Stomatitis: how to overcome the “language barrier”?
Stomatitis on the tongue is just one of the manifestations of this “popular” disease. There are a huge number of reasons for its appearance, as well as ways to treat it.
There are several types of stomatitis, when it manifests itself specifically on the tongue: glossitis, viral stomatitis, vesicular stomatitis, enteroviral vesicular stomatitis, catarrhal stomatitis, fungal stomatitis, etc.
In general, stomatitis on the tongue is most common. Its notable feature is small ulcers, from which the patient suffers greatly. If inflammation is observed only on the tongue, and, for example, there are no signs of stomatitis on the palate, cheek or gum, then this disease is called glossitis.
Causes, symptoms and types of stomatitis on the tongue
Modern medicine has a huge variety of causes of stomatitis. As a rule, they are either bacterial or viral in nature. Not only adults, but also children can suffer from stomatitis on the tongue. Here are the most common causes of stomatitis on the tongue:
- Infectious diseases: diphtheria, influenza, scarlet fever, measles, acute respiratory infections. Such diseases are usually accompanied by acute stomatitis. Its development is facilitated by constant irritation of the mucous membrane during smoking, alcohol abuse, and regular consumption of too cold, hot or spicy foods. Among stomatitis caused by infection, herpetic stomatitis (herpetic sore throat) or stomatitis in the throat is distinguished. It is caused by various enteroviruses. In addition to stomatitis in the throat, this virus can cause enteroviral vesicular stomatitis with exanthema, acute hemorrhagic conjunctivitis, and aseptic (serous) meningitis. If you suspect that you have stomatitis in the throat or herpetic sore throat (white or grayish-yellow blisters in the throat), contact your doctor immediately to clarify the diagnosis.
- Diseases of the digestive system and stomach.
- Bad habits.
- Dental damage: tartar, caries, periodontitis, bleeding gums.
- Various types of damage: mechanical or chemical. For example, low-quality dentures, chipped teeth. Such violations can lead, first of all, to the appearance of stomatitis on the lip. The thin, delicate skin of this area is injured (burn, chapping, etc.), through microcracks in the thin and delicate skin of this area, an infection enters the body, causing stomatitis on the lip.
- Worm infestation.
- Weakened immunity, vitamin deficiency.
Characteristic signs that you have stomatitis are a white-yellow coating. Then gray spots appear on the tongue, reaching up to 0.5 mm in diameter. Sometimes they change shