When to take an antibiotic for teeth
Antibiotics are drugs that are used to treat bacterial infections.
It is important to note that we are talking specifically about bacterial diseases, not viral or fungal ones. Antibiotics are powerless against viruses or fungi. Therefore, if we are talking about a viral or fungal disease, then in such cases it is appropriate to use antiviral and antifungal drugs, respectively. Antibiotics are also used in dental practice when a tooth hurts. At the same time, it is important to understand in which cases the pain is of infectious (bacterial) origin, and in which – non-infectious.
A common type of toothache is due to pulpitis. It occurs when caries has already eroded the top layer of enamel. The resulting hole reaches the pulp of the tooth, which is why the latter begins to hurt when exposed to various irritants - thermal, chemical or mechanical. In this case, antibiotics are useless. In order to relieve pain due to pulpitis, anti-inflammatory drugs are used.
In cases where a dead tooth hurts, there is a high probability that the cause is bacteria. As you know, dead teeth (with filled canals) cannot hurt on their own. If such pain occurs, it means that bacteria have grown in the cracks or cavities of the tooth. Microorganisms multiply, infect the gums and lead to the accumulation of pus. The latter exerts pressure, which leads to pain. The above pathology is nothing more than a gumboil. The antibiotic for flux is selected by the doctor after diagnosis. After all, it is necessary to establish the type of pathogenic bacteria so that the antibiotic for flux will work for sure.
Antibiotics in dental practice are also used in the following situations:
- After surgical operations . Tooth extraction and other surgical interventions are sometimes complicated by an infectious process. To avoid bacterial infection, surgical treatment is accompanied by antibiotic therapy.
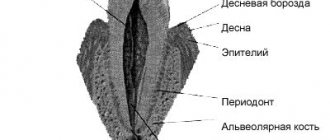
- Periodontal diseases . Advanced variants of periodontal pathologies are sometimes complicated by purulent periostitis (flux). To avoid such developments, treatment of periodontal diseases is sometimes accompanied by the use of antibiotics.
The above cases are not the only ones in which antibacterial drugs are used. These medications are prescribed by the doctor based on the clinical picture, as well as the individual characteristics of the patient. In some cases, antibiotics are also prescribed for preventive purposes - when there is a possibility of a bacterial infection. These risks are assessed by a doctor.
Indications for the use of antibiotics in dentistry
The need for treatment with antibiotics depends on the nature of the infection and the body's ability to withstand the course. The main reasons for prescribing antibiotics include:
- When advanced caries threatens pulpitis, the dentist may prescribe antibiotics to limit the spread of the pathological process. The patient is prescribed antihistamines to complement the effectiveness of antibiotics.
- With the development of an inflammatory process of periodontal tissue (periodontitis), antibiotic therapy allows the destruction of protozoa, gram-negative anaerobes in the oral cavity. Various dosage forms of drugs are used for treatment: gels, ointments, intramuscular and intravenous injections, tablets.
- The proliferation of pathogens, poor immunity, caries and dense plaque can lead to the development of gingivitis. After laboratory detection of the sensitivity of microbes to the antibiotic, a course of treatment is prescribed. Antibiotic drugs are mainly used for catarrhal gingivitis.
- The appearance of purulent accumulations inside the oral mucosa provokes the appearance of a fistula. The process occurs due to the proliferation of anaerobic gram-negative bacteria, streptococci, staphylococci, Pseudomonas aeruginosa or Escherichia coli. A doctor-prescribed course of antibiotics, which are also used for dental implantation, will help cope with the infection.
- Inflammation of the connective tissue around the root of the tooth is called periodontitis. The occurrence of the disease is a consequence of dental trauma, a complication of pulpitis, caries, or an error in dental treatment. If the process is not stopped, pus may appear. The effectiveness of antibiotics for periodontal disease is felt after preliminary cleaning of the periodontal tissue.
- The result of inflammation of various origins can be a granuloma - a cavity of granulation tissue filled with fluid. Location: on the gum near the root of the tooth. It is important to start treating granuloma in the early stages. The use of antibiotics facilitates the opening of the granulosa vesicle and suppresses the infection accumulated in it, and serves to prevent infection. Self-medication with antibacterial drugs is unacceptable.
Antibiotics for gumboil and toothache: types of drugs
Today in dental practice various antibiotics are used for gumboils and toothache. Let us remember that antibiotics are usually divided into classes. Let's look at the most popular types of antibiotics for purulent gum disease.
Nitroimidazoles
Nitroimidazoles are synthetic antibacterial drugs that exhibit high activity against anaerobic microorganisms (bacteria living in conditions without oxygen). The most popular drug in this group is metronidazole, which has been used since the 60s of the last century.
The mechanism of action of nitroimidazoles is associated with disruption of DNA replication and protein synthesis of microbial cells. Such violations are incompatible with the life of the bacterium.
Representatives of this group of antibiotics are active against most anaerobic bacteria (both gram-positive and gram-negative). Some types of protozoan microorganisms and the bacterium Helicobacter pylori are also sensitive to nitroimidazoles. The latter is the cause of the development of gastritis and gastric ulcers (as well as tumor lesions of the mucous organs of the gastrointestinal tract).
Fluoroquinolones
This is a group of drugs that exhibit antibacterial activity against a wide range of bacteria. It is noteworthy that fluoroquinolones are not considered antibiotics in the classical sense of the word. The fact is that antibiotics (even synthetic ones) always have analogues of natural origin. Fluoroquinolones have no natural analogue. The most popular representatives of fluoroquinolones include ciprofloxacin, ofloxacin, moxifloxacin, lomefloxacin, levofloxacin and others.
The mechanism of action of fluoroquinolones is reduced to inhibition of a number of important microbial enzymes. This leads to disruption of DNA synthesis and death of the bacterial cell.
Lincosamides
Lincosamides are a group of antibacterial drugs that includes antibiotics such as lincomycin and clindamycin. The mechanism of action of lincosamides is reduced to suppressing protein synthesis in bacterial walls.
Symptoms
Inflammatory processes can be asymptomatic for a long time, but at some time it becomes painful when pressing on a tooth, biting or chewing on it. Acute pain indicates a serous or purulent lesion near the tooth. It puts pressure on the surrounding tissues, the pain is felt constantly, either subsiding or worsening. When the aching pain under the crown of the tooth is short-term in nature, occurring only when the prosthetic structure is loaded or when chewing, then the inflammation has become chronic, but this does not make it any less dangerous.
Other symptoms may accompany the pain:
- swelling, redness of the gums is a clear sign of an inflammatory process;
- flux (periostitis) - swelling affects not only the gums, but the face in the area of \u200b\u200bthe inflammatory focus, the prosthetic unit and the teeth nearby ache. The purulent cavity must be opened, drained, and treated with antiseptic;
- cyst under the crown - forms near the root apex due to periodontal inflammation. Initially, a granuloma is formed, grows, becomes covered with a durable membrane of connective tissue, and transforms into a capsule with purulent contents (cyst). It grows, accompanied by pain, swelling, redness of the gums;
- formation of a fistula - the purulent contents increase in volume, a channel is formed for its outflow. In the best case, it forms in the gums, in the worst case, pus spreads deep into the tissues, affecting the jaw bone, causing osteomyelitis.
During the first days after treatment, slight pain when loading the prosthesis is a normal physiological reaction of tissues to the intervention. But if a pulpless tooth under the crown hurts for a week or more, the pain is severe and interferes with eating, sleeping, and speaking, you should immediately go to the doctor.
Antibiotics for tooth root inflammation
For toothache caused by inflammation of the tooth root, doctors also prescribe fluoroquinolones (as for gumboil). In addition, for inflammatory pathologies of the tooth root, antibiotics of the penicillin and tetracycline series are also used. Let's take a closer look at them.
Penicillins
These are the first antibiotics that were discovered by Alexander Fleming in 1928. The main mechanism of action of penicillins is bactericidal. These drugs disrupt the synthesis of peptidoglycan, a component of the bacterial cell wall. This leads to the death of the bacterium.
Currently, different types of penicillin antibiotics are used in dental practice. The most common are amoxicillin and ampicillin.
Tetracyclines
Another class of antibiotics that was discovered a long time ago - back in the 40s of the last century. Tetracyclines act against a wide range of bacteria, both gram-negative and gram-positive microorganisms. The mechanism of action of tetracyclines is inhibition of protein synthesis in bacterial cells. Microorganisms stop synthesizing vital proteins, which is why they die.
