Prevention of periodontitis
Why do you need to brush your teeth?
To remove plaque and tartar and prevent various gum diseases.
Every day, a sticky film consisting of bacteria forms on the surface of the teeth, which accumulate in hard-to-reach places, especially between the teeth and at the border with the gums. This can lead to various dental diseases such as caries and periodontitis.
Dental plaque and tartar. What is the difference?
The bacterial plaque interacts with the minerals contained in the saliva and gradually hardens. This is how tartar is formed. It can be removed only with professional hygienic teeth cleaning performed by a hygienist.
Professional hygienic cleaning consists of several stages:
- plaque staining and individual hygiene consultation;
- removing plaque and tartar from the surface of teeth, cleaning periodontal pockets and interdental spaces using an ultrasonic scaler;
- restoration of natural enamel color and whitening using the Airflow method.
- polishing tooth surfaces;
- fluoridation.
What do healthy gums look like?
Healthy gums are pale pink, strong and dense. Fit tightly to the necks of the teeth. When brushing your teeth, healthy gums do not bleed.
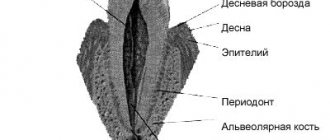
What are teeth held on to?
Each tooth has an upper (crown) part and one or more roots that go into the jaw bone, into the so-called supporting-retaining apparatus - periodontium.
How does periodontitis occur?
If you do not remove plaque from your teeth for a long time, then in the process of life, bacteria produce toxins that cause inflammation of the gums. This initial stage of inflammation is called gingivitis.
Healthy tooth
Gingivitis
Periodontitis
What are the symptoms of periodontitis?
Inflamed and bleeding gums, unpleasant taste in the mouth, the formation of pathological periodontal pockets, bad breath, gradually progressive tooth mobility.
How does inflammation develop?
When bacterial plaque grows and penetrates from the surface of the tooth into the periodontal sulcus (a small depression between the tooth and the gum), the deeper layers of the periodontium become inflamed. Pathological periodontal pockets are formed. As a result, bone tissue is involved in the inflammatory process, which leads to its destruction (resorption). The more extensive the destruction of bone tissue, the greater the mobility of the teeth, and purulent inflammation (abscess) can occur in periodontal pockets. Sometimes the gums on the destroyed bone ridge recede, exposing the roots of the teeth.
What is the daily prevention of periodontitis?
At home, you should try to remove 100% plaque from your teeth. Most people don't even realize how difficult it is to remove plaque between teeth and especially at the interface between tooth and gum. Many people skip the same place when brushing their teeth. It is in such “dead” zones that inflammation usually occurs. To avoid this, the hygienist conducts a test using an indicator to determine the places where plaque remains after brushing with a toothbrush. Under the guidance of a doctor, you can master effective dental care techniques.
Failure to see a doctor in a timely manner can lead to tooth loss! Proper oral hygiene means freshness of your breath, health of your gums and teeth! Remember that timely prevention of dental diseases will save you from expensive treatment.
Generalized periodontitis (GP) currently occupies a leading place among periodontal diseases among the population of all age groups.
According to the World Health Organization, the maximum prevalence of periodontal tissue diseases, including GP, occurs in the age category of 35-44 years.
According to some studies, from 65% to 95% of the most able-bodied population in different countries of the world suffers from periodontal diseases.
A significant proportion of these patients will eventually require surgical treatment using various osteoplastic materials to restore bone tissue.
The occurrence of functional disorders of the dentofacial system as a consequence of damage to the oral cavity is recorded 4-5 times more often than with complications of caries.
Untimely treatment and ineffective symptomatic treatment of generalized periodontitis in almost 50% of clinical cases lead to early loss of groups of teeth in able-bodied patients of relatively young age.
Complications of HP require significant financial costs and qualified dental care to fully restore chewing function.
The lack of a trend towards a reduction in the incidence of HP in Russia and post-Soviet republics dictates the need to find new methods of prevention, early diagnosis and effective treatment.
