Reasons for the development of pathology
The formation of an acute purulent process in the subcutaneous fat layer near the lymph nodes can be triggered by a significant decrease in immunity. If there is inflammation of the lymph node itself, then a delay in lymph outflow and increased vascular permeability are observed.
Adenophlegmons develop due to ongoing inflammatory processes of any localization. Often this pathology is diagnosed against the background of malignant tumors, some types of dermatitis, chronic dental pathologies, and inflammation of the tonsils.
Diagnostics is aimed not only at identifying adenophlegmon, but also at establishing the cause of its occurrence - medical tactics for this pathology depend on this.
Prevention of cellulitis and oral infections
The best way to avoid oral phlegmon is prevention.
- Regular visits to the dentist for professional teeth cleaning, plaque and tartar removal reduces the likelihood of caries and gum problems. Tartar causes bleeding gums, and microtraumas on the gums provide an entry point for bacteria and oral infections.
- General strengthening of the immune system, taking vitamins, and a varied diet with plenty of protein and fiber leave little chance for infections to enter the body through the oral cavity.
Symptoms of adenophlegmon of different types
Symptoms depend on where adenophlegmon developed:
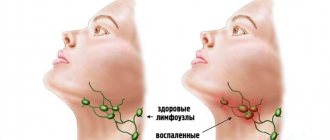
- With submandibular adenophlegmon, body temperature rises, swallowing may be difficult, problems with speech arise, swelling forms in the affected area, redness of the skin and pain when palpated are observed.
- With adenophlegmon of the neck, symptoms appear only when there is a critical accumulation of coccal microflora in the tissues of the anterior or lateral part of the neck. There is an increase in body temperature, pain when feeling the neck, redness of the skin, but swelling may be absent.
- With inguinal adenophlegmon, the clinic develops against the background of an inflammatory process in the genitourinary system. This type of adenophlegmon is characterized by rapid progression, while the patient experiences severe pain, due to which he cannot move freely. There are also signs of general intoxication of the body.
- With adenophlegmon of the axillary region, symptoms more often occur with open wounds of the upper extremities. Signs are pronounced: enlargement of regional lymph nodes, deterioration of general condition (including increased body temperature).
The symptoms for different types of pathology in question are similar, the differences lie only in the location of the lesion. If adenophlegmon occurs in children, then loss of appetite, increased drowsiness, lethargy, and lack of interest in games and others will be noted.
Symptoms of oral phlegmon
- General intoxication, weakness, high temperature, fever, chills;
- The tongue and lower jaw swell and become inactive;
- The tongue becomes so swollen that it may fall out of the mouth;
- Edema and swelling lead to distortion of facial shape;
- Pain at the base of the tongue, neck, painful sensations when chewing and swallowing;
- Gray-brown coating on the tongue;
- Unpleasant putrid odor from the mouth;
- Profuse salivation.
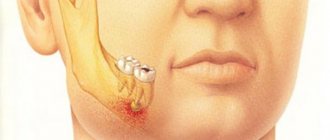
Cellulitis of the jaw develops very quickly, spreading from the affected sublingual space to neighboring areas, the floor of the mouth, and gums. With phlegmon of the lower jaw, inflammation can affect the postmaxillary and peripharyngeal space, chin, and neck.
With dental phlegmon, the symptoms are local in nature and appear against the background of untreated caries. The disease goes through several stages:
- Inflammation of dental tissue, pulpitis and periodontitis;
- Inflammation of the periosteum, swelling of the gums;
- Formation of a purulent sac on the gum.
The purulent formation grows, causes intoxication, chills, and is accompanied by bad breath. If dental phlegmon is not diagnosed in time and treatment is not started, there is a risk that the disease will spread to the entire oral cavity.
Treatment of anderophlegmon
The solution to the problem is to carry out complex treatment:
- The purulent focus is opened under local anesthesia or general anesthesia;
- it is being sanitized;
- install drainage without suturing the wound;
- apply a sterile bandage with a mandatory change once a day.
When treating adenophlegmon, antibiotics are used - not only in the form of tablets or injections, but also topically, to wash the abscess cavity. If you seek qualified medical help in a timely manner, the prognosis is favorable. But we must not forget that there is a high risk of developing sepsis.
Information about in what cases adenophlegmon of the floor of the mouth develops and what features of treatment of the disease you need to know is contained on our website https://www.dobrobut.com/.
Treatment of phlegmon
At the initial stage of the disease, drug treatment of phlegmon is possible. Anti-inflammatory therapy includes taking antibiotics and painkillers. Folk remedies, decoctions and herbal infusions are not helpful in the fight against a rapidly developing infection. Alcohol infusions are even more dangerous because... can burn the inflamed mucous membrane of the oral cavity. Do not apply heat to the affected area, because this will only provoke the development of purulent inflammation.
If it is not possible to cure phlegmon at the initial stage, the only solution is surgery. During the operation, the affected areas are excised, dead tissue is removed, and then a drain is placed at the site of suppuration. After the wound is cleared of pus, it is necessary to heal the resulting open wound.
Sutures are not used on incisions on the mucous membrane; the incisions scar quickly. But you can’t do without antibiotics and antifungal drugs in the postoperative period. If the incision was made on the outside of the jaw, sutures are placed on it after sanitation.
If the cause of phlegmon is a diseased tooth, in parallel it is necessary to treat teeth affected by caries in order to prevent the growth of foci of inflammation and the recurrence of phlegmon.
If the phlegmon caused difficulty breathing, the patient undergoes a tracheostomy: a special tube is inserted into the trachea, which supplies air directly to the lungs. After the operation, when the swelling and swelling of the larynx subsides and no longer impedes breathing, the tube is removed.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
How does APO manifest itself?
Adenophlegmon manifests itself with rapidly increasing signs of general intoxication of the body. Further on the neck, in the area where the submandibular lymph nodes are located, a tumor appears and is actively growing. This formation is painful on palpation and has a characteristic hyperemic focus in the center. Adenophlegmon is dense, this indicates the presence of fluid in its cavity (fluctuation). There are multiple small hemorrhages on the skin and mucous membranes located in close proximity to the tumor.
Untreated dental diseases are a common cause of APO
If adenophlegmon develops in children, they become tearful, weak, apathetic, refuse food and active games, and there is increased sweating. Against the background of APO, other diseases worsen in the child - diathesis, dermatitis, ARVI, etc. Sometimes adenophlegmon causes hyperthermia, the abscess can resolve outward (through the skin).
Features of children's APO
Children aged 3 to 7 years are at risk. The trigger for the development of pathology can be untreated acute osteomyelitis of the jaw. At an older age (10–14 years), adolescents are faced with adenophlegmon resulting from soft tissue injuries, followed by infection of the wound canals.
The list of main causative agents of the inflammatory process includes:
Treatment of tooth abscess
- staphylococci (white, golden);
- streptococci;
- diplococci, etc.
Important! If the baby suddenly begins to be capricious, begins to refuse to eat, complains of pain under the jaw, there is severe hyperthermia (sometimes the body temperature jumps sharply to 40 degrees) - this is a reason to immediately seek medical help from a pediatrician.
Causes of the problem
The etiology of this disease is very simple. After any infectious-inflammatory pathology (often lymphadenitis leads to APO), an immune failure occurs in the body, and the lymphatic system loses its full protective properties.
Lymph nodes become inflamed, swollen, and stop resisting pathogenic microflora, which massively attacks the body with reduced immune function. Bacteria settle in the lymph nodes, seep through their walls, enter the adipose tissue and cause an acute inflammatory process in it.
The following factors can also be “provocateurs” of APO in children and adult patients:
- soft tissue injuries of the neck;
- past infectious and inflammatory diseases;
- dental problems;
- inflammation of the lymphoid apparatus of the pharyngeal ring;
- jaw cysts;
- infection during medical procedures;
- malignant neoplasms;
- various pathologies of the excretory (genitourinary) system.
How to deal with the disease
After the diagnosis has been confirmed, the patient is sent to the hospital. Treatment of APO includes several successive stages:
- Surgical intervention. It is performed under local (adults) or general (children) anesthesia. In a situation where a tooth has become the source of infection, it is subject to extraction or depulpation (the dental canal is cleaned and a filling is placed). If necessary, an incision is made on the skin and the pus is released from the capsule - often such manipulations are not required, the contents come out on their own under internal pressure. As such, additional cleaning of the affected area is not carried out; the postoperative area is covered with a protective bandage (it is changed daily).
- Drug therapy involves taking anti-inflammatory, antibacterial, and restorative drugs.
- The wound is treated with local antiseptic solutions.
Treatment of APO is exclusively surgical - removal of pus from the capsule followed by the use of local antiseptics and systemic anti-inflammatory and antibacterial drugs. At home, in addition to traditional treatment, you can use several proven effective recipes. First of all, the action of the following compositions is aimed at strengthening the body's defenses and improving the general well-being of the patient.
Take 100 g of dry St. John's wort and 50 g of propolis, pour in 300 ml of vodka (medicinal alcohol). The mixture is poured into a glass container and sealed tightly. The medicine is infused for 7 days in a cool, dark place, filtered. When ready, the tincture is used for rinsing the mouth (the procedure is carried out at least 6 times a month, proportions - 20 g / 100 ml of warm water) and therapeutic compresses.
Compilation of anamnesis, analysis of complaints, visual examination of the patient and assessment of the results of clinical studies are components of the diagnosis of adenophlegmon
A few tablespoons of crushed dry eucalyptus leaves are poured into a thermos and steamed with boiling water and left for several hours. It is recommended to take a third of a glass of this infusion at least 4 times a day before meals. Burdock leaves are washed under running water, finely chopped, mixed with sour cream (2:1). The finished mass is applied to the affected area and left for half an hour. Manipulations are carried out daily.
Diagnostics
An appropriate diagnosis is made by a specialist based on a visual examination, anamnesis and clinical studies. Treatment of adenophlegmon is carried out exclusively in a hospital setting under the supervision of a doctor. Adenophlegmon of the neck is a dense, hyperemic, inflamed formation (tumor), painful on palpation.
A patient who comes to the doctor for a consultation voices classic complaints of general malaise, weakness, and swelling under the lower jaw. Subsequently, doctors usually discover that there were symptoms of lymphadenitis (a dense ball of varying sizes is present in the area of the lymph nodes). The doctor notes the presence of infiltration, swelling, hyperemia and other signs of APO that are accessible to visual inspection and palpation.
Important! If the lower submandibular triangle is affected by a purulent-inflammatory process, patients experience dysphagia (difficulty swallowing), problems with speech, and discomfort when opening and closing the mouth.
Adenophlegmon, localized in the submandibular region, is the most common type of this disease
Laboratory studies demonstrate an increase in ESR (indicating the presence of acute inflammation in the body), an increase in the number of neutrophils and leukocytes. It happens that APO develops within a few weeks after the patient undergoes dental treatment.
The doctor has no complaints about the condition of the teeth and gums, but under the lower jaw, a small ball appears at first, and then increases in size, a dense ball, which is also painful on palpation. Often such patients are referred to an otolaryngologist, but he also does not find any respiratory abnormalities. The cause of the pathological process and pain syndrome in this case is the same adenophlegmon under the lower jaw.
"Phlegmon of the neck"
General information about phlegmon of the neck and its ultrasound diagnosis.
Description of the disease
Diffuse purulent inflammation develops in the subcutaneous fat and is not limited to one area. The inflammatory process can spread rapidly, threatening the patient's life. Severe pathology can ultimately lead to sepsis. Therefore, when you notice the first symptoms, it is important to seek medical help.
Cellulitis most often develops as a complication of another infectious disease. In this case, the pathological microflora enters the fatty tissue from other systems of the body through the blood and lymph flow. Secondary phlegmon often develops if the patient does not adequately treat purulent processes (furunculosis, carbuncles, abscesses). In most cases, the causative agent is Staphylococcus aureus. Less commonly, other pathogenic organisms - E. coli, streptococcus, Proteus - can be detected during the diagnostic process.
Primary phlegmon develops quite rarely due to the introduction of pathogenic microorganisms into the soft tissues through wounds or cuts on the neck.
Cellulitis is severe due to diabetes mellitus. Rotting processes occur at an accelerated pace. In 10% of cases the disease is fatal.
Classification
Inflammation can occur in acute and chronic forms. In the second case, the disease is characterized by a sluggish course and the absence of acute symptoms. There are periods of remission, when any complaints are completely absent, and exacerbations, when all the symptoms characteristic of the acute form of the disease appear.
Depending on the depth of the inflammatory process, the following forms of the disease are distinguished:
- deep phlegmon (inflammation is localized under the connective membrane of the muscles);
- superficial phlegmon (pathogenic microflora develops in the subcutaneous tissue).
Depending on the location of the infection, the following types of disease occur:
- mental phlegmon;
- submandibular phlegmon (often occurs as a complication of diseases of the molars);
- phlegmon of the posterior surface of the esophagus;
- phlegmon of the sternal fossa;
- phlegmon of the anterior surface of the trachea;
Also, all phlegmons are divided into unilateral and bilateral. If we are talking about a unilateral form of the disease, there are:
- phlegmon of the back of the neck;
- phlegmon of the anterior surface of the neck;
- lateral phlegmons.
Cellulitis of the neck is a dangerous pathology that threatens life
Depending on the factors contributing to the development of the disease, the following forms of secondary phlegmon are distinguished:
- tonsillogenic (inflammatory process provoked by throat diseases);
- odontogenic (infection enters the soft tissues of the neck from diseased teeth or gums).
Based on the morphological changes occurring in the infected area, the following types of phlegmon are distinguished:
- Serous. This is the initial stage of the pathological process, which is characterized by the absence of a clear boundary between healthy and affected tissues and the formation of exudate.
- Purulent. A purulent exudate forms, the tissues swell, and a fistula may appear.
- Putrid. There is tissue destruction with the formation of gases and an unpleasant odor.
- Necrotic. In the area of inflammation, necrotic foci are formed, followed by tissue rejection. Ulcers may develop.
- Anaerobic. A secondary anaerobic infection joins the inflammatory process.
Cellulitis of newborns is another form of the disease, which is quite rare and develops at 2-3 weeks of a baby’s life. The inflammatory process is preceded by a persistent decrease in immunity. The risk of developing the disease increases if the mother experiences a bacterial infection in the last months of pregnancy.
Reasons for the development of inflammation in the neck
The disease develops as a result of penetration into the fatty tissue through a wound on the neck or through the flow of blood and lymph from other foci of infection. However, the presence of pathogenic microflora in the body does not mean that you will have to deal with phlegmon. Immunity is of great importance. If the body's defenses are working at full strength, bacteria will not be able to fully reproduce.
The following factors can become a trigger for the development of neck phlegmon:
- Diseases of the lower jaw. Foci of infection such as pulpitis, caries, periodontitis, and gingivitis can provoke infection of the soft tissues of the neck.
- Throat infections. People with chronic tracheitis, tonsillitis, pharyngitis, and laryngitis are at risk.
- Inflammation of the lymph nodes.
- Neck injuries. Through scratches and abrasions, the infection can penetrate into the deep layers of the epidermis, provoking a purulent process.
- Any infectious diseases. Pathogenic microflora enters soft tissues through the blood and lymph flow.
In some cases, phlegmon may develop not due to pathological microflora, but due to exposure to chemicals. Thus, purulent inflammation in the subcutaneous tissue of the neck will develop with the introduction of turpentine, gasoline, etc.
Symptoms
The disease in its acute form begins with a sharp increase in body temperature to 39–40 degrees. In this case, the patient has signs of general intoxication of the body:
- headache;
- reduced blood pressure;
- weakness;
- chills;
- thirst;
- sleep disturbance.
With superficial phlegmon, redness and swelling appear in the affected area. When palpating the inflamed area, the patient feels acute pain, and regional lymph nodes become enlarged. Cellulitis may be hard to the touch, and there is a local increase in body temperature (the inflamed area seems hot).
Pain at the gate of the head is one of the signs of the disease.
In deep forms of phlegmon, general symptoms are more pronounced (weakness, fever, headache, etc.). In the early stages, changes in the area of inflammation may not be noticeable. Severe pain is caused by turning the neck. The patient tries to limit his movements. As deep inflammation develops, symptoms also begin to appear in the upper layers of the epidermis. Swelling develops, the skin begins to become shiny.
If purulent masses are present inside the phlegmon, the tumor becomes loose. Pressing on the inflamed area may leave a dent. The pus forms a fistula and begins to come out or spread to neighboring tissues, aggravating the inflammation. As the affected area grows, the patient develops breathing problems due to swelling of the larynx. Body temperature can rise to 42 degrees. There is a serious risk to the patient's life.
Diagnosis of the disease
A qualified surgeon can detect superficial cellulitis during the initial examination. Deep forms of the disease require more careful differential diagnosis . In addition, it is important to identify what pathogen provokes the inflammation in order to prescribe adequate therapy.
A specialist can use the following techniques:
- Palpation of the inflamed area. Changes in the temperature of the affected area, sharp pain, absence of clear boundaries of the tumor - these symptoms indicate the development of phlegmon.
- Patient interview. The doctor clarifies when the first symptoms appeared and what preceded them. It is possible that phlegmon is a complication of a disease of the throat or oral cavity.
- General blood analysis. A change in blood composition may indicate the development of an inflammatory process.
- General urine analysis.
- Ultrasonography. The technique allows you to determine the localization of inflammation in deep forms of the disease.
- MRI of the affected area. The study also helps determine the volume and nature of inflammation. The technique is not used in all clinics due to the high cost of the equipment.
- Puncture of the inflamed area under ultrasound control. The specialist studies the obtained material and determines what pathogen provoked the inflammatory process. In accordance with the information received, medications are selected for antibacterial therapy.
Ultrasound examination of neck phlegmon.
Ultrasound examination has a number of advantages over other methods. In particular, there is the possibility of dynamic monitoring of the process, the possibility of contact between the specialist and the patient during the examination, allows for monitoring of treatment, and provides the possibility of timely controlled puncture of the object under study for the administration of medications or collection of material for research. Ultrasound does not require much time to perform and has no side effects, which emphasizes the promise of this method. Modern Doppler techniques provide the ability to assess the vascular response in the area of detected changes, while the sensitivity of the method reaches 93%. Ultrasound makes it possible to detect infiltrates and fluid accumulations that do not appear clinically in the early stages before the development of a purulent process. Ultrasound criteria for purulent tissue damage are the presence of characteristic changes in the structure of soft tissues - a decrease in their echo density with disruption of the normal anatomical structure, as well as the presence in the soft tissues of a zone of increased echo density with heterogeneous hypoechoic inclusions, as well as gas inclusions. Ultrasound makes it possible to determine the exact localization of the inflammatory focus, its depth and determination of blood flow parameters.
Ultrasound, along with high accuracy in diagnosing inflammatory changes in soft tissues, has other advantages over alternative imaging methods: it does not expose the patient and the doctor to radiation, allows monitoring the object of interest and the process of needle insertion during puncture in real time, and maintains the doctor’s contact and the patient. Ultrasound examination is most comfortable for the patient. The mobility of ultrasound devices makes it possible to use them in an operating room or intensive care unit, when it is impossible to transport the patient, for example, when performing artificial ventilation.
Intern doctor Badyukova A.A.