the jaws themselves are not misaligned, they are corrected by a combination of treatment by an orthodontist and an oral surgeon. This is called orthognathic surgery. Correction of the bite occurs through the intensive work of the dentist, with the installation of crowns, bridges, and, if necessary, implants. This is done to replace missing teeth or to change the size and shape of teeth so that they fit together and function more harmoniously with the jaws and muscles. Surgery is sometimes performed to repair or reconstruct the jaws when conservative treatment fails to achieve comfort and good function. Surgery is rarely necessary, but it can be performed to remove debris that may have accumulated in the joint cavity, to repair damaged tissue, or even to replace the entire jaw, such as other joints (knees, hips, and shoulders). Conclusions
Extensive research is now being conducted to determine the safety and effectiveness of treatments for TMJ dysfunction/orofacial pain syndrome. Many researchers and clinicians advocate reversal and conservative treatment of dysfunction. Even when the symptoms of this dysfunction persist for a long time and are pronounced, many patients with this pathology do not require invasive treatment. Treatments designed to change the bite or reposition the jaws through orthodontic or dental reconstructive procedures are usually not necessary. And if they are used, then only when absolutely necessary. If permanent treatment is being considered for TMJ dysfunction or orofacial pain, we recommend seeking a second opinion. Specially trained dentists, physical therapists, psychologists and clinicians are often the best source of correct diagnosis and further management of this group of patients.
Exercises for the temporomandibular joint
About trismus
Trismus can occur at any time, immediately after or even years after treatment. This condition may occur in the following cases:
- if you have a tumor affecting the bones, muscles and nerves that control the opening of your mouth;
- after surgery on the head and neck organs;
- after radiation therapy in the head and neck area.
Trismus can occur when fibrosis (scarring) develops during the healing process of tissue after surgery. In addition, fibrosis may worsen years after radiotherapy.
If you cannot open your mouth wide enough, it will be difficult for the health care provider to examine your mouth. In this regard, problems may also arise with:
- oral hygiene (keeping the mouth clean and brushing teeth), which can lead to bad breath, tooth decay and oral infections;
- chewing and swallowing, which may make it difficult for you to eat and drink;
- speech;
- kisses;
- insertion of a breathing tube, for example if you ever need general anesthesia (a drug given to keep you asleep during an operation or procedure);
- carrying out routine dental treatment.
When trismus occurs, its treatment is very difficult. This is why it is important to prevent trismus and treat the condition as early as possible.
to come back to the beginning
Features of treatment for older patients
Among the common age-related changes in the lower jaw, changes in the content of water, organic and inorganic substances are noted, osteoporosis, atrophy and thinning of bone tissue are often detected. In addition, older patients often have concomitant diseases, such as diabetes. All of these factors can greatly limit treatment options. For example, if dentures are required, then in some situations the dentist may only offer removable dentures. Placing implants will be risky and ineffective.
Nevertheless, modern dental capabilities make it possible to find a way out of any, even the most difficult situation. A wide variety of materials and techniques can eliminate existing problems and significantly improve the patient’s quality of life.
How to prevent trismus
There are 4 main ways to prevent trismus:
- massage your jaw muscles;
- train your jaw muscles;
- maintain good posture;
- Maintain proper oral hygiene.
This should be done even if there are no symptoms of trismus to prevent it. Follow the directions in the section below. If you have had surgery, ask your healthcare provider if it is safe before you have surgery.
You may need a timer or watch to help you hold the stretching position for the required amount of time. Breathe normally and do not hold your breath. If you feel pain, numbness, or tingling, stop immediately and call your healthcare provider.
Massage your jaw muscles
Press your index and middle fingers against your cheekbone. Use your fingers to massage the masseter muscle, which is attached to the lower jaw (see Figure 3). As you move your fingers, look for areas that are tender or tight. Massage these areas with circular movements of your fingers for 30 seconds. Do this 2-3 times a day.
Try not to clench your jaw when you are stressed or out of habit. This will help relax your jaw muscles.
