Description of the disease
Cellulitis of the maxillofacial area
Phlegmon is a purulent inflammation that occurs in soft tissues.
The pathological process does not have clear boundaries, which is why it quickly spreads to blood vessels, nerve endings and organs.
Phlegmon of the maxillofacial area mainly affects bone tissue and tendons, salivary glands, and muscle tissue.
Cellulitis is a dangerous pathological condition. Due to the purulent-inflammatory process, a large amount of toxic substances enter the bloodstream, which causes general intoxication of the body.
The disease is acute, characterized by the rapid development of symptoms, against the background of which the functions of the masticatory apparatus, swallowing, and breathing are impaired in patients.
Phlegmon in ICD 10
In the international classification of diseases, phlegmon of the maxillofacial area is included in the group of diseases of the skin and skin tissue (L00 - L99). The pathology is included in the block of infectious skin diseases and is designated in the ICD by code value L 03.2.
Types and classification of inflammation
An abscess occurs due to the process of decay in the lower teeth.
Inflammatory processes are divided into maxillary and mandibular (including submandibular), since their sources of origin are located in the same area.
- Maxillary abscess mainly develops due to the spread of infections from wisdom teeth. Characterized by difficulty swallowing and opening the mouth.
- An abscess of the lower jaw originates from the molars and premolars - the lower molars, causing pain when chewing and swallowing food.
- A submandibular abscess is characterized by severe swelling in the submandibular triangle, which leads to a noticeable distortion of the oval of the face.
Based on education, dental surgeons classify abscesses as follows:
- odontogenic, occurring as a result of the spread of pathogenic flora from the root of a diseased tooth (wisdom, molars, premolars);
- intraosseous are a consequence of ENT diseases (otitis, sinusitis), suppuration of cystic formations, osteomyelitis, inflammation of the periosteum;
- gingival, originating in the inflamed tissues of the gums and periodontal structures;
- salivatory, characterized by a purulent-inflammatory process in the salivary glands.
Severity:
- mild – the abscess is located in one zone;
- medium - the abscess affects several parts of the face;
- severe – the soft tissues of the neck and face, and the floor of the mouth are affected.
Most purulent inflammations affecting the maxillofacial area are odontogenic in nature, forming due to the spread of infection from diseased teeth.
Causes of phlegmon of the maxillofacial area
The causative agent of phlegmon is bacterial microorganisms: streptococci, pneumococci, staphylococci, E. coli
Cellulitis of the maxillofacial area is an infectious disease.
The causative agent is predominantly bacterial microorganisms: streptococci, pneumococci, staphylococci, E. coli.
Pathogenic microflora penetrates the subcutaneous fatty tissue through small skin lesions.
Most often the cause is odontogenic, but infection through the lymphatic or circulatory system is possible.
Anaerobic bacteria (clostridia) and non-spore-forming microorganisms (peptococci, poststreptococci) also act as pathogens.
The presented microorganisms are able to reproduce in the absence of oxygen. They cause the rapid development of necrotic processes in tissues.
Factors contributing to the development of the disease:
- Reduced immunity;
- The presence of allergies with severe skin manifestations;
- Acute or chronic tonsillitis;
- Carious lesions of teeth;
- Contact with aggressive substances under the skin;
- Furunculosis;
- Use of low-quality cosmetics;
- Failure to comply with hygiene standards.
Development mechanism
When an infection enters the subcutaneous environment, inflammation rapidly develops. The high intensity of the pathological process is explained by several factors.
These include:
- Rapid development of intoxication;
- Lack of an adequate immune response of the body;
- Decreased local immunity;
- The presence of optimal conditions for the growth of bacteria.
Due to the rapid development, granulation tissue does not have time to form, which should protect the source of inflammation from healthy tissue. Therefore, the pathological process spreads quickly.
Symptoms
Symptoms of inflammation occur quickly, which is explained by the short incubation period of bacteria
The nature of clinical manifestations varies depending on the location of inflammation.
As a rule, the pathology is acute. Symptoms of inflammation occur quickly, which is explained by the short incubation period of the bacteria.
Main features:
- High body temperature;
- Symptoms of general intoxication (nausea, vomiting, dizziness);
- Muscle weakness, tremors;
- Chills;
- Headache;
- Toothache;
- Decreased appetite;
- Pain when swallowing.
Important to remember! Local symptoms, such as swelling, swelling of the skin, redness, do not appear immediately. Therefore, the symptoms of phlegmon are often mistaken for other diseases. A distinctive feature is intense pain at the site of inflammation.
External signs
After symptoms of inflammation appear on the skin at the site of the lesion, local symptoms occur.
These include:
- Swelling;
- Change in skin color;
- Hyperemia;
- Cracks in the skin;
- Pain when moving;
- Formation of a purulent fistula.
Conventionally, the course of phlegmon can be divided into 2 stages. At the first stage, a dense formation appears under the skin, which is easily felt by palpation. At the next stage, the compaction softens, indicating the secretion of pus.
Symptoms of an abscess in the submandibular region
At the beginning of inflammation, a person experiences toothache that radiates to the gums. Then the appearance of a compaction is noted, pressure on which brings significant discomfort. Nearby tissues swell and turn red, and facial asymmetry appears. An abscess of the submandibular region can be recognized by a number of specific signs:
- constant attacks of headache, general malaise, chills;
- increase in body temperature with swelling of the affected area;
- increasing the level of leukocytes in the blood;
- the presence of purulent accumulations under the mucous membrane, looking like a reddened swelling.
If the above symptoms are present, the patient should immediately seek medical help to avoid the spread of inflammation to neighboring tissues.
Types of phlegmon
Phlegmons of the maxillofacial area in dentistry are classified depending on the location.
The main types of pathology are presented in the table below:
| Localization | Characteristic |
| Phlegmon of the temporal region | It is an inflammatory formation in the subcutaneous layer in the temple area. Accompanied by throbbing pain, the intensity of which depends on the depth of the lesion. With superficial phlegmon, severe swelling is noted. In some cases, due to temporal phlegmon, the patient cannot open his mouth normally. |
| Orbital phlegmon | The purulent-inflammatory process occurs in the fatty tissue of the orbit. In most cases, the pathology is one-sided. Accompanied by intense headaches, severe swelling of the eyelids, conjunctiva, and protrusion of the eyeball. Eye movement is limited. A significant decrease in visual acuity or its complete absence is possible. |
| Phlegmon of the subtemporal space | A purulent-necrotic process occurring in the infratemporal fossa. Occurs against the background of caries of the upper teeth. It is also possible for phlegmon to spread from the area of the upper jaw and temples. Patients experience pain above the upper jaw, which radiates to the ear, temple or teeth. |
| Phlegmon of the peripharyngeal space | Phlegmon in this area occurs against the background of carious lesions of the lower teeth and infectious diseases. Accompanied by moderate pain that is permanent. There is an increase in local lymph nodes, difficulty swallowing and opening the mouth. |
| Phlegmon of the pterygomaxillary space | The pathology is localized in the area of the pterygomaxillary fold. Phlegmon occurs mainly against the background of carious lesions and other dental diseases. Infection is also possible if antiseptic standards are not observed during torusal anesthesia. There is pronounced facial asymmetry. The patient is unable to open his mouth and swallow food normally. There is hyperemia of the mucous membrane. |
| Phlegmon of the parotid region | It occurs against the background of a purulent form of lymphadenitis, the presence of carious lesions in the upper molars. Accompanied by swelling of the tissues of the parotid region. In this case, the skin color, as a rule, does not change. There is pain when moving the jaw. |
| Phlegmon of the chewing area | Localized in the area of the masticatory muscles (cheeks). Accompanied by severe swelling, facial asymmetry, and pain. Mouth movements when chewing are limited. |
| Cellulitis of the floor of the mouth | Located in the sublingual or submandibular region. Accompanied by swelling under the tongue and pain. The patient has difficulty breathing and increased salivation. The mobility of the tongue decreases due to which speech defects occur. The tissues under the tongue acquire an unhealthy shine and turn red. |
Cellulitis of the jaw space occurs against the background of carious lesions and other dental diseases
Oral abscess - symptoms and treatment
Symptoms of oral abscesses are variable and depend directly on the type and location of the abscess. In acute purulent periostitis, patients complain of pain in the area of the causative tooth or jaw segment, swelling of the soft tissues. The face of such a patient is asymmetrical.
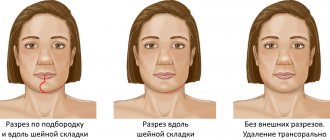
When the causative tooth is localized in the frontal part of the upper jaw, the swelling is located in the upper lip and infraorbital region, the nasolabial fold is smoothed. If the diseased tooth is located in the frontal region of the lower jaw, swelling of the soft tissues is noted in the area of the lower lip and chin. When the causative tooth is located in the lateral part of the dentition, perifocal edema (near the infectious focus) is located in the buccal region.
Acute purulent periostitis is usually not accompanied by restrictions in mouth opening. Palpation of regional lymph nodes often reveals signs of acute lymphadenitis (enlarged lymph nodes). When examining the oral cavity, the causative tooth is identified, which usually reacts sharply to tapping (percussion). This is explained by the presence of a pathological process behind the root apex. When examining the vestibule of the oral cavity, a painful inflammatory infiltrate is determined, over which there is an edematous and hyperemic (red) mucous membrane. According to the literature, periostitis is most often located on the side of the cheek or lips, less often on the palatal and lingual side [5][8].
Often abscesses of the maxillo-lingual groove, buccal region, and pterygomaxillary space are considered as a complication of acute purulent periostitis. However, in some cases these diseases develop independently, so there is no reason not to consider them in this review.
Abscess of the maxillo-lingual groove is characterized by a more serious course. The patient complains of pain when swallowing, moving the tongue to the sides, and limited mouth opening. A visual examination reveals swelling of the submandibular area and acute lymphadenitis. Examination of the oral cavity is often difficult and is only possible after blocking the motor branches of the mandibular nerve. When examining the oral cavity, acute or aggravated periodontitis of the chewing tooth of the lower jaw or difficult eruption of the lower wisdom tooth is determined. When examining the maxillo-lingual groove, its bulging is determined; upon palpation, an inflammatory, sharply painful infiltrate can be detected.
With an abscess of the pterygomaxillary space, the patient notes an increase in body temperature, pain in the pharynx, difficulty swallowing, mouth opening is limited, in some cases almost impossible. Visually, perifocal edema is often absent. An examination of the oral cavity can be carried out only after blocking the motor branches of the mandibular nerve. In the oral cavity, difficult eruption of the lower wisdom tooth is usually detected, as well as a hyperemic and edematous pterygomandibular fold.
The clinical picture of an abscess in the buccal region largely depends on the depth of the abscess. With a superficial abscess, hyperemia (redness) of the skin, a local increase in temperature, the skin is tense and does not fold. With a medium and deep location, there is pronounced swelling of the buccal area, the skin is not externally changed, it is difficult to fold into a fold. Local hyperthermia (increased temperature) is usually not observed. When the abscess is deeply located on the mucous membrane of the cheek, marks from teeth are detected.
The condition of patients with these abscesses is usually assessed as moderate. Treatment is usually carried out in a maxillofacial surgery hospital under supervision in order to prevent the development of severe complications. Patients often exhibit symptoms of general intoxication of the body (fever, headaches and muscle pain).
Diagnostic procedures
The diagnosis is made on the basis of anamnesis and external examination of the patient. The presence of acute or chronic infectious diseases is taken into account. Auxiliary diagnostic procedures are prescribed to determine the severity of the pathology.
During diagnosis, it is extremely important to determine the type of infection that provokes the pathology. This will allow further effective antibacterial treatment.
To determine the type of pathogen, a puncture biopsy is performed, during which purulent contents are collected, which are further studied in the laboratory.
Treatment
The nature of therapeutic procedures depends on the severity of phlegmon and its location. The pathology is potentially life-threatening, and therefore requires hospitalization of the patient.
Drug therapy
Treatment involves taking medications in strict accordance with the dosages prescribed by the doctor.
The following groups of drugs are used:
- Treatment involves taking medications in strict accordance with the dosages prescribed by the doctor.
Antibiotics. The action is aimed at destroying pathogenic microflora, thereby stopping the development of inflammation. Antibacterial therapy is most effective at an early stage, before tumor formation. In later stages, antibiotics are used as an adjuvant. Patients are prescribed intramuscular injections of Erythromycin, Cefuroxime and Gentamicin. On average, the duration of therapy is 3-5 days.
- Anti-inflammatory drugs. They are used to reduce tissue swelling, eliminate hyperemia, and pain. Medicines are prescribed by a doctor taking into account pharmacological interactions with antibiotics. In most cases, drugs based on Diclofenac and Nimesulide are used.
- Local antiseptics. Used for local treatment of phlegmon, which is required in the formation of a purulent fistula. For disinfection, a solution of chlorhexidine, Furacilin, and less commonly Boric acid and hydrogen peroxide are used.
Surgery
The operation can be performed during planned treatment or urgently, if the patient’s condition worsens.
Purulent phlegmon is treated surgically. The operation can be performed during planned treatment or urgently, if the patient’s condition worsens.
The presented treatment option is considered more preferable than drug therapy, as it eliminates the risk of complications and re-development of the pathology.
The main indication for surgery is the presence of an inflammatory focus and elevated body temperature of the patient.
The procedure is performed under general anesthesia. The phlegmon is opened with a wide incision, which allows for the outflow of purulent substance.
After the pus is released, the affected area is washed and disinfected. Bandages containing antibacterial ointments are applied to the incision. If the skin does not heal well, dermoplasty is performed.
Physiotherapy
The use of physiotherapeutic procedures is considered appropriate only at the early stage of pathology. Physiotherapy methods can also be used for symptomatic treatment.
Basic methods:
- UHF therapy;
- Ultraviolet irradiation;
- Light therapy;
- Ultrasonic treatment of opened phlegmon;
- Laser treatment of the wound.
Alternative medicine
Traditional methods are not recommended for use in acute illness. The use of unconventional methods is possible during the period of postoperative rehabilitation.
For better healing of affected skin, it is recommended to apply sea buckthorn or rosehip oil. For general strengthening of the body, medicines made from the herbs Eleutherococcus, Chinese magnolia vine, ginseng, and rose hips are used.
Abscess treatment methods
Drainage tubes for a diffuse abscess of the lower jaw
The goal of combating a submandibular purulent abscess is to eliminate the source of inflammation and completely restore body functions in the shortest possible period of time. This can be achieved using complex therapy. When choosing a treatment program, the maxillofacial surgeon takes into account the results of the examination (radiography in frontal and lateral projections, laboratory blood tests), as well as:
- stage of the disease;
- the rate of spread of the lesion to healthy tissues and organs;
- individual characteristics of the patient’s body: age, presence of chronic diseases, state of immunity.
The treatment program for an odontogenic jaw abscess includes taking medications, physiotherapy, and surgical intervention with the removal of a tooth that has caused the spread of pathogenic flora.
Surgical autopsy
After the operation, a course of antibiotics is indicated.
The operation is performed in a hospital setting, where the necessary equipment and instruments are available. The procedure is carried out under local or general anesthesia, taking into account the severity of inflammation, the extent of the process, the presence of contraindications to anesthesia, and the type of intervention (emergency or planned).
The mucous membrane, skin and underlying tissues are cut with a scalpel. If necrotic changes are observed, the dead fibers are carefully excised, then drained:
- special drainage tubes are inserted into the wound (polyethylene, rubber, etc.);
- wash the wound with an antiseptic, which reduces intoxication, normalizes blood counts, and accelerates the formation of granulation tissue;
- wound catheterization or packing is performed.
After the procedure, the patient is transferred to a regular ward. He is given dressings once a day. Slowly the body’s functions improve, the person begins to eat and sleep peacefully. The pain subsides, the temperature returns to normal, and the discharge of pus from the wound stops. During this period, the patient is given stitches to speed up healing.
As soon as blood counts and jaw function stabilize, the general condition improves, the patient is discharged from the hospital. He must attend physical therapy and take medications prescribed by the doctor.
Treatment with medications
Painkillers after surgery
Medications must be prescribed in advanced stages, as well as after surgical treatment. Use parenterally or internally:
- broad-spectrum antibacterial agents for 7-10 days;
- anti-inflammatory and painkillers;
- restorative and antihistamine medications;
- hyposensitizing medications and immunomodulators.
During treatment of an abscess of the upper or lower jaw, the patient is advised to eat well, take vitamins, maintain a normal drinking regime (1.5-2 liters of fluid per day), and not to overwork.
Physiotherapeutic procedures
In the postoperative period, to accelerate the removal of secretory fluid from the wound, speed its healing, and reduce the symptoms of intoxication, UHF therapy, ultrasound, laser irradiation, and ultraviolet radiation are recommended.
In the future, for general strengthening of the body, ultraviolet irradiation, EHF therapy, local and intravenous laser irradiation are indicated. During the recovery period, sessions of magnetic therapy, ultrasound, and aeroionic procedures are recommended.
Forecast
The likelihood of complications increases significantly in the absence of timely assistance
If you seek medical help in a timely manner, the prognosis is favorable.
The pathology can be successfully treated surgically, and with the help of auxiliary drug therapy, the symptoms are eliminated and the general condition of the patient is normalized.
The likelihood of complications increases significantly in the absence of timely assistance.
In such situations, phlegmon can cause conditions that threaten the patient's life.
Possible complications
Possible complications of phlegmon in the maxillofacial area include:
- Blood poisoning and septic shock;
- Impaired brain activity due to intoxication;
- Asphyxia;
- Impaired cerebral circulation due to compression of blood vessels;
- Thrombosis of the neck veins;
- Development of a brain abscess.
Important to remember! In the absence of timely treatment, phlegmon can cause a skin defect that will persist even if treatment is successful.
Odontogenic infection
Odontogenic periostitis
Depending on the clinical course, periostitis can be acute (serous, purulent) or chronic (simple, hyperplastic).
In the area of the affected tooth - the probable source of infection - pain is felt, radiating to the ear and temple. Swelling of the cheek and asymmetry of the face due to unilateral swelling of soft tissues are often visually noticeable. Difficulty opening the mouth. With odontogenic periostitis, general health suffers: weakness, febrile temperature, headache, sleep and eating disturbances. Regional lymph nodes are enlarged and painful.
Odontogenic osteomyelitis
It is more often diagnosed in men in the age group of 20-40 years, in 68% of cases it affects the lower jaw. Against the background of a pronounced intoxication syndrome, intense local pain in the tooth or diffuse pain in the entire jaw, which spreads to the corresponding half of the head, is disturbing. The configuration of the face is changed due to swelling on the side of inflammation.
There are difficulties when opening the mouth, pain when chewing and swallowing food, impaired speech function, paresthesia of the upper or lower lip. There may be a putrid odor from the mouth. The temperature curve for odontogenic osteomyelitis ranges from 37.5 to 39-40°C.
Odontogenic sinusitis
Odontogenic sinusitis accounts for 10 to 30% of all cases of infections of the maxillary sinuses. Acute sinusitis manifests itself with headache, temperature reaction, and a feeling of pressure in the projection of the corresponding sinus. Swelling of the nasal cavity increases, breathing becomes difficult, and the sense of smell decreases. After some time, a mucopurulent or purulent secretion begins to separate from the sinus. The soft tissues of the infraorbital region and cheeks look swollen.
Odontogenic abscesses and phlegmons
About 57% of purulent infections of the soft tissues of the head and neck have a dental etiology. Odontogenic abscesses are usually localized in the infraorbital, buccal, submandibular, and parotid regions. Accompanied by the appearance of swelling in the face or neck, hyperemia of the skin over the abscess. With a superficial abscess, a symptom of fluctuation is felt. There is local pain and pulsation in the projection of the abscess. Signs of intoxication are moderate.
Based on localization, odontogenic phlegmons of the floor of the mouth, submandibular, submental, peripharyngeal space, and neck area are distinguished. There is swelling of soft tissues without clear boundaries with the presence of a dense painful infiltrate. The pain is spontaneous, diffuse, and constantly present. Depending on the location of the phlegmon, chewing, swallowing, breathing, and speech are impaired. Characterized by a pronounced deterioration in general health, febrile fever, chills.
Odontogenic lymphadenitis
Usually develops in the area of the submandibular or cervical lymph nodes. They are characterized by local swelling, pain, and dense consistency. Facial asymmetry occurs. When lymph nodes become abscessed, body temperature rises, chills and malaise appear. When palpating a purulent focus, fluctuation is felt.