Why can odontogenic sinusitis occur?
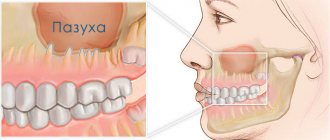
The maxillary (maxillary) sinus is a cavity with bony walls that is located inside the upper jaw. The cavity communicates with the nasal cavity through the anastomosis, which is located on the side wall of the sinus facing the nasal cavity. The lower wall has contact with the upper teeth. Quite often (in about 15% of cases) the apex of the tooth root lies directly under the mucous membrane of the bottom of the maxillary sinus, and there is no bone septum between them.
When an infection enters the maxillary sinus, inflammation of its mucous membrane or sinusitis occurs.
There are two ways of infection:
- rhinogenic - through the nasal cavity. In this case, the infection penetrates from the nasal cavity through natural or artificial (after surgery) communication;
- odontogenic - through the tooth or tissue around it.
Odontogenic sinusitis most often develops slowly against the background of chronic infection in the area of the tooth root. As a result of chronic inflammation, a cyst forms in the root area, which destroys the barrier between the sinus and the tooth. Pathogenic microbes gradually penetrate the sinus mucosa, causing inflammation.
Also, odontogenic sinusitis can occur as a result of the actions of the dentist. Often, after the removal of the upper tooth, the thin barrier between the sinus and the oral cavity may be damaged. As a result, a gateway for dental infection appears. In this case, the anatomical features of the patient with a thin bone septum between the sinus and the tooth root or its complete absence are of key importance.
Infection can occur when cleaning the canals and filling them. In some cases, the filling material gets inside the sinus, causing the formation of fungal sinusitis, and the zinc contained in the filling material promotes the growth of mold fungi (Aspergillus, Mucora). Also, odontogenic sinusitis can develop after the sinus lift procedure and the installation of dental implants in the upper jaw.
What are the maxillary sinuses
The maxillary sinuses (also called the maxillary sinuses) are special cavities on both sides of the nose that are filled with air. Each cavity is connected to the nasal passage by small openings called anastomoses. The cavities are covered with mucous membrane. The function of mucus is to trap bacteria and harmful particles in it, and then remove them from the body through those same anastomoses. When edema occurs, the excretory opening becomes very narrow, as a result of which mucus, along with harmful particles and bacteria, cannot come out and stagnates. At this time, the patient begins to experience bursting pain in the cheek area - this is how inflammation of the maxillary sinus begins. Treatment of the maxillary sinus should not be neglected, since inaction can provoke serious consequences, including sepsis and meningitis.
Classic sinusitis can be bilateral, when both sinuses are affected. In the odontogenic form, the inflammatory process starts in the sinus on which side the diseased tooth is located.
Complications
With odontogenic sinusitis, a chronic inflammatory process occurs. Dental microflora appears in the sinus, not typical for the upper respiratory tract, which can destroy bone tissue. Due to the fact that the paranasal sinuses have contact with the orbit and brain, odontogenic sinusitis can lead to severe complications:
- intraorbital (orbital phlegmon, ophthalmitis, optic nerve neuritis);
- intracranial (meningitis, encephalitis, brain abscess).
Therefore, at the slightest suspicion of this disease, you should consult a doctor.
Symptoms of perforation of the maxillary sinus
The symptoms of the disease are specific, especially if they occur after tooth root removal. In this case, the patient can note it virtually immediately after the intervention. It is as follows:
- The appearance of air bubbles in the blood that is released from the tooth socket. The number of bubbles increases with a sharp exhalation of air through the nose;
- The appearance of bloody discharge from the nose is noted. They can be scanty in nature and are detected from the side of the maxillary sinus perforated by the dentist;
- Sore throat, presence of nasal sound, the patient additionally notes a state of nasal congestion;
- Patients may also complain that they feel air passing through the hole. There may be a feeling of heaviness in the projection of the upper jaw. The oppressive feeling does not disappear, but only intensifies over time.
If such symptoms appear, you should immediately seek help from a doctor, who will examine the patient and do an X-ray examination, based on which it will be possible to judge the degree of perforation.
The dentist may suspect perforation of the maxillary sinus during implantation based on certain signs. The main one is the failure of the pin, which it is simply no longer able to strengthen at the base of the bone tissue. The doctor may also suspect the presence of pathology based on the following characteristic signs:
The appearance of small air bubbles in the hole;
- Infection of the cavity. As a rule, this happens because the diagnosis of perforation was not carried out completely or was not done completely;
- The patient complains of sharp, unpleasant and aching pain in the sinus area;
- Hypertrophy and swelling of the mucous membrane;
- The patient has difficulty breathing, with the development of an infectious process the appearance of purulent discharge.
General symptoms include fever, weakness, chills, headaches, which may accompany the inflammatory process.
Treatment
The treatment of odontogenic sinusitis requires an integrated approach. As a rule, treatment requires the simultaneous participation of an otolaryngologist and a dentist. Isolated antibacterial and conservative therapy lead only to temporary relief of the condition and removal of the severity of the process.
For a complete recovery, it is necessary to eliminate the source of infection - remove or treat the causative tooth while simultaneously sanitizing the inflamed sinus.