The most important criteria for successful treatment of periodontitis are the elimination of bone pockets, manifestations of the inflammatory process in the periodontium and traumatic occlusion with the achievement of long-term stable remission.
The most effective way to achieve these goals is the use of surgical treatment methods using modern osteoplastic materials, as well as the comprehensive use of additional conservative methods.
According to foreign studies, the redox balance of oral and gingival fluid plays a key role in the treatment of periodontitis in the context of maintaining the activity of natural biochemical reactions and reducing the manifestations of metabolic acidosis in periodontal tissues.
For the surgical treatment of generalized periodontitis, various types of gingivectomy, curettage, and numerous flap techniques are used. The key to success is the correct choice of techniques and materials.
Characteristics of osteoplastic materials for the treatment of periodontitis
The development of surgical treatment of HP originates from the resection technique of periodontal surgical interventions. It involved mandatory leveling of bone tissue in areas of bone pockets with excision of the soft tissue component of periodontal pockets. This resulted in excessive post-operative gum recession.
Thanks to the progress of surgical periodontology and the emergence of more modern surgical intervention techniques, the need for mechanical removal of the affected bone tissue has disappeared. Improved clinical results were achieved through more gentle sanitation of periodontal pockets and ensuring more effective reparative regeneration of bone tissue in these areas.
In the first half of the twentieth century, the famous scientists Widmann, Neumann and Cieszynski proposed a completely new surgical approach.
It involved performing flap operations with a specific type of incision and detachment of mucoperiosteal flaps to access intraosseous pockets and adequate removal of granulation tissue, subgingival dental plaque and stratified ingrown epithelium.
Complications of surgical treatment of periodontitis were serious:
- Multiple gum recessions
- Unacceptable aesthetic defects
- Tooth hypersensitivity
Due to numerous complications, especially in the areas of the frontal group of teeth, researchers almost immediately began work on a deep modification of the new technique and the search for fundamentally new solutions to the problem of GP.
Among them, the modified Widmann flap, coronally and laterally displaced flap, split flap, non-displaced flap and others appeared.
Despite obvious progress, due to the proliferation of osteoplastic materials and membranes, the resection approach began to be replaced by the regenerative concept of treatment. A technique for targeted regeneration of periodontal tissue
(SRT).
Materials for the restoration of periodontal tissues are classified by origin:
- Autogenous
- Allogeneic
- Xenogeneic
- Alloplastic
Alloplastic materials, in turn, can undergo complete or partial resorption or remain unresorbed in the defect area.
Classification depending on the severity of osteogenic potential:
- Osteoinductive
- Osteoconductive
- Osteoneutral
Some authors classify into a separate group materials that are used for targeted bone and tissue regeneration. Bone autografts of intra- or extraoral origin are classified as osteoinductive materials.
According to the concept of Boyne (1973), the optimal osteoplastic material for periodontal purposes should meet the following criteria:
- Availability in required quantities
- Promoting revascularization of the defect site
- High osteoinductive potential
- Osteoconductive properties
In addition, the ideal material should not interfere with the formation of new bone tissue, and to obtain it the patient should not undergo additional painful manipulations (excludes autografts).
Cohen et al in 2011 put forward additional requirements for osteoplastic materials for periodontal purposes:
- Lack of antigenic properties
- Resistance to microorganisms
- Preventing tooth root resorption
- Mechanical strength and elasticity
- Adaptation to the three-dimensional structure of the bone pocket
- Stimulation of new attachment formation
- Complete osteogenesis and cementogenesis
- Formation of a functional periodontal ligament
- Prevention of apical migration of epithelium
Autogenous bone tissue
in the form of bone autografts (intra- and extraoral origin) best meets these requirements. Currently, it remains the gold standard for the surgical treatment of periodontitis.
Autogenous bone tissue was previously used as an osteoplastic material characterized by a number of positive properties. It can be intraoral (bone exostoses, toothless areas of the jaw, hump of the upper jaw) or extraoral (proximal epiphysis of the tibia) of origin.
