5. Dental devices used in the treatment of gingivitis
6. Complications and consequences of gingivitis
7. Prevention of gum disease
8. Diet for gingivitis
9. Prices for treating gingivitis in our clinic
Gingivitis is one of the most common periodontal pathologies, affecting the gums without compromising the integrity of the periodontal ligaments. The disease is inflammatory in nature and is manifested by hyperemia of the mucous membrane, swelling, and bleeding of the gums. In the early stages of its development, inflammation is easily treatable, but if gingivitis starts, it becomes chronic and requires more serious therapeutic measures.
Classification
Practicing dentists use a clinical classification of the disease, which involves dividing it according to the form of its course, the nature of the lesion and the localization of the inflammatory process. Depending on the course, gingivitis is divided into two types:
- Acute - occurs suddenly and occurs with pronounced symptoms that cause significant discomfort to the patient.
- Chronic – characterized by a long course with periods of exacerbation and remission. As a rule, the inflammatory process with this form of gingivitis worsens in winter or spring, which is due to a lack of vitamins and minerals in the body.
Based on the degree of spread, localized and generalized gingivitis are distinguished. In the first case, the disease affects one or more unrelated areas of the gum. In the second case, the inflammation covers a large area of the gingival margin, affecting one or both jaws (upper and lower).
Classification according to the nature of the lesion takes into account the difference in the clinical picture of the disease and provides for four types of gingivitis:
- Catarrhal is a common form of pathology, manifested by pain in the affected area, swelling and bleeding, which can occur while eating or brushing teeth.
- Ulcerative-necrotic - gingivitis of this type is characterized by the development of necrosis (death) of tissue with the formation of ulcers and general intoxication of the body.
- Atrophic – occurs against the background of a decrease in the volume of the gums and exposure of the dental neck. If left untreated, progressive gingivitis causes the patient's tooth roots to become exposed.
- Hypertrophic – manifested by an increase in gum papillae and is most often a consequence of vitamin C deficiency or hormonal imbalance.
The severity of a particular form of the disease is determined by the nature of its course and its spread throughout the periodontium. In particular, the mild degree is characterized by moderate symptoms of gingivitis and damage mainly to the interdental papillae. In moderate pathology, the inflammatory process covers the papillae and marginal gum, and in severe form it affects the entire gum, including its alveolar part.
Diagnostics
Symptoms of pathology are visible upon visual examination. To confirm, a scraping is taken from the surface of the ulcers and the samples are checked for the presence of anaerobic and fusobacteria, spirochetes.
Differential diagnosis
The task of differential diagnosis is to distinguish Vincent's stomatitis from ulcerative inflammation of the gums, which manifests itself against the background of blood diseases - leukemia, infectious mononucleosis and agranulocytosis. To do this, they take a peripheral blood test - from the vascular bed, that is, the usual finger prick blood test.
To differentiate ulcerative-necrotizing gingivitis from allergic stomatitis, an additional bacterioscopic examination - a smear - will be required. If it is suspected that inflammation has developed due to mercury poisoning, a urine test is performed.
If the pathology appears suddenly, it is recommended to take tests for HIV infection and syphilis, and be checked for cancer.
Causes of gingivitis and provoking factors
The infectious factor plays a fundamental role in the development of gingivitis. Caries, tooth deformation or malocclusion provide favorable conditions for the appearance of plaque and the proliferation of microbes in the oral cavity. Subsequently, the pathogenic microflora that accumulates in the dental plaque leads to a destructive effect on periodontal tissue and, as a result, causes inflammatory processes.
The bacterial etiology of gingivitis should be considered in combination with the individual characteristics of the organism and the influence of the external environment, which provides predisposing conditions for the development of the disease. The main causes of gingivitis include:
- poor oral hygiene;
- gum injury;
- decreased immunity;
- lack of vitamins or minerals in the body;
- tartar (supragingival and subgingival);
- poor quality dental treatment;
- the presence of braces or dentures, which complicate dental care.
In addition to the main reasons, there are a number of factors that can provoke the development of gingivitis. These are smoking, diabetes, depression, infectious or viral diseases (ARVI, tuberculosis, AIDS, etc.), malnutrition, chemical poisoning. Most often, pregnant women and children aged 3–6 years, as well as people with nasal breathing problems, suffer from gingivitis.
What is gingivitis
Gingivitis is treated by a periodontist.
Gingivitis is an inflammatory process that occurs inside the gums, sometimes accompanied by symptoms such as pain, swelling, swelling of the affected area and a general rise in body temperature. Gingivitis can occur in patients under a variety of circumstances; Inflammation such as gingivitis can occur due to traumatic effects on the gums, penetration of pathogenic microbes into the gums, hypothermia of the body, a sharp drop in immunity, deficiency of certain vitamins, and for other reasons.
Symptoms of gingivitis
The clinical picture of the disease can vary significantly depending on its type and severity, but there are general signs of gingivitis that are common to all its forms:
- pain in the gum area, which becomes more intense when chewing food, eating cold or hot;
- itching;
- redness of the gingival margin;
- bleeding gums;
- swelling of the affected area;
- bad breath.
If we consider the symptoms by type of disease, then with necrotizing ulcerative gingivitis the most striking manifestation is the formation of ulcers with the release of pus. Their number is rapidly increasing, the patient complains of severe pain in the gums and general intoxication of the body, manifested in the form of fever, weakness, and enlarged lymph nodes in the neck.
With atrophic gingivitis, the gums decrease in size, which leads to the gradual exposure of the dental neck. The patient notes the high sensitivity of the teeth to irritants and the appearance of interdental spaces in which pieces of food accumulate. Gradually progressive atrophy leads to exposure of the roots, which entails the development of periodontitis and tooth loss.
Signs of hypertrophic gingivitis vary depending on its form - edematous or fibrous. With edematous pathology, the patient is bothered by a strong burning sensation and enlarged gums, accompanied by a feeling of fullness. In the fibrous form of gingivitis, a characteristic symptom is gum overgrowth, which prevents the patient from eating. The gum becomes massive and dense to the touch, has an uneven surface with bumps.
Diagnosis of ulcerative gingivitis
Diagnosis of ulcerative gingivitis includes an examination by a dentist and laboratory tests. This comprehensive approach makes it possible to distinguish it from gum ulceration. To do this, a blood test is performed, as well as an examination of the contents of the inflamed area. Treatment of ulcerative gingivitis is selected individually, based on the results obtained.
During a dental examination, the doctor pays attention to the condition of the gums. Atrophic ulcerative gingivitis is characterized by hyperemia of the gums, which are covered with a grayish coating. It can be easily removed, revealing a bleeding wound underneath. This form of the disease is characterized by a decrease in gum size.
Treatment of gingivitis
Correct diagnosis of gingivitis plays an important role in the treatment of the disease, since the pathology has similar symptoms to periodontitis, stomatitis and periodontal disease. When conducting an examination at the Telo's Beauty clinic, the basic diagnostic method is to calculate the hygiene index, which is carried out using special coloring preparations. They are applied to the dental plaque and, based on visualization, areas of damage to the tooth and gums are determined.
Additional diagnostic measures for gingivitis include:
- determination of bleeding of the gingival groove - is carried out using periodontal probes, which make it possible to identify hidden areas of bleeding;
- an x-ray with which the doctor can understand whether the disease is gingivitis or whether it has already turned into periodontitis;
- orthopantomogram - an x-ray study aimed at studying the condition of the roots and their rudiments.
After diagnosis, treatment for gingivitis is prescribed, the methods of which may vary depending on the form of the disease.
Treatment of acute gingivitis
Anti-inflammatory and antibacterial treatment plays an important role in the treatment of acute gingivitis. Relief of inflammation is carried out through irrigation, rinsing and applications using medicinal ointments and gels. If there is no positive dynamics, non-steroidal anti-inflammatory drugs are prescribed, which help relieve inflammation and get rid of symptoms.
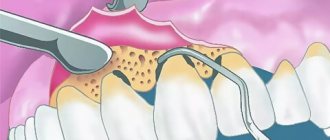
To eliminate the source of infection, soft and hard deposits on the teeth are removed. For this purpose, ultrasonic scalers or manual curettes are used. To prevent the re-formation of plaque, which can cause gingivitis, teeth are polished using special rotating instruments followed by the use of polishing pastes.
Since improper oral hygiene has a high probability of re-developing gingivitis, the patient is taught how to care for his teeth and individual cleaning products are selected.
Treatment of chronic gingivitis
Complex therapeutic measures for chronic gingivitis include eliminating the causes of the disease and influencing pathological foci. For this, the patient is prescribed:
- local anti-inflammatory gels and ointments;
- vitamins and means to improve blood circulation in the oral cavity;
- cleaning teeth and removing deposits;
- treatment of caries and removal of decayed teeth;
- correction of bite and other anomalies that provoke the development of gingivitis;
- electrophoresis, ultraviolet irradiation, laser therapy.
Treatment of ulcerative-necrotizing gingivitis
When deciding how to cure gingivitis in the ulcerative-necrotic form, doctors focus on a combination of local and general therapeutic measures. The patient is prescribed antibiotics, immunomodulators, antiallergic and restorative drugs, and the ulcers are cleansed and treated with wound-healing agents. An obligatory point in the treatment of gingivitis is the fight against dental plaque, which includes brushing the teeth and removing deposits. After the ulcers disappear, treatment of diseased teeth is performed.
Treatment of hypertrophic gingivitis
Hypertrophic gingivitis is treated in a similar way to catarrhal gingivitis. For the fibrous form, the same methods are used as for chronic catarrhal gingivitis, and for the edematous form, methods for treating the acute catarrhal form are used. Since in many cases conservative therapy does not give the desired effect, the patient often undergoes cryodestruction of hypertrophied papillae or their diathermocoagulation. Sometimes the indication for treatment is gingivectomy - a surgical procedure during which an overgrown area of the gum is excised.
Pathogenesis of gingivitis
In the pathogenesis of gingivitis, there are several stages that transform into one another:
- initial stage;
- early stage;
- stage of stable damage;
- progressive stage.
The initial stage of gum inflammation develops in the first 2-4 days. Polymorphonuclear leukocytes begin to fight dental plaque microorganisms. Let me remind you that these include basophils, eosinophils and neutrophils. In our case, neutrophils predominate:
They penetrate from the blood vessels into the connective tissue of the gums, the epithelium of the gingival sulcus, and the attachment epithelium. They displace and compress the collagen fibers around the vessels, releasing collagenase, which destroys them. In response to the appearance of such a large number of immune cells, capillaries dilate and blood flow increases. And, as a result, more exudate and extravascular proteins are released from the gingival sulcus - the amount of gingival fluid increases.
This stage is also called subclinical gingivitis, because outwardly the gums look absolutely healthy. Pathological changes are visible at the microscopic level:
Neutrophils (NF) in blood vessels near the junctional epithelium (JE) and even between its cells. There are no neutrophils in the gingival crevicular epithelium (GED)
1 - healthy gums. Connective tissue (CT) contains fibroblasts, blood vessels, and dense collagen fibers. 2 – after a few days of plaque accumulation. Many immune cells in connective tissue, epithelium (CE). Dilated blood vessel (CV) in the center
The body's response determines how the initial stage will end. Recovery and return to a normal state or transition to the next stage - the stage of early damage.
The initial stage becomes early after about 1 week of plaque accumulation. Other immune cells - macrophages, lymphocytes - begin to migrate into the inflammation zone, forming an infiltrate. Around such infiltrates, as well as around vessels in the initial stage, collagen is destroyed:
The appearance of lymphocytes of small (ML) and large (BL) sizes. Light spaces around them are missing collagen
Moreover, its production by fibroblasts decreases. The worst conditions are for circular (4) and dentogingival fibers (1,2,3 in the figure below).
The connective epithelium and blood vessels grow: epithelial cords appear, between which there are capillary loops. Therefore, the color of the gums changes and erythema occurs. The first clinical sign also appears - bleeding gums.
Over time (according to various sources, from 2-3 weeks to even 1-2 months), the process enters the stage of stable damage (developed). This period can already be characterized as a chronic inflammatory process in the gums. Many immune cells of previous stages (neutrophils, macrophages, lymphocytes) are destroyed. From them there is only a trace in the form of expanded intercellular spaces, granular residues and lysosomes. They are replaced by others - B lymphocytes and plasma cells. The amount of collagen continues to decrease.
Plasma cell degeneration, cellular debris (debris)
Epithelium of the gingival sulcus with increased intercellular spaces and lymphocytes
The blood vessels change significantly: they are overloaded. As a result, their fragility increases, blood circulation in them slows down, and venous stagnation occurs. The color of the gums becomes darker and cyanotic. Plus, red blood cells leave the capillaries into the connective tissue, the hemoglobin in them breaks down, this enhances the staining.
Strands in the epithelial attachment can become very pronounced. So much so that, continuing to grow in the direction of the connective tissue of the gums, they can partially destroy the basal lamina (with the help of which the epithelium is attached to the connective tissue).
The stage of sustained damage can have several scenarios:
- With one of them, the process remains stable for several months or years.
- In the other case, it is more active and causes progressive destructive lesions.
- But the most favorable path is tissue restoration thanks to successful therapy. This happens due to the return of healthy periodontal microflora, which causes the inflammatory response of immune cells to disappear.
Some authors also distinguish stage 4 of gingivitis: progressive damage. But this is already periodontitis. This stage is left and considered, because gum inflammation with the involvement of other periodontal structures (ligament, bone) does not disappear anywhere. But this is a completely different story, so we’ll limit ourselves to three.
For clarity, we can summarize the results with a table:
| Stage | Time (days) | Blood vessels | Connective and sulcus epithelium | Predominant immune cells | Collagen | Clinical signs |
| Initial | 2-4 | Dilation, inflammation, increased permeability | Infiltration of polymorphonuclear leukocytes | PMN (mainly neutrophils) | Destruction around blood vessels | Increased amount of gingival fluid |
| Early | 4-7* | Proliferation | The same + epithelial strands, atrophy zones | Lymphocytes | Destruction around infiltrates | Erythema Bleeding (probe) |
| Persistent damage (developed) | 14-21* | Same + blood stagnation, fragility | Same + progression | Plasma cells | Progressive destruction | Changes in color, size, texture, surface, etc. |
* other authors note the duration of stage II is 1-3 weeks, stage III – 1-2 months.
I hope I was able to lift the veil of mystery about the occurrence and development of gingivitis. With this knowledge, it will be easier to understand where all the clinical signs, or symptoms, of gum inflammation come from.
The inflammation itself can occur and manifest itself in different ways. Due to these features, various forms of gingivitis are distinguished.
Dental devices used in the treatment of gingivitis
Treatment of gingivitis at the Telo's Beauty clinic is carried out using modern dental devices, which allow professional diagnostics, teeth cleaning and periodontal therapy without pain and damage to tooth enamel. Thanks to the latest technologies and improved devices, the patient calmly endures any manipulation and receives quality care that previously could only be dreamed of.
| Name | Device functions |
| Estetica E50 | The dental unit is safe to use and is equipped with a wide range of attachments that allow the doctor to perform a variety of manipulations for gingivitis - teeth cleaning, restoration, restoration, caries treatment. |
| Kavo Gendex expert DC | An X-ray machine from the American company Gendex is an improved device that is highly efficient in operation and the ability to take high-quality images of the dentition. Its main advantages include a low dose of radiation and the availability of individual settings that allow the doctor to choose the shooting mode. |
| Kavo Gendex GXDP-700 | The digital x-ray system is used to diagnose gingivitis and obtain dental images in various formats, including 3D. The tomograph allows you to solve any problems in dental imaging and provides focused radiation, which significantly reduces the level of radiation received. |
| Waterlase | A dental laser is a universal device for the treatment of gingivitis, providing high-quality restoration and therapy of diseased teeth - sterilization of canals, treatment of furcation, excision of the gingival margin, etc. |
Procedure for diagnosing gingivitis
The dentist in a clinic first of all diagnoses gingivitis and determines its form. During the examination, the degree of gum damage is determined, the etiology of the disease is determined (determining the gate of infection to the site of inflammation). To do this, dentists may prescribe radiography, OPTG, computed tomography and other diagnostic tests to assess the extent of the lesions and determine the form of gingivitis.
Only after the indicated studies and the availability of a complete picture of the disease can dentists begin to treat gingivitis using certain selected treatment tactics.
