Sometimes dentists jokingly say that they can diagnose any patient before he sits in the chair. “The wonders of X-ray vision” or unrivaled professional experience? I hasten to disappoint: neither one nor the other. The point is the widespread prevalence of periodontal diseases. And the diagnosis of “gingivitis” can be given in absentia to the vast majority without making a mistake. So, what is periodontium and what does it consist of?
The periodontium of a tooth is the tissue that surrounds it. More precisely, a complex of tissues. They are interconnected by their common location, development and functions. The structure of the periodontium has four main components:
- gum;
- periodontal ligament;
- tooth root cement;
- alveolar bone (alveolar part of the lower jaw and alveolar process of the upper).
Well, first things first. In this article we will look at the structure of the gums.
The gum is part of the oral mucosa that covers the alveolar bone (1) and surrounds the necks of the teeth (2).
The main task of the gum is to protect the tissues underneath it from mechanical and microbial damage.
Attached gum
From simple to complex: let's start with the attached gum. It is dense, elastic, firmly connected to the periosteum by collagen fibers. Wider in the incisor area (up to 4.5 mm in the upper jaw) than in the chewing teeth. Above, the attached gum borders on the marginal gum, below – on the mucous membrane of the alveolar bone. The border with the marginal gingiva is a small depression called the gingival groove (white arrow). And the mucous membrane of the alveolar bone originates at the mucogingival junction (black arrow).
Gingival sulcus
The depth of the gingival sulcus can be determined using a probe (periodontal, preferably). Normally it can be up to 3 mm. But it is worth considering that the gingival groove is not the same on different surfaces of the tooth: the approximal grooves are deeper, and they are shallower on the lingual and buccal sides. With many periodontal diseases, this depth increases (the answer to the question “why?” will be a little lower).
The gingival sulcus is lined with sulcular epithelium (or gingival sulcus epithelium). It is thin, non-keratinizing and is a kind of semi-permeable membrane for gingival fluid, on the one hand, and for microbial toxins, on the other.
Day after the procedure
At the initial stage, the hole remaining in the place of the pulled out tooth is filled with a scarlet blood clot. It is not recommended to remove it, as it performs several functions:
- protects the wound from infections;
- eliminates bleeding from blood vessels;
- promotes the formation of new tissue that will fill the empty space.
To avoid breaking up the blood clot, it is recommended not to brush your teeth on the day of surgery. Smoking is accompanied by inhalation of smoke, which creates negative pressure in the oral cavity. This may help pull the clot out of the socket. It is not recommended to blow your nose or spit. Rinsing your mouth should also be avoided; you can simply put the solution in your mouth and hold it for a while without rinsing. Gentle rinsing can be indicated only in the presence of inflammatory and purulent processes.
Gingival fluid
Gingival fluid is transudate or exudate (more protein compared to transudate) from the connective tissue of the gum and its blood vessels. Normally there is very little of it - 0.5-2 ml; with inflammation this figure increases. The composition of this liquid is very diverse:
- Microorganisms;
- Leukocytes;
- Desquamated epithelium;
- Enzymes;
- Immunoglobulins;
- Other serum and connective tissue components.
It is logical that its composition determines the functions it performs: it cleanses the gingival sulcus, has antimicrobial properties and even improves the attachment of the epithelium to the tooth.
The gingival sulcus (2) is followed by the attachment epithelium (attachment, connective) (3).
Causes of gingivitis
1) The main cause of gingivitis is microorganisms . “But there are always a lot of microbes in the oral cavity!” - you will say and you will be right. However, for gum inflammation to occur, more specific conditions are needed:
Condition once. So that these are certain microorganisms, here are these beauties:
- Streptococcus intermedius;
- Streptococcus sanguis;
- Actinomyces odontolythicus;
- Actinomyces naeslundii;
- Veilonella parvula.
Condition two. In the gingival sulcus:
| Gingival sulcus |
Both of these conditions are perfectly realized in dental plaque. It tends to accumulate in places that are difficult for a brush to reach (the gum area, for example) and creates an excellent environment in which there is little oxygen. For our microorganisms - facultative anaerobes - this is a resort.
Colored plaque. The color is especially intense in the gingival area (where there is more plaque).