Autologous bone was used by mixing bone chips with the patient's blood in a sterile container to create a mixture to fill the bone pockets. However, such a product had a very unpleasant tendency to microbial contamination and further sequestration.
The feasibility of the clinical use of autologous bone in regenerative periodontology has been confirmed by numerous histological studies. They confirmed the ability of autogenous osteoplastic material to form new connective tissue attachment.
However, given the always limited amount of donor autologous bone, especially from intraoral sources, as well as the need for painful surgery, its use has been limited.
According to Dumitrescu, the above features should be taken into account when planning periodontal treatment in cases of multiple deep bone pockets. This limits the widespread use of autologous bone and requires the involvement of a qualified, high-profile specialist for intervention.
Therefore, a number of alternative materials were subsequently developed for the surgical treatment of generalized periodontitis. Among them were allogeneic materials, hydroxyapatite (HAP), and growth factors in combination with HAP.
However, the presence of antigenic properties, a weak osteoinductive effect, the need to create specific conditions for collecting and preserving the material, as well as the impossibility of standardization for osteogenic potential complicate their use.
When using xenogeneic osteoplastic materials
For the treatment of periodontitis, special treatment largely eliminates the antigenic effects. However, the presence of the problem of antigenic incompatibility during xenoimplantation, along with immunological incompatibility, retains the threat of material rejection.
However, despite the positive properties of xenogeneic osteoplastic materials and their wide practical application, the problem of potential prion transfer even after careful chemical treatment has not been solved.
An alternative for periodontology has become the use of inorganic and organic synthetic materials
. Among them worthy of attention:
- Synthetic hydroxyapatite
- Alpha and beta tricalcium phosphate
- Organic synthetic polymers
- Bioactive glass
- Calcium sulfate
- Calcium carbonate
- Bioceramics
Various combinations of these products with other osteoplastic materials have also gained some clinical significance.
Among the disadvantages of bioceramic materials for the treatment of HP is their ability to transform during the preparation process into hard and inelastic masses that do not facilitate rapid integration with the surrounding bone tissue.
The use of collagen in surgical periodontology is popular in many countries around the world. Combinations of highly purified collagen with sulfated glycosaminoglycans (sGAG), hyaluronic acid, hydroxyapatite and tricalcium phosphate, and autografts have been proposed.
Melcher formulated the concept of directed tissue regeneration in 1976.
Data from histological studies have demonstrated the successful formation of new connective tissue attachment in humans as a result of the use of this technique, which was first shown back in 1982.
The CTP concept has opened up exciting possibilities for clinical applications of various types of membranes
- resorbable and non-resorbable. But the presence of technical difficulties, including the occurrence of exposure (resorbable membranes) and the need to involve a qualified surgeon to prevent complications during periodontal intervention, are associated with a deterioration in their results.
Use of autologous periosteum
in periodontal practice it is a relevant method due to its high biological compatibility.
The presence of fibroblasts in the periosteum ensures the attachment of various types of undifferentiated cells to the soft tissue and the internal cambial region, which contains mesenchymal and osteoprogenitor cells.
Periosteal cells produce, under specific influence, an intercellular matrix with the subsequent formation of a membrane structure, which takes part in the formation of complete bone tissue.
The use of autologous periosteum is an effective method in the treatment of periodontal furcation defects of bone pockets and gingival recession.
The need for additional surgical intervention to collect material limits the use of the method. Therefore, Saimbi et al in 2014 proposed a new technique for transplanting autologous periosteum from a mucoperiosteal (full-thickness) flap.
Considering the peculiarities of using each of the materials for STR, the search for the most universal option for periodontal regeneration is one of the most pressing issues of modern regenerative periodontology in Russia and in the world.
According to foreign authors, the goal of treating generalized periodontitis and treating periodontal defects of any type is to achieve predictable regeneration of lost periodontal tissue.