Complications and consequences of gingivitis
Proper treatment and compliance with the doctor’s recommendations leads to complete recovery and elimination of the inflammatory process. But if gingivitis is ignored and delays in visiting a doctor, then over time the disease will begin to progress and affect neighboring tissues. The most common complication of the pathology is periodontitis, which entails loosening of teeth and their complete loss.
In addition, possible consequences of gingivitis are:
- gum abscess;
- infectious diseases of the jaw bones;
- transition of a simple catarrhal form of gingivitis to ulcerative-necrotic;
- hematogenous infections (glomerulonephritis, endocarditis).
Folk remedies for Vincent's stomatitis
The disease can only be treated with traditional dental medicine. Folk remedies will help complement the main treatment and speed up healing.
To relieve inflammation after dental procedures, rinsing with decoctions and tinctures based on:
- calendula;
- oak bark;
- St. John's wort;
- daisies.
Oak bark decoction
Prevention of gum disease
To prevent the occurrence of gingivitis, it is recommended to pay increased attention to oral hygiene. High-quality dental care involves thorough brushing at least twice a day using special therapeutic and prophylactic pastes. After eating, it is advisable to rinse the oral cavity with balms, which allow you to clean your teeth from food debris and stop the pathological proliferation of microbes.
Additionally, the prevention of gingivitis involves completely quitting smoking and taking calcium supplements, which will help strengthen the gums and jaw bones. You should eat well and strengthen your immune system, and avoid consuming excessively cold or hot drinks and foods. Twice a year it is advisable to visit a dentist who will perform professional teeth cleaning, remove tartar and, if necessary, treat identified diseases.
Diet for gingivitis
Since in most cases, gingivitis develops as a result of a lack of nutrients in the body, patients need to undergo vitamin therapy with the consumption of large amounts of fruits and vegetables. The greatest effect in treatment is provided by vitamins A, B, C and D, which are found in pineapples, broccoli, onions, kiwi, carrots, citrus fruits, and blackberries.
Products of plant origin that promote natural salivation and natural cleaning of teeth are beneficial for the oral cavity. To strengthen the gums and clear them of the accumulation of microbes, patients suffering from gingivitis are recommended to consume ginger, celery, sesame seeds, parsley, and dill.
During treatment, the following foods should be completely excluded from the diet:
- alcoholic and carbonated drinks;
- sour, hot and spicy dishes;
- too hot or cold food;
- solid foods (nuts, crackers and other similar products that can damage the mucous membrane).
Prices for gingivitis treatment in our clinic
The cost of services at the Telo's Beauty clinic depends on the form and degree of the disease - the sooner you seek help, the cheaper and easier it will be to cure gingivitis. In the initial stages of pathology, it is enough to get by with ultrasonic cleaning and polishing of teeth, while in later stages a complex and long-term therapeutic course will be required. In the table below, you can familiarize yourself with our prices and calculate the upcoming costs of treating gingivitis.
| Service | Cost, rub.) |
| Superficial anesthesia | 350 |
| Anesthesia using the Sleeper One device | 800 |
| Plasma injection I-PRF/ 1 tube | 5000 |
| Bone bioreconstruction /fibrin membrane APRF/ 1 tube | 6000 |
| Excision of the gingival margin (1 tooth) | 2000 |
| Relieving enamel hyperesthesia | 1500 |
| Scaling (1 tooth) – removal of hard plaque | 350 |
| Polishing restoration | 700 |
| Whitening with the Beyond Polus system | 22 000 |
| In-canal whitening | 1500 |
Professional treatment of gingivitis at the dentist of our clinic will help you quickly get rid of the disease and regain your beautiful and healthy smile!
Ulcerative gingivitis – Prices
| Services | Price |
| Periodontist consultation | 1100 rub. |
| Consultation with a periodontist with drawing up a treatment plan | 1000 rub. |
| Medicinal treatment of periodontal pockets in the area of 2 teeth | 200 rub. |
| Surgical treatment of periodontal pocket 1 tooth | 600 rub. |
| Tooth extraction according to DS: Periodontitis, with bone grafting (preparation for implantation using biomaterials) | 20,000 rub. |
| Opening a periodontal abscess | 1750 rub. |
| Flap surgery on the periodontium of one jaw without the use of biomaterials | from 3000 rub. |