These microorganisms damage the gums by:
- The toxins they produce (exotoxins);
- Toxins that are released when bacteria die (endotoxins);
- Enzymes that destroy components of the connective tissue of the gums (hyaluronidase, collagenase);
- Products of their vital activity (amines, ammonia, organic acids).
There are other reasons why gum inflammation occurs. But these reasons are rather factors that accelerate the formation of plaque and the development of bacteria or help the plaque stay longer in the oral cavity. Their other effect is a decrease in immunity (both local and general).
2) Oral factors. In more detail, this factor could be:
- small amount of saliva, its high viscosity. Teeth are less easily cleared of plaque naturally. Local immunity suffers, because saliva contains important antibacterial substances (lysozyme, immunoglobulins).
- violation of the load on the periodontium aggravates inflammation.
Such a violation occurs with an incorrect bite.
The destruction or even absence of a tooth leads to the fact that the load falls on neighboring teeth. At the same time, chewing is also impaired. Due to pain or if there is, roughly speaking, nothing to chew on one side, it becomes one-sided. Then, on the chewing side, the teeth are overloaded, and on the opposite side they are not cleaned of plaque mechanically (with solid food).
Other reasons for increased load on the periodontium:
- overbite on the filling. As a result, so-called supercontacts arise in the area of this tooth and its antagonist;
- incorrect design of the prosthesis when the supporting teeth suffer;
- abrasion of teeth.
— factors that increase plaque retention, among them:
- malocclusion, when it is difficult to reach an incorrectly positioned tooth with a brush;
- carious cavities of class II, V (proximal, cervical areas);
- The fillings that exist after treatment of these cavities are of poor quality, poorly polished. A microbial plaque will linger better on a rough surface, and cleaning such a filling with a toothbrush will not give an ideal result.
- injury to periodontal tissue disrupts its blood supply and depletes its protective forces. Mechanical damage can occur as a result of:
- anomalies of attachment of soft tissues of the vestibule of the oral cavity. These are short frenulums of the lips and tongue, pronounced buccal cords, and a small vestibule (less than 5 mm).
A short wide frenulum of the lower lip injures the periodontium of tooth 41
- incorrect movements when brushing teeth, inaccurate cleaning of interdental spaces;
3) General factors reduce our resistance to gum attack by microorganisms.
These include immunity problems, general diseases (diabetes mellitus, hypothyroidism), and certain vulnerable periods in life (pregnancy, puberty). And the omnipresent stress that accompanies every step in the modern world.
We are what we eat. This is also true for gingivitis. On the one hand, if your diet is high in carbohydrates, plaque accumulates better. On the other hand, a lack of vitamins in food worsens the body’s protective functions. Vitamin C has a special role, because if there is not enough of it, the renewal of collagen fibers suffers. And this, for a minute, is as much as 60% of the composition of the connective tissue of the gums.
And also, importantly, bad habits. The most dangerous one is smoking. It harms not only general, but also local immunity in the oral cavity. The local inflammatory response, blood supply to the gums, and the composition of the gingival fluid are disrupted, and the number of bad, pathogenic microorganisms increases.
So, we figured out the reasons. Let's take a hypothetical patient who has one or more of these. Obviously, the development of inflammation in the gums is inevitable. How does it arise, and then develop and progress? Let's figure it out.
Junctional epithelium
The junctional epithelium is a stratified squamous non-keratinizing epithelium (like the furrows). Formed during tooth eruption as a result of the fusion of the oral epithelium of the gum (1) + the primary enamel cuticle. Its length is very small - from 0.25 to 1.35 mm. Interestingly, at the apical end (the one closest to the enamel-cementum junction) its width can be only 1-2 cells. But, despite its far from impressive size, the attachment epithelium performs a number of important functions:
- it is a barrier against bacterial plaques;
- this is access of gingival fluid with protective components to the site of inflammation;
- this is a quick update (every 4-8 days), recovery from damage;
- and, finally, the ability to phagocytose epithelial cells (according to some scientists).
In the figure “Formation of the connective epithelium”: REE – primary enamel cuticle; OE – oral epithelium; JE – junctional epithelium
It is he who is destroyed by marginal gingivitis, and then by periodontitis. And it is precisely with the destruction of the attachment epithelium that the inevitable deepening of the gingival sulcus is associated (the promised answer to the question above).
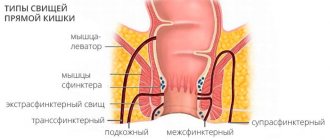
Pathologies
Factors that can trigger gum disease include mechanical damage, poor hygiene, infection, and the development of ulcers or cancer. Characteristic signs of deviation from the norm are loss of sensitivity, the formation of edema, bleeding and abundant accumulation of plaque on the surface. Common diseases include:
- Gingivitis is an inflammatory process that occurs as a result of chronic pathologies, errors in the selection of prosthetic structures, as well as tartar deposits.
- Periodontitis is an inflammation of bone tissue, often developing from a local to an extended form. It becomes the result of infection or food debris getting into the gum pockets, and, in the absence of proper treatment, leads to a weakening of the structure of the dentition.
At the first signs of abnormalities, it is recommended to undergo diagnostics at a dental clinic. Timely identification of the cause of gum disease allows comprehensive treatment to begin and helps to avoid serious consequences.
Interdental papillae
A number of authors also make interdental papillae (interdental gum) a separate point in the anatomy of the gums. This is the gum that fills the space between the teeth below their contact point. But in terms of their structure, these are all the same parts - marginal (top and edges) and attached (central part).
The shape of the interdental papilla may vary depending on the size of the interdental space. So, in the area of the incisors it is smaller - and the interdental gum there is triangular (in the photo). In molars, its shape is more like a trapezoid.
The shape of the interdental gum may also change as a result of its recession:
Or there may be no interdental papilla at all. For example, at the site of a trema or diastema, this space is tightly connected to the alveolar bone (attached gum):
Since we have sorted out the gum anatomically, it’s time to talk about its histology. Of course, it is full of its own characteristics, but in general, like any mucous membrane, it consists of epithelium and connective tissue (the lamina propria of the mucous membrane).
A small flowchart about the gingival epithelium, so as not to get confused (checkmarks on what we have already talked about):
A few words about the oral epithelium. It covers the entire gum from the tongue, cheeks and lips. That is, the outer surface of the marginal and the entire attached gingiva. It is parakeratinized, or partially keratinized (difference from completely keratinized - in the surface, stratum corneum, there are remnants of the nucleus and organelles).
All its layers are visible in the figure:
- basal (on the basement membrane);
- spiny;
- grainy;
- horny;
- connective tissue.
Cells in its composition:
- keratinocytes (epitheliocytes) – the main ones;
- melanocytes (in figure M);
- Langerhans cells (white arrow) – macrophages;
- Merkel cells – tactile receptors;
The oral epithelium is a mechanical, chemical, water and microbial barrier. On the plus side, there are more specific protective reactions: the epithelium can respond to stimuli by changing proliferation (start dividing and regenerating faster) or cell differentiation, signaling, or even death.
Histological structure
In accordance with the histological characteristics, two components are distinguished in the structure of the gums. These include stratified epithelium and connective tissue.
In the case of epithelium, the basis of the basal layer are cells in the shape of a cube or cylinder, on top of which are sequentially located spiny cells, protein grains (keratohyalin), as well as the outer stratum corneum. The structure of the latter consists of flat cellular elements that do not contain nuclei and are subject to keratinization, which leads to its periodic renewal - due to deeper layers.
The absence of nerve endings or blood vessels in the epithelium is determined by the functional task of the layer. The goal is to prevent pathogenic bacteria and microbes from entering the periodontal tissue. In this case, there is a natural barrier between the basal layer and the connective tissue base, which forms in the form of a membrane septum.
The gum's own plate is two-layered:
- The upper layer is structurally a connective tissue with a loose structure, forming papillae oriented towards the surface and extending into the epithelium. The sensitivity of the gums is caused by the passage of blood vessels, nerve endings, and the central or trigeminal nerve through them.
- The deeper layer is characterized by a mesh structure and is formed from collagen fibers produced by fibroblasts. Uniting with each other, they move into the periosteum area, due to which the gums remain immobile, and the elements of the dentition are arranged in strict sequence.
The connective substance that unites and strengthens connective tissue cells is the matrix, a product of proteoglycan and glycoprotein molecules. The supply of blood is ensured by the gum branches - the location of the capillaries close to the edge of the tissue causes increased sensitivity of these areas.