In case of foreign inclusions in the sinus (filling material, sinus lifting material, fungal bodies), their complete removal is necessary. For this, endoscopic techniques are used. They allow you to remove these formations through the nasal cavity. If there is a connection between the sinus and the oral cavity (oroantral fistula), it must be closed using special bioinert collagen-based membranes and mucosal flaps.
Methods for diagnosing perforation of the maxillary sinus floor
During diagnosis, a comprehensive study and analysis of the typical clinical picture observed with perforation of the maxillary sinus is used. The condition of the tooth socket, the presence of air bubbles, nosebleeds, and pain are taken into account. X-ray diagnostics are also performed, which show the area of perforation with high accuracy.
The dentist can perform a probing procedure for a perforated canal or an extracted tooth using a thin medical probe. This helps to reliably understand that there is no bone bottom in the wound. The instrument itself must pass freely through soft tissue without encountering obstacles along the way.
X-rays of the sinuses can detect characteristic darkening in the images, which are formed as a result of the accumulation of blood clots. Among other things, X-rays can show filling material, implants, and fragments of dental roots. X-rays with a contrast agent are often taken to help clearly visualize the condition of the bone tissue and surrounding tissues.
In such situations, a contrast agent is introduced into the cavity through a perforation fistula. An additional method of instrumental diagnostics is computed tomography, which determines the degree of perforation and the presence of foreign bodies, such as tooth fragments or residual filling material. If perforation is suspected, general clinical tests are required, which can show the presence of a focal infection in the patient’s body.
Treatment of the pathological process
Treatment depends on the severity of the observed pathological process. Typically, surgical intervention is not required in situations where the perforation was carried out during the extraction of a diseased tooth and was detected at the same moment. In this case, X-ray data should show the absence of an infectious process in the maxillary sinus.
If there are no fragments, filling material or infection in the wound, then in this situation the dentist tries to form a blood clot in the hole after tooth extraction and make sure that the resulting cavity is not susceptible to infection. For such purposes, a small gauze swab can be used, which is soaked in iodine solution. Iodine itself has good bactericidal properties, allowing you to quickly eliminate all pathogenic microorganisms.
Most often, such a tampon can self-fix in the resulting wound cavity after tooth extraction. Sometimes stitches are required on the gums, which are done directly by the dentist. Treatment with an iodine solution is carried out for six to seven days until granulation tissue forms, which allows the perforation to close.
The dentist can temporarily close the defect using a special hypoallergenic plate made of plastic. The plate itself is securely fixed to adjacent teeth using clasps. It carefully separates the cavities of the maxillary sinus and mouth, which in turn promotes rapid healing and regeneration of healthy tissue in the perforation area.
It is important to carry out preventive measures aimed at preventing the development of any inflammatory complications. After all, after tooth extraction during perforation, pathogenic microorganisms that can cause a serious inflammatory process can enter the wound surface.
Prevention lies in the mandatory use of anti-inflammatory drugs and antibiotics prescribed by the doctor; agents that have a vasoconstrictor effect are also used to stop bleeding.
If foreign bodies penetrate into the maxillary sinus during perforation (fragments of tooth roots, filling materials, implant perforation), treatment is carried out in a hospital setting. In severe cases, surgical interventions can be performed on the maxillary sinus with its further opening, during which tissue is cleansed and foreign bodies are removed. After sanitation, plastic closure of the resulting perforation is performed.
Old perforations that occur after tooth extraction or therapeutic treatment
If perforation was not detected after tooth extraction, the patient may attribute the discomfort to the consequences of surgery. It is worth saying that after a couple of weeks the stage of acute pain passes, and in the area of the resulting defect in the maxillary sinus, a so-called fistula appears, which connects the surface of the gum to the sinus.
This process is accompanied by symptoms characteristic of chronic sinusitis; among other things, patients complain of pain, purulent discharge from the nasal cavity, and swelling of the cheek. Treatment consists of the use of therapy aimed at stopping the inflammatory process and surgical methods that eliminate foreign bodies in the maxillary sinus.
If we summarize the above, we can say that the removal of teeth in the upper jaw, as well as their treatment, should be carried out as competently as possible. Perforation of the maxillary sinus can have quite serious consequences for the patient’s body. In some cases, long-term hospital treatment is required. The addition of an infectious process is especially dangerous.
Such a complication can be avoided if the dentist is sufficiently competent, who must take into account the anatomical position of the teeth and the maxillary sinus before performing any complex dental procedures related to the upper jaw. Based on this, the dentist is obliged to highlight all the anatomical and topographical features of the patient and conduct qualified treatment.
Before the procedure for removing, implanting or treating upper teeth, the doctor must take a targeted photo, which will help visualize the area with which he will be working. If these conditions are met, such a serious complication as perforation of the maxillary sinus can be avoided.
Old perforations
If the perforation of the maxillary sinus was not promptly identified and eliminated, then after 2-4 weeks the stage of acute manifestations will subside, and a fistula will form in the area of the defect, connecting the sinus cavity with the surface of the gum.
This process is simultaneously accompanied by symptoms of chronic sinusitis:
- constant dull pain in the sinus area radiating to the orbit and temple;
- nasal congestion on the affected side;
- purulent discharge from the nasal cavity, as well as from the fistula;
- Sometimes patients have swelling of the cheek on the side of the damaged sinus.
Most patients also complain of a sensation of air moving through the fistula when talking or sneezing, difficulty pronouncing certain sounds, and liquid food entering the nasal cavity from the mouth.
Treatment of such chronic perforations with fistulas presents some difficulties, since the presence of a chronic focus of inflammation in the maxillary sinus significantly reduces the effectiveness of therapy and quite often leads to relapse and re-formation of the fistula canal.
Such patients are indicated for surgical intervention, which includes opening the maxillary sinus with removal of all non-viable tissues and foreign bodies from its cavity, excision of the fistula and plastic closure of the defect. Antibiotics after removal of the fistula are prescribed for a course lasting 10-14 days with the simultaneous use of anti-inflammatory and antihistamine drugs, and the use of physiotherapeutic methods of treatment.
What is sinusitis?
Sinusitis is an infectious-inflammatory process in the maxillary sinus, which is the main contraindication for bone grafting. Performing a sinus lift for sinusitis is not considered possible, since the main rule of any surgical intervention is violated - maintaining asepsis (sterility).
There are two types of inflammatory process:
- Rhinogenic. The infection spreads into the sinus from the nasal passages. The viral etiology of the disease predominates, as well as bacterial agents typical for respiratory pathologies.
- Odontogenic. The cause of sinusitis is a diseased tooth located in the upper jaw. The infection penetrates through the dental roots, which are involved in the process, or by perforating the sinus with the formation of a communication between it and the oral cavity.
Sinusitis can be acute or chronic, depending on the causes and timeliness of treatment. The chronic form is characterized by the proliferation of vegetations and develops with untimely or improper treatment of acute inflammation.
Clinic
Damage to the maxillary sinuses always begins with an acute inflammatory process, which is characterized by the following symptoms:
- copious greenish nasal discharge (with bacterial infection) or scanty serous discharge (with viral etiology);
- pain in the infraorbital region, especially when changing body position;
- headache (most often forehead);
- pain in the jaw is characteristic of odontogenic sinusitis.
The pathological process can be in one or two sinuses, and the clinical picture, accordingly, is localized on the affected side. The lack of adequate treatment leads to the development of a chronic form of the disease, which is characterized by a decrease in the intensity of clinical manifestations.
X-rays of the skull help to make a reliable diagnosis, where the maxillary sinuses and their contents are clearly visualized. Normally they are completely airy.
Treatment
Therapeutic measures to eliminate the inflammatory process can be conservative or surgical. Treatment with antibacterial drugs and anti-inflammatory drugs is carried out within several days after diagnosis. In the absence of positive dynamics, an operation is performed - maxillary sinusotomy.
The essence of the manipulation is to create a hole in the wall of the affected sinus. Through it, the doctor drains the cavity (removing purulent contents) and administers medications to directly influence pathogenic agents. Such manipulation does not always require hospitalization, but lasts only a few minutes.
There is an opinion that performing a maxillary sinusotomy can lead to a chronic process, which is why patients have to constantly repeat this manipulation. The emergence of such fear is due to the fact that surgical treatment is carried out in advanced cases, when a full cure is no longer possible.
Features of the maxillary sinuses
Sinus lift surgery is closely related to the anatomy and functioning of the maxillary sinuses. Each maxillary sinus has the same structure, but has certain differences that the dentist must pay attention to when planning the operation.
There are two main types of maxillary sinus:
- Hyperpneumatized. It is a large volume cavity with increased airiness.
- Hypopneumatized. A small space characterized by sclerotic areas.
When assessing the results of radiography or computed tomography, the dentist always pays attention to the structural features of the maxillary sinus in order to accurately calculate his actions during the operation. In addition, examination of the maxillary sinus is required in order to exclude any signs of an inflammatory process, which the patient may not even be aware of.
Alternative to sinus lift for sinusitis
Modern dentistry offers several alternative methods that allow you to install implants without sinus lifting. Such surgical interventions have appeared quite recently and cannot yet be characterized by high demand and ideal results. But if a sinus lift is strictly contraindicated for a patient, then these methods can be used.
Ultra-short implants
Specific structures about 5 mm long are used, which are installed in the existing volume of bone tissue. The main disadvantage of such implants is the unnatural distribution of the chewing load, which leads to problems with their functioning. To install such a structure, a sufficient volume of the alveolar ridge is required, as well as certain characteristics of the bone tissue (it should not be too porous) for tight fixation.
Zygomatic implants
They are used only for massive restoration of the dentition. Implants are structures of about 40 mm, which are fixed at an angle into the zygomatic bone. To carry out the manipulation, general anesthesia is required in almost all cases. The operation is considered one of the most traumatic in implantology.
Basal implants
The essence of the surgical intervention is the use of a non-standard shape of implants to bypass the maxillary sinuses. Such a surgical intervention is very traumatic and dangerous with a number of complications, but it allows you to avoid an additional sinus lift procedure. Indications for the installation of basal implants are very limited.