Figure 3. Massage the jaw muscles
Train your jaw muscles
Perform these exercises 3 times every day. You can do them standing or sitting. Use a mirror to help you do the exercises correctly.
These exercises will help stretch the muscles well, but should not cause pain. If an exercise causes pain or discomfort, try doing it with less effort. If pain or discomfort persists, contact your healthcare provider.
Range of motion and stretching exercises
Your head should remain in one position while performing these exercises. Repeat these steps 5 times.
- Open your mouth as wide as possible until you feel a good stretch but no pain (see Figure 4).
Hold this position for 10 seconds. Figure 4. Opening your mouth as wide as possible - Move your lower jaw to the left (see Figure 5). Hold this position for 3 seconds.
- Move your lower jaw to the right (see Figure 6). Hold this position for 3 seconds.
Figure 5. Jaw shift to the leftFigure 6. Jaw shift to the right
- Make circular movements with your lower jaw to the left.
- Make circular movements with your lower jaw to the right.
Passive stretching exercise
Figure 7. Press your thumb and index finger against your teeth.
Repeat these steps 5 times.
- Press your thumb against your upper teeth in the middle of your jaw.
- Press the index finger of your other hand against your lower teeth in the middle of your jaw (see Figure 7).
- Open your mouth as wide as possible. Place additional emphasis with your fingers so that your mouth does not close. You should feel a slight stretch, but not pain. Hold this position for ______ seconds.
Maintain proper posture
Correct posture means sitting and standing with your ears, shoulders, hips, knees and ankles aligned horizontally (see Figure 8). To have correct posture, it is necessary to maintain good tone and stretch in the muscles of the neck and shoulders. The following exercises will help you with this.
Figure 8. Correct posture
Do them 2 times every day. You can do them standing or sitting with your arms at your side.
Neck stretch
Repeat these steps 5 times. Hold each stretch for 30 seconds.
- Tilt your head forward (see Figure 9).
- Tilt your head back (see Figure 10).
Figure 9. Head tilt forwardFigure 10. Head tilt back
- Turn your head to the right (see Figure 11).
- Turn your head to the left (see Figure 12).
Figure 11. Turning the head to the rightFigure 12. Turning the head to the left
- Tilt your head, trying to bring your left ear closer to your left shoulder (see Figure 13).
- Tilt your head, trying to bring your right ear closer to your right shoulder (see Figure 14).
Figure 13. Head tilt to the leftFigure 14. Head tilt to the right
Chin retraction
Figure 15. Retraction of the chin when pulling the head back.
Repeat these steps 5 times.
- Looking forward, tuck your chin.
- Pull your head back so that your ears are level with your shoulders (see Figure 15). Stay in this position for 3 seconds.
Scapula compression
Repeat these steps 5 times.
- Tuck your chin in as described in the exercise above.
- Squeeze and squeeze your shoulder blades together as hard as possible (see Figure 16).
- Stay in this position for 3 seconds.
Figure 16. Squeezing the shoulder blades together
Maintain proper oral hygiene
- Brush your teeth and tongue in the morning after sleep, after every meal and before bed.
- If you have removable dentures, remove and clean them every time you brush your teeth. Don't go to bed with dentures in your mouth.
- Floss your teeth once a day before bed.
to come back to the beginning
What can you do at home if:
Head muscle spasms
To relieve spasm and pain, you can take aspirin, a painkiller tablet like Ibuprofen, or a painkiller in powder form (for example, Nimesil). Give yourself peace of mind. You can try pressing trigger points and stretching your earlobes.
Jaw muscle spasm
If trismus manifests itself, before the doctor arrives, you can self-massage the masticatory muscles, accelerating the blood in them, alternately pressing on the muscles constrained by spasm. It is also possible to use compresses (alternate warm and cold compresses, apply them to the lower third of the face).
Cervical muscle spasms
Make gentle rotational movements with your head, lower and lift it (without throwing it back too much), turn it right and left. You can try stretching your neck muscles with your hands. Warm compresses and rubbing are effective.
*Attention! The information is for informational purposes only and does not constitute medical advice.
Reviews
Tatiana
I’m happy to be among your guests at the clinic, I enjoy our communication, I’m grateful for your super professionalism, for giving beauty and a sense of confidence in your professional actions, protection from “age-related changes”?! I admire the combination of beauty, tenderness, intelligence, and fortitude! With respect, gratitude and love???
Olga
A modern clinic with friendly staff and highly professional doctors. I received a consultation on facial rejuvenation, a procedure was proposed that completely satisfied me, the consultation was very detailed. Satisfied with the visit.
Irina Nikolayevna
Clean, comfortable clinic, polite staff, professional specialists. The services are of excellent quality, I have been using the services for almost a year and a half, and have never had any problems with parking.
Anna and Alexander
Marina Vladimirovna, we wanted to express our gratitude to you for the Fotona 2D rejuvenation procedure. The skin is just super, and the scars on both of them are noticeably better. My husband says every day how beautiful and smooth his skin is, his nasolabial folds have disappeared. We are very pleased, we will come to you again!
In case of spasm of the masticatory muscles when opening the mouth
The sooner you begin treatment for spasms of the masticatory muscles, the easier it will be to resume normal jaw function. If you experience tension in your jaw, call your healthcare provider immediately. He or she may refer you to a specialist, as described below.
- See a speech and swallowing specialist, a physical therapist, or both. They will help you maintain your ability to open your mouth and regain any lost abilities. These professionals use a variety of techniques, such as exercise, stretching and massage. They may also recommend that you use special devices to help open your mouth.
- See a rehabilitation doctor. He will evaluate how well you can open your mouth. He or she may prescribe medications for pain or spasms (sudden, strong muscle contractions), suggest other treatments, or recommend medical devices to help you.
Your healthcare provider will discuss with you which specialist referral would be most beneficial for you.
to come back to the beginning
Signs of involuntary muscle contraction are:
- with bruxism – grinding of teeth during sleep, a feeling of overexertion in the jaws after waking up;
- with spasms of the head muscles - hoop-shaped pain in the temples, in the forehead, in the back of the head;
- pressing, pulsating, squeezing nature of pain;
- feeling of heaviness in the area of spasm;
- pain when pressing trigger points (try to palpate the area of the head when it hurts: when you press certain points, the pain increases significantly);
- nausea, vomiting, dizziness;
- painful reaction to light, loud sounds (infrequently).
When to see a doctor:
- headaches appeared suddenly and do not go away;
- you are experiencing muscle pain for the first time after 50 years;
- pain is accompanied by dizziness, weakness, numbness of the limbs;
- pain lasts more than two weeks in a row;
- painkillers either do not work at all or give an insignificant short-term effect;
- the pain is localized on one side of the head/neck.
Muscle spasms that provoke pain indicate a disruption in the healthy functioning of the body. To prevent the development of the disease, it is important to consult a doctor in time. We advise you to visit a therapist, neurologist, endocrinologist, who will prescribe detailed laboratory diagnostics for you. Based on the research results, specialists of another profile may be involved in your treatment: an orthopedist, a cardiologist, a chiropractor. Complex treatment may include taking medications, a massage course, and therapeutic exercises. A good doctor will definitely give you recommendations on nutrition and daily routine.
MIGUNOVA ANASTASIA ANDREEVNA
Cosmetologist
Initial consultation: 4500 rub.
VYATKINA IRINA SERGEEVNA
Gynecologist-endocrinologist
Initial consultation: RUB 8,500
KALININA EKATERINA ALEXANDROVNA
Cosmetologist
Initial consultation: 4500 rub.
KOZLOVA EKATERINA NIKOLAEVNA
Gynecologist, oncologist
Initial consultation: 5000 rub.
KUSRAEVA DIANA TEYMURAZOVNA
Cosmetologist, dermatovenerologist
Initial consultation: 4500 rub.