Choosing a surgical treatment method for periodontitis
Personalized comprehensive treatment of periodontitis using therapeutic, surgical, orthodontic and physiotherapeutic methods is an effective way to achieve long-term remission.
In the 1980s, research demonstrated the formation of new connective tissue attachments through the concept of guided tissue regeneration. Karring's experimental studies have determined the role of the oral epithelium, alveolar bone, periodontal ligament and gingival connective tissue in the regeneration of periodontal tissues.
The authors showed that it is the cells of the periodontal ligament and root cement that take part in the formation of new cement on the root surface. This played an important role in the further development of therapeutic approaches and surgical techniques.
Numerous authors have concluded that successful treatment of periodontitis with a decrease in the depth of bone pockets is possible subject to complex treatment
, combining measures of professional oral hygiene, non-surgical and surgical.
Currently, much attention is paid to modern methods of conservative therapy for GP, which suggests delaying periodontal surgical interventions. This is explained by the introduction of new methods and protocols for patient management using modern devices and medications that expand the possibilities of conservative treatment of periodontitis.
Modern technologies make it possible to influence the chronic inflammatory process of periodontal tissues and their redox state, helping to achieve optimal clinical results before surgery.
Analyzing data from three decades of research, Cortellini et al showed that regular ultrasonic scaling
and smoothing of root surfaces with a periodontal pocket depth of 4-6 millimeters provides a decrease in depth by an average of 1.3 mm with an increase in the level of clinical attachment by 0.55 mm.
With a periodontal pocket depth of 7 millimeters or more, a decrease in depth is achieved within 2.15 mm with an increase in the clinical attachment index by 1.2 mm.
According to other authors, it will take 4-8 weeks to evaluate the effectiveness of the conservative phase of treatment of generalized periodontitis before moving on to the surgical phase. This is the optimal time.
Badersten et al point out that reduction in pocket depth can last up to 9 months (!), so early probing and assessment of pocket depth reduction 8 weeks after treatment may provide unreliable information, hastening the transition to the surgical phase of periodontitis treatment.
But according to other authors, the transition to the surgical phase of treatment of HP, especially in the presence of multiple deep periodontal pockets, should begin if there is no improvement in periodontal status after conservative therapy.
Despite the existence of generally accepted classical surgical techniques, the issue of choosing the optimal technique using additional methods remains poorly understood and requires further clinical research.
Schwarz et al note that the percentage of patients with pain after surgical periodontal treatment is 20-40%, which negatively affects the effectiveness of treatment of GP and further cooperation.
This fact requires the development and modification of surgical interventions aimed at minimizing pain in patients.
Many foreign authors compared different groups of surgical techniques
periodontal interventions and indicators of PC depth, level of increased clinical attachment and other indicators. Among the main compared treatment methods:
- Resection surgery
- Modified Widmann flap
- Sublingual curettage
- Scaling with smoothing of root surfaces
Summarizing the publications of Pihlstrom, Silvestri, Ramfjord and other studies, we can conclude that with a periodontal pocket depth of up to 6 mm
Ultrasonic scaling and smoothing of root surfaces is the most effective procedure.
With a periodontal pocket depth of 7 mm
The decrease in depth after surgery using the modified Widmann flap technique averaged 4.8 mm, and the level of clinical attachment was 3.3 mm.
Studies by Serino and Linghe have shown that the greatest change in clinical attachment loss can be achieved by avoiding the bone recontouring step in deep pockets and tightly suturing the periodontal wound.
Other authors obtained similar results and concluded that when the depth of the root layer is from 6 mm, it is necessary to perform flap operations after preliminary scaling with smoothing of the root surface, which reduces the depth of the root layer and increases the level of attachment to the maximum extent.
Reddy's studies have shown that de-epithelialization of the flap is a necessary step during flap operations and affects the indicators of periodontal status during treatment using the modified Widmann flap technique.
Ramfjord and Reddy compared the clinical effectiveness of the coronally advanced flap and the modified Widmann flap, finding a reduction in attachment loss after modified flap surgery.