Reasons for the development of the disease
- untreated caries or poor quality of filling, when an inflammatory process has developed again under the installed filling,
- preservation of the nerve under the crown - in this case (if the tightness of the prosthesis is broken, there is inflammation underneath) there is a high risk of pulp inflammation,
- tooth injury – inflammation penetrates from the outside, i.e. through cracks and chips that are located on the root or in close proximity to it,
- exposure to aggressive stimuli - temperature and chemical, for example, during previous canal treatment, naturally, with an incorrectly selected dosage of the drug.
How long do antibiotics work for toothache?
The therapeutic effect of antibiotics occurs within the first three days. If relief does not occur during this time, then a decision is often made to prescribe another drug.
The minimum course of antibiotics is 5 days. In this case, an individual course of therapy is established for each patient depending on a number of factors.
Sometimes antibiotics do not work and the patient does not feel a therapeutic effect from taking them. Let's consider typical cases when antibacterial drugs do not work:
- Insufficient dose of medication . When carrying out antibiotic therapy, strict adherence to the dosage is an important condition. If you take less than what your doctor prescribed, there will be no effect. In other words, there was not enough active substance to suppress pathogenic flora. Please note that the dosage of the antibiotic also depends on the age and weight of the patient. The heavier the patient, the more drug is required to achieve the required drug concentration in the blood.
- Insufficient duration of therapy . Strictly adhere to the regimen and duration of taking the drug. Some patients, feeling relief, decide to interrupt the course, which makes a mistake. Premature interruption of the course of antibiotic therapy is fraught with the development of antibiotic resistance - resistance of pathogenic and opportunistic flora to antibacterial drugs.
- Some concomitant diseases . Before prescribing medications, the doctor must have comprehensive information regarding the patient’s health. It is important to inform your doctor about all chronic and recent acute diseases that may affect the effectiveness of antibiotic therapy.
- Antibiotic intolerance . The patient may have individual intolerance to some types of antibiotics. Don't despair. If one antibiotic is not suitable, then there is always an alternative antibacterial drug. Sometimes a patient has problems taking an antibiotic orally (in the form of tablets, capsules or solutions). In such cases, a decision is made to inject antibiotics, bypassing the gastrointestinal tract.
- Interaction with other active substances . The doctor must be informed about the medications the patient is taking. Some drugs cannot be taken together with antibiotics, as they neutralize the effect of the latter. In addition, drinking alcoholic beverages is prohibited during antibiotic therapy. Otherwise, the treatment will not bring the desired effect.
Why does a tooth hurt under a denture?
A crown is a prosthetic structure in the form of a cap that covers a previously prepared tooth. The cause of tooth pain under the crown in many cases is associated with poor preparation of the unit for prosthetics. Most often, this is a mistake when filling dental canals after pulp removal. The source of pain can be:
- Untreated caries
- the doctor did not remove all the affected tissue, which led to a relapse of the carious process under the crown. - Defects during
canal filling - when filling the canal with composite material, voids are formed, which are quickly populated by pathogenic microflora, which causes inflammation and pain. - Perforation of the canal wall
- when the canal walls are damaged, the filling material begins to extend beyond its boundaries, irritating the periodontium; a complication of the current inflammation can be the formation of granulomas and cysts. - Instrument fragment in the canal
- treatment is carried out with thin instruments, which may break during treatment. If the root is severely curved and difficult to pass, it is often impossible to remove the fragment. It promotes the development of inflammation, even if the canal is sealed hermetically. - Poor quality prosthetics
– the crown does not fit well to the supporting tooth or puts pressure on the gum, causing inflammation. In this case, the teeth under the crown hurt when pressing or biting. - Pulp burn
- occurs if, during the preparation of dental tissues, the doctor allowed overheating of the dentin and the neurovascular bundle hidden under it. The pulp becomes inflamed, reacts painfully to temperature stimuli, and acute pain periodically occurs, turning into aching pain.
If a tooth without a nerve hurts under the crown, this is a sign of periodontal pathology or poor-quality installation of the prosthesis. When a crown is placed on a living tooth that has not undergone depulpation, the painful syndrome, as a rule, indicates pulpitis.
What you need to know when taking antibiotics
Let's consider some facts about antibiotics that will help the patient avoid mistakes during antibiotic therapy:
- Taking antibiotics should not be combined with alcohol . Doctors prohibit drinking alcohol because alcohol increases the likelihood of side effects. It has been established that drinking alcohol during antibiotic therapy increases the likelihood of headaches, abdominal pain, tachycardia, and increased blood pressure. In addition, alcohol is an additional burden on the liver, which is already having a hard time coping with medications. Thus, drinking alcoholic beverages increases recovery time.
- Antibiotics, orange juice and milk . Few people know about this, but it is not advisable to take antibiotics with fruit juices (in particular, orange, grapefruit, apple or pineapple), as well as milk or dairy products. This is due to the fact that the above drinks impair the absorption of antibiotics. For this reason, the effectiveness of antibiotic treatment deteriorates. Therefore, after taking medications, refrain from drinking juices and milk for at least 3 hours.
- Antibiotics with meals . Some types of antibiotics should be taken on an empty stomach. For others there are no strict restrictions, and they are allowed to be taken with food. Read the medication instructions carefully and consult your doctor regarding your medication regimen.
- Medicines and antibiotics . The instructions for the antibiotic contain a list of drugs with which it is undesirable to combine it. Some combinations may weaken the effect of the antibiotic or increase the likelihood and intensity of side effects.
- Proper distribution of the antibiotic dose . The frequency of antibiotic intake per day is directly related to its effective concentration in the blood. For example, if the instructions say that the drug should be taken once a day, this means that after administration it remains effective for 24 hours. Thus, you need to take the antibiotic a second time the next day, at about the same time. If the instructions say that you need to take the drug 2 times a day, then the interval between doses should be 12 hours; if 3 times a day, the interval should be 8 hours.
What is it – tooth pulpitis?
Pulpitis is a dental term that refers to an inflammatory process that affects the nerve bundle inside the tooth - the pulp. Colloquially, the pulp is often called the nerve of the tooth. Strictly speaking, the pulp is not only nerves, but also small blood vessels, thanks to which a living tooth receives nutrients and necessary microelements. If the pulp is removed (and this often happens during the treatment of pulpitis), the tooth becomes dead and fragile because it does not receive the nutrition necessary for its full functioning and healthy condition.
The inflammatory process in the pulp never occurs on its own - there are always reasons that trigger it. Knowing the reasons why pulpitis appears is necessary and useful; this will make it possible to carry out effective prevention of this dental disease.
Take a short test and calculate the cost of treatment!
Take a short test
Adverse reactions from antibiotics
Antibiotics, like other medications, have side effects. Let's look at the most common problems that patients encounter from taking these drugs:
- Digestive problems . This is due to a disruption of the normal microflora. Antibiotics affect not only pathogenic and opportunistic flora, but also normal flora. A change in the balance of microflora leads to the development of gastrointestinal disorders. In particular, this is diarrhea, bloating, and sometimes constipation.
- Allergic reactions . After taking antibiotics, some patients experience allergic reactions. These include skin rash, runny nose, sneezing, watery eyes and swelling. In severe cases, severe allergic reactions, including anaphylactic shock, are possible. It is noteworthy that disruptions in the functioning of the immune system (and associated allergic reactions) are often a consequence of intestinal disorders. Let us remember that a huge number of intestinal bacteria are directly involved in the functioning of the immune system.
- Headache . This is a relatively common side effect of taking antibiotics. Some patients who have never previously complained of headaches experience this symptom while taking antibiotics.
- Sensitivity to the sun . While taking antibiotics, it is not recommended to sunbathe or visit solariums. This is due to the fact that some antibacterial drugs act as photosensitizers - photosensitive components. This significantly increases the likelihood of getting a burn.
- Fungal infections . Since antibiotics also suppress the normal flora of the mucous membranes, this increases the likelihood of developing fungal infections. For example, oral candidiasis (thrush) is often caused by taking antibiotics.
- Teeth staining . Another problem caused by antibiotics is tooth pigmentation. Most often, this problem is encountered by patients taking tetracycline antibiotics. In some cases, such staining is irreversible, especially in childhood.
- Other side effects . The range of adverse reactions from antibiotics is not limited to the above effects. While taking these medications, the patient may experience joint pain, double vision, problems with the liver and kidneys (due to intoxication), and even depressed mood and depression.
Causes of gum inflammation
There are many causes of gum inflammation. They can be caused by systemic and local factors. Local ones include:
- mechanical trauma to the gums during brushing;
- formation of tartar;
- eruption of wisdom teeth;
- pulpitis and caries;
- poor oral hygiene.
Painful sensations may appear due to the root of the tooth affected by pulpitis or caries. The reason for this may be dental treatment, which resulted in inflammation of the gums. It may also be associated with canal injury and poor filling.
System factors include:
- diabetes;
- diseases of the stomach and intestines;
- hormonal disbalance;
- weakened immune system;
- reaction to taking medications.
Other ways to treat dental and oral infections
The advisability of antibiotic therapy is determined solely by the doctor after diagnosis. In some cases, it is impossible to do without antibiotics, since it is not possible to get rid of the pathogenic infection in other ways.
In some cases, for inflammatory pathologies of the teeth and oral cavity, antiseptic drugs and anti-inflammatory drugs can be used. Folk remedies, for example, rinsing with herbal decoctions, have also proven themselves to be quite effective in the treatment and prevention of inflammatory diseases of the oral cavity. However, remember that traditional medicine cannot be used as the main type of treatment. They can be used as an additional measure to the main treatment.
Treatment of hyperplastic (hypretrophic) gingivitis
At the first stage, the same set of measures is provided as for catarrhal gingivitis.
If the treatment is ineffective, sclerotherapy is indicated: injections into the gingival papillae of sterile hypertonic solutions (10% calcium chloride or gluconate solution, 40% glucose solution, 90% ethyl alcohol). The administration of 0.1-0.3 ml of such solutions is carried out under local anesthesia. The injection is carried out with a thin needle from the top of the papilla to its base simultaneously in 3-4 papillae. The interval between injections is 1-2 days, the course is 4-8 injections. Pregnant women with this form of gingivitis do not undergo sclerotherapy.
Treatment of ulcerative-necrotizing gingivitis
Includes:
- relief of acute gum inflammation;
- reducing intoxication of the body, increasing the resistance of the body and periodontal tissues;
- elimination of local unfavorable factors that may contribute to the progression of the inflammatory-destructive process.
The treatment plan repeats the sequence of medical actions for other inflammatory periodontal diseases, but there are some features [10, 19, 20]:
- professional hygiene is carried out in stages under local anesthesia (applications, oral baths with lidocaine solution; if necessary, infiltration or conduction anesthesia);
- at the first visit, only supragingival dental deposits are removed;
- other local measures are carried out as the inflammatory process subsides.
It is important that both the doctor when seeing a patient and the patient at home use antiseptics that release atomic oxygen and chlorine-containing solutions, which have an adverse effect on the anaerobic microflora. Acceleration and facilitation of the removal of necrotic tissue from the surface of the gum lesion is ensured with the help of proteolytic enzymes. To optimize the epithelization of tissues (after cleansing them from a film of necrotic tissue), keratoplasty preparations are used.
Systemic (general) therapy for patients with necrotizing ulcerative gingivitis includes (Table No. 1):
- antibacterial drugs (beta-lactam antibiotics - penicillins and cephalosporins), tetracycline antibiotics, macrolides, antiprotozoal drugs (metronidazole);
- anti-inflammatory drugs;
- vitamins, adaptogens;
- hyposensitizing agents.
Criteria for assessing the effectiveness of complex treatment of inflammatory periodontal diseases can be:
- improvement of the patient’s general condition;
- relief of inflammation - in acute gingivitis;
- stabilization of periodontal status - with periodontitis;
- improvement of parameters assessed by additional research methods.
We are far from thinking that we were able to take into account and present all aspects of complex therapy, and especially drug therapy, for inflammatory periodontal diseases, and we admit that some of the materials were not included in this publication. Therefore, all constructive comments from readers will be received with gratitude.
For readers interested in this issue, we provide a list of recommended literature.
LITERATURE
- Abaev Z. M., Domashev D. I., Antidze M. K. et al. Modern methods of treatment and prevention of periodontal diseases // Dentistry. - 2012, No. 4. - P. 72-74.
- Wolf G.F., Rateitzhak E.M., Rateitzhak K. Periodontology; lane with German; edited by G. M. Barera. - M.: MEDpress-inform, 2008. - 548 p.
- Goncharova E.I. Herbal remedies in the prevention and treatment of periodontal diseases // Ros. stoma magazine. - 2012, No. 3. - P. 48-52.
- Grudyanov A.I. Periodontal diseases. — M.: Publishing house “Med. information agency", 2009. - 336 p.
- Grudyanov A.I., Aleksandrovskaya I.Yu. Planning of therapeutic measures for periodontal diseases. — M.: LLC “Med. information agency", 2010. - 56 p.
- Grudyanov A.I., Ovchinnikova V.V., Dmitrieva N.A. Antimicrobial and anti-inflammatory therapy in periodontology. — M.: LLC “Med. information agency", 2004. - 80 p.
- Periodontal diseases. Modern view on clinical, diagnostic and therapeutic aspects: study. village, recom. UMO MH&SR and Ministry of Education. RF / Yanushevich O. O., Grinin V. M., Pochtarenko V. A., Runova G. S. et al.; edited by O. O. Yanushevich. - M.: GEOTAR-Media, 2010. - 160 p.
- Krazhan D.S., Garazha N.N., Orlov M.N., Morgoeva Z.Z. Potentiated effect of antiseptics and sorbents on the microflora of periodontal pockets // Med. Bulletin of the North Caucasus. - 2012, No. 2. - P. 40-42.
- Lobko S. S., Khomenko A. I., Shadurskaya S. K., Petruk A. A. Therapeutic dentistry: Etiotropic therapy of marginal periodontal diseases: Textbook. allowance. - Mn.: BSMU, 2001. - 70 p.
- Makeeva I.M., Kudryavtseva T.V., Erokhin A.I., Akulovich A.V. Periodontal diseases: a guide. to practice therapist classes. dentistry for students IV and V courses of stoma. faculties. - MEDpress-inform, 2009. - 96 p.
- Makeeva I.M., Smirnova T.N., Chernousov A.D. et al. The use of lactoferrin in the complex treatment of dental diseases (literature review) // Dentistry. - 2012, No. 4. - P. 66-71.
- Müller H.-P. Periodontology; lane with him. - Lvov: GalDent, 2004. - 256 p.
- Patient management plans. Dentistry / ed. O. Yu. Atkova, V. M. Kamenskikh, V. R. Bosyakova. - M.: GEOTAR-Media, 2010. - 240 p.
- Platonov I. A., Andreeva T. A. Workshop and methodological guidelines on pharmacology. Part 2. Ed. prof. I. A. Platonova. - Smolensk, 2009. - 106 p.
- Modern aspects of clinical periodontology / Ed. L. A. Dmitrieva. - M.: MEDpress, 2001. - 128 p.
- Therapeutic dentistry: national. manual / ed. L. A. Dmitrieva, Yu. M. Maksimovsky. - M.: GEOTAR-Media, 2009. - 912 p.
- Filatova N.A., Elizova L.A., Chekhova N.O., Kostryukov D.A. Possibilities of achieving stabilization of the inflammatory process in periodontitis // Int. scientific-practical conf. "Achievements and prospects in dentistry." - 1999. - T. 1. - P. 257-260.
- Tsarev V.N., Ushakov R.V. Antimicrobial therapy in dentistry: Guide. — M.: Med. information agency, 2004. - 144 p.
- Tsepov L. M. Periodontal diseases: a look at the problem. - MEDpress-inform, 2006. - 192 p.
- Tsepov L. M., Nikolaev A. I., Mikheeva E. A. Diagnosis, treatment and prevention of periodontal diseases. — 3rd ed., rev. and additional - MEDpress-inform, 2008. - 272 p.
- Tsepov L. M., Nikolaev A. I., Nesterova M. M. et al. System doctor - patient - periodontal pathology: reasons for suboptimal interaction that reduces the quality of dental care // Dental South. - 2012, No. 8. - P. 28-29.
- Yudina N. A., Lyugovskaya A. V., Kurochkina A. Yu. Antimicrobial therapy in the treatment of periodontal diseases: educational method. allowance. - Minsk: BelMAPO, 2008. - 42 p.
What happens if you ignore warning signs?
If inflammation is not eliminated, over time the pathological process will destroy bone tissue, which will lead to loss of teeth. In addition, pus accumulated in soft tissues can enter the intermuscular space or subcutaneous area. This can lead to melting of nearby tissues, requiring the intervention of an oral and maxillofacial surgeon.
It is difficult to treat a prosthetic tooth; this will require unfilling the canals, conducting anti-inflammatory therapy, and filling the canals again. If the inflammation has affected the root apex, surgical intervention will be required - resection of the apex along with the granuloma or cyst.
The doctor decides how to relieve pain under the crown individually in each clinical situation, based on the cause, stage, and extent of inflammation. Sometimes the situation goes so far that the only effective treatment method is the removal of a tooth followed by prosthetics.