CLASSIFICATION
Odontogenic infections (infections of the oral cavity), depending on the anatomical location, are divided into truly odontogenic
associated with damage to tooth tissue (caries, pulpitis);
periodontal
, associated with damage to the periodontium (periodontitis) and gums (gingivitis, pericoronitis), surrounding tissues (periosteum, bone, soft tissues of the face and neck, maxillary sinus, lymph nodes);
non-odontogenic
, associated with damage to the mucous membranes (stomatitis) and inflammation of the major salivary glands.
These types of infections can cause serious life-threatening complications from the cranial cavity, retropharyngeal, mediastinal and other localizations, as well as hematogenously disseminated lesions of the heart valve apparatus, sepsis.
Purulent infection of the face and neck
may be of non-odontogenic origin and includes folliculitis, furuncle, carbuncle, lymphadenitis, erysipelas, hematogenous osteomyelitis of the jaws.
Specific infections (actinomycosis, tuberculosis, syphilis, HIV) can also be observed in the maxillofacial area.
MAIN PATIENTS
Infections of the oral cavity are associated with the microflora that is constantly present here. Usually this is a mixed flora, including more than 3-5 microorganisms.
With truly odontogenic
infections, along with facultative bacteria, primarily viridans streptococci, in particular (
S.mutans, S.milleri
), anaerobic flora is released:
Peptostreptococcus
spp.,
Fusobacterium
spp.,
Actinomyces
spp.
In case of periodontal infection, five main pathogens are most often isolated: P.gingivalis, P.intermedia, E.corrodens, F.nucleatum, A.actinomycetemcomitans
, less commonly
Capnocytophaga
spp.
Depending on the location and severity of the infection, the patient’s age and concomitant pathology, changes in the microbial spectrum of pathogens are possible. Thus, severe purulent lesions are associated with facultative gram-negative flora ( Enterobacteriaceae
spp.) and
S.aureus
.
In elderly patients and hospitalized patients, Enterobacteriaceae
spp also predominate.
In the conditions of domestic bacteriological laboratories, it is quite difficult to isolate a specific pathogen of a certain odontogenic infection. However, it seems possible to localize pathogens that play a major role in the development of oral infections in supragingival and subgingival plaque.
PRINCIPLES OF TREATMENT OF INFECTIONS OF THE ORAL CAVITY AND MAXILLOFACIAL AREA
Treatment of odontogenic infection
often limited to local therapy, including standard dental procedures.
Systemic antibacterial therapy is carried out only when odontogenic infection spreads beyond the periodontal period (under the periosteum, into the bones, soft tissues of the face and neck), in the presence of elevated body temperature, regional lymphadenitis, and intoxication.
When choosing antimicrobial therapy in a hospital setting, in cases of severe purulent infection, it is necessary to take into account the possibility of the presence of resistant strains among anaerobes such as Prevotella
spp.,
F. nucleatum
to penicillin, which determines the prescription of broad-spectrum drugs, amoxicillin/clavulanate in monotherapy or a combination of fluoroquinolone with metronidazole.
Due to increasing levels of resistance by Streptococcus
spp.
to tetracycline and erythromycin, these drugs can only be used as alternatives. Since metronidazole has moderate activity against anaerobic cocci ( Peptostreptococcus
spp.), simultaneous administration of β-lactam antibiotics is necessary to increase effectiveness.
Preventive systemic use of AMPs when performing dental procedures in the oral cavity or periodontium does not guarantee a reduction in the incidence of infectious complications in somatically healthy patients. Convincing data on the sufficient effectiveness of topical antibiotics for oral infections have not been obtained. At the same time, oral bacteria are a reservoir of determinants of resistance to AMPs. Excessive and unjustified use of antibiotics contributes to their appearance and the development of resistance of pathogenic microflora.
Complications of abscesses and phlegmon
Purulent lesions of the maxillofacial area can be complicated by the following pathologies:
Sepsis is a serious condition of the body that is caused by the penetration of a bacterial infection into the circulatory system. Treatment of such a complication is difficult due to the development of body resistance to antibiotic therapy. Sepsis is often the cause of death. Mediastenitis in the form of purulent inflammation of the tissue of the mediastinum, where the heart, lungs and bronchi are located. Meningitis . Inflammatory damage to the meninges develops as a result of the spread of purulent infection through the lymphatic and blood vessels of the head.
ODONTOGENIC AND PERIODONTAL INFECTION
PULPITIS
Main pathogens
Viridans streptococci ( S. milleri
), non-spore-forming anaerobes:
Peptococcus
spp.,
Peptostreptococcus
spp.,
Actinomyces
spp.
Choice of antimicrobials
Antimicrobial therapy is indicated only in case of insufficient effectiveness of dental procedures or spread of infection into surrounding tissues (periodontal, periosteal, etc.).
Drugs of choice
: phenoxymethylpenicillin or penicillin (depending on the severity of the disease).
Alternative drugs
: aminopenicillins (amoxicillin, ampicillin), inhibitor-protected penicillins, cefaclor, clindamycin, erythromycin + metronidazole.
Duration of use
: depending on the severity of the current (at least 5 days).
PERIODONTITIS
Main pathogens
Microflora is rarely detected in the periodontal structure and is usually S.sanguis, S.oralis, Actinomyces
spp.
In periodontitis in adults, gram-negative anaerobes and spirochetes predominate. P.gingivalis, B.forsythus, A.actinomycetemcomitans and T.denticola
are highlighted most often.
In juveniles, there is rapid involvement of bone tissue in the process, with A. actinomycetemcomitans
and
Capnocytophaga
spp.
P.gingivalis
is rarely isolated.
In patients with leukemia and neutropenia after chemotherapy along with A. actinomycetemcomitans
C.micros
is isolated , and in prepubertal age -
Fusobacterium
spp.
Choice of antimicrobials
Drugs of choice
: doxycycline; amoxicillin/clavulanate.
Alternative drugs
: spiramycin + metronidazole, cefuroxime axetil, cefaclor + metronidazole.
Duration of therapy
: 5-7 days.
For patients with leukemia or neutropenia after chemotherapy, cefoperazone/sulbactam + aminoglycosides are used; piperacillin/tazobactam or ticarcillin/clavulanate + aminoglycosides; imipenem, meropenem.
Duration of therapy
: depending on the severity of the course, but not less than 10-14 days.
PERIOSTITIS AND OSTEOMYELITIS OF THE JAWS
Main pathogens
With the development of odontogenic periostitis and osteomyelitis, S. aureus
, as well as
Streptococcus
spp., and, as a rule, anaerobic flora prevails:
P.niger, Peptostreptococcus
spp.,
Bacteroides
spp.
Specific pathogens are less commonly identified: A.israelii, T.pallidum
.
Traumatic osteomyelitis is often caused by the presence of S.aureus
, as well as
Enterobacteriaceae
spp.,
P.aeruginosa
.
Choice of antimicrobials
Drugs of choice
: oxacillin, cefazolin, inhibitor-protected penicillins.
Alternative drugs
: lincosamides, cefuroxime.
When P.aeruginosa
, antipseudomonas drugs (ceftazidime, fluoroquinolones) are used.
Duration of therapy
: at least 4 weeks.
ODONTOGENIC MAXILLARY SINUSITIS
Main pathogens
The causative agents of odontogenic maxillary sinusitis are: non-spore-forming anaerobes - Peptostreptococcus
spp.,
Bacteroides
spp., as well as
H.influenzae, S.pneumoniae
, less often
S.intermedius, M.catarrhalis, S.pyogenes
.
Isolation of S.aureus
from the sinus is characteristic of nosocomial sinusitis.
Choice of antimicrobials
Drugs of choice
: amoxicillin/clavulanate. For nosocomial infection - vancomycin.
Alternative drugs
: cefuroxime axetil, co-trimoxazole, ciprofloxacin, chloramphenicol.
Duration of therapy
: 10 days.
Symptoms
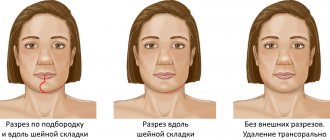
Phlegmon of the perimaxillary region, unlike an abscess, develops rapidly and is characterized by severe intoxication. Its main clinical manifestations:
- infiltration on the affected area of the face or neck;
- hyperemia, swelling, soreness of the skin at the site of inflammation;
- high body temperature;
- rapid pulse;
- severe pain when chewing, swallowing, talking;
- spasm of the muscles responsible for opening and closing the mouth (trismus);
- increased salivation;
- weakness;
- chills;
- pale skin;
- loss of appetite;
- sleep disorders;
- enlargement of regional lymph nodes;
- facial asymmetry.
Periandibular phlegmon, photos of which can frighten impressionable people, is always accompanied by an increased number of leukocytes and neutrophils in the blood, a shift in the leukocyte formula to the left and an increased ESR value. The diagnostic sign of phlegmon in the blood serum is C-reactive protein. Protein and white blood cells also appear in the urine.
PURULENT INFECTION OF SOFT TISSUE OF THE FACE AND NECK
Main pathogens
Purulent odontogenic infection of the soft tissues of the face and neck, tissue of deep fascial spaces is associated with the release of polymicrobial flora: F. nucleatum
, pigmented
Bacteroides, Peptostreptococcus
spp.,
Actinomyces
spp.,
Streptococcus
spp.
ABSCESSES, PHLEGMONS OF THE FACE AND NECK
Main pathogens
With an abscess in the orbital area in adults, a mixed flora is released: Peptostreptococcus
spp.,
Bacteroides
spp.,
Enterobacteriaceae
spp.,
Veillonella
spp.,
Streptococcus
spp.,
Staphylococcus
spp.,
Eikenella
Streptococcus
spp.,
Staphylococcus
. predominate in children .
The causative agents of abscesses and phlegmon of non-odontogenic origin, most often caused by minor skin lesions, are S.aureus, S.pyogenes
.
With putrefactive-necrotic phlegmon of the floor of the mouth, a polymicrobial flora is released, including F.nucleatum, Bacteroides
spp.,
Peptostreptococcus
spp.,
Streptococcus
spp.,
Actinomyces
spp.
S.aureus
can be isolated in patients with severe disease (more often in patients suffering from diabetes and alcoholism).
Choice of antimicrobials
Drugs of choice:
inhibitor-protected penicillins (amoxicillin/clavulanate, ampicillin/sulbactam), cefoperazone/sulbactam.
When P.aeruginosa
- ceftazidime + aminoglycosides.
Alternative drugs:
penicillin or oxacillin + metronidazole, lincosamides + aminoglycosides of the II-III generation, carbapenems, vancomycin.
Duration of therapy:
at least 10-14 days.
BUCCAL CELLULITE
Main pathogens
Usually observed in children under 3-5 years of age. The main pathogen is H. influenzae
type B and
S. pneumoniae
.
In children under 2 years of age, H. influenzae
is the main pathogen, and bacteremia is usually observed.
Choice of antimicrobials
Drugs of choice
: amoxicillin/clavulanate, ampicillin/sulbactam, third generation cephalosporins (cefotaxime, ceftriaxone) IV, in high doses.
Alternative drugs
: chloramphenicol, co-trimoxazole.
Duration of therapy
: depending on the severity of the current, but not less than 7-10 days.
LYMPHADENITIS OF THE FACE AND NECK
Main pathogens
Regional lymphadenitis in the face and neck is observed with infection in the oral cavity and face. Localization of lymphadenitis in the submandibular region, along the anterior and posterior surfaces of the neck in children aged 1-4 years, is usually associated with a viral infection.
Abscess formation of lymph nodes is usually caused by a bacterial infection. With unilateral lymphadenitis on the lateral surface of the neck in children over 4 years of age, GABHS and S.aureus
.
Anaerobic pathogens, such as Bacteroides
spp.,
Peptococcus
spp.,
Peptostreptococcus
spp.,
F.nucleatum, P.acnes
, can cause the development of odontogenic lymphadenitis or inflammatory diseases of the oral mucosa (gingivitis, stomatitis), cellulite.
Choice of antimicrobials
Drugs of choice: AMPs corresponding to the etiology of the primary source of infection.
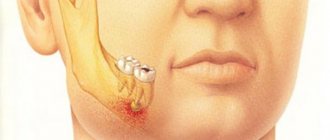
Causes and pathogenesis of abscesses and phlegmons
Most purulent lesions of the maxillofacial area are odontogenic in nature. This means that the disease is formed due to the spread of infection from the inflamed root or periodontium. In such cases, streptococci and staphylococci from the primary lesion penetrate through the lymphatic vessels into the deep layers of the soft tissues of the face.
The state of immunity is of great importance in the development of the purulent process. A decrease in the body's protective abilities is a powerful predisposing factor for tissue suppuration.
NON-ODONTOGENIC AND SPECIFIC INFECTION
NECROTIC STOMATITIS (VINCINS ULCER-NECROTIC GINGIVOSTOMATITIS)
Main pathogens
Fusobacterium is concentrated in the gingival sulcus
, pigmented
Bacteroides
, anaerobic spirochetes. With necrotizing stomatitis, there is a tendency for infection to quickly spread into surrounding tissues.
The causative agents are F. nucleatum, T. vinsentii, P. melaninogenica, P. gingivalis and P. intermedia
.
In patients with AIDS, C. rectus
.
Choice of antimicrobials
Drugs of choice:
phenoxymethylpenicillin, penicillin.
Alternative drugs:
macrolide + metronidazole.
Duration of therapy:
depending on the severity of the current.
ACTINOMYCOSIS
Main pathogens
The main causative agent of actinomycosis is A.israelii
, association with gram-negative bacteria
A. actinomycetemcomitans
and
H. aphrophilus
, which are resistant to penicillin but sensitive to tetracyclines, is also possible.
Choice of antimicrobials
Drugs of choice
: penicillin at a dose of 18-24 million units/day, with positive dynamics - transition to step-down therapy (phenoxymethylpenicillin 2 g/day or amoxicillin 3-4 g/day).
Alternative drugs
: doxycycline 0.2 g/day, oral drugs - tetracycline 3 g/day, erythromycin 2 g/day.
Duration of therapy
: penicillin 3-6 weeks IV, drugs for oral administration - 6-12 months.
Treatment of inflammatory diseases in Kaluga
If any symptoms of the above diseases occur, it is important to consult a doctor immediately. Even a day of delay can result in serious complications. An oral and maxillofacial surgeon working in our clinic will conduct a thorough examination and prescribe competent treatment. Make an appointment by phone or through the feedback form on the website.
We are always happy to help you and invite you to medical assistance! Be alert! You can make an appointment by phone; 8 (4842) 27-72-50.