However, numerous studies by Bosshardt and others demonstrate that there is no clinically significant improvement in the reduction of PC depth and clinical attachment loss when using such techniques.
Studies by Zamet et al have shown that the coronally advanced flap is a more effective surgical technique in reducing periodontal pocket depth compared with the modified Widmann flap. However, the technique does not improve the rate of clinical attachment loss.
Ben-Yehouda et al demonstrated a slight superiority in the effectiveness of the coronally advanced flap technique in reducing PC depth compared with the modified Widmann flap.
The results of the six-year Axellson study indicate the effectiveness and importance of providing regular maintenance therapy after the surgical phase of treatment for HP.
Histological studies by Bosshardt and Salaria demonstrated that, despite existing surgical techniques for periodontal treatment, they can result in the formation of a wide zone of ingrown epithelium with tissue recession and loss of underlying bone tissue. In this case, the speed of migration of epithelial cells into the periodontal wound exceeds the speed of migration of ligament cells.
These
and other listed points are important to consider when choosing a method of surgical treatment of HP. , along with the development of modern osteoplastic materials for the treatment , are current problems in periodontology.
Results of periodontal treatment
Doctors at a French dental clinic will help you get rid of all the listed symptoms, as well as keep your own teeth in place. The most common periodontal diseases are gingivitis and periodontitis. Periodontitis, for example, if it is severely neglected, can lead to the loss of a tooth or several teeth (and at first they will be very loose).
In very severe (advanced) cases, even intoxication of the body, destruction and degradation of bone tissue are possible. Modern methods of diagnosis, prevention and treatment of periodontal diseases used in our center, as well as a good knowledge of periodontics itself by our dentists, specialists from France, allow us to avoid all of the above dangers.
We promise that periodontal treatment at FDC
it will take a minimum of time, will be carried out completely painlessly and will definitely bring the best result.
Indications and contraindications
The need for intervention is determined by the severity of the changes that the periodontium has undergone during the development of pathology. The list of indications includes the following situations:
- The depth of the bone pockets exceeds 5 mm;
- Significant growth of granulations was diagnosed;
- Interdental tissue areas are subject to deformation;
- There are abscesses or purulent inflammations;
- Pathologies in the formation and position of tissues were identified;
- Maintaining the gap between the gum and tooth after cleaning;
- Conservative treatment methods do not give the desired effect.
Contraindications that limit the possibility of treatment are differentiated into the following categories:
- Absolute – exclude the possibility of performing an operation. Such factors include cancer and severe chronic diseases;
- Relative - viral pathologies, inflammatory processes and local defects of the jaw row, after elimination of which surgical intervention is allowed.
Surgical treatment of periodontal diseases is carried out only after diagnosis, drawing up a clinical picture and assessing the general health of the patient.
Preparation and stages of treatment
Outpatient operations require compliance with antiseptic standards and involve the use of local anesthesia. Duration is no more than two hours. The operations are quite well tolerated by the patient's body, allowing for the possibility of short-term mild discomfort in the first hours after completion of the procedure.
The list of previous events includes:
- Sanitation and hygienic cleaning of the oral cavity;
- The use of medications that localize inflammation;
- Installation of splints or orthopedic structures that fix movable units;
- The use of antibiotics that enhance the immune system.
For good gum regeneration, a soft bandage is applied. In the postoperative period, if necessary, a course of antibiotics and antiseptic drugs is also prescribed to promote recovery.
Where to contact?
Modern treatment methods used in the CELT clinic can significantly slow down the development of the disease, and often stop it for a long period. Our experts recommend regular dental examinations, which allow you to identify the disease at an early stage, but even if the disease is advanced, we will do everything to stop it.
Surgical methods for the treatment of periodontitis are selected by our specialists based on diagnostic studies and examination of the patient. Our specialist will explain the current situation to you and tell you about the treatment methods that will be optimal in your case. He will provide full information about their advantages and disadvantages, calculate the cost of treatment and answer any questions you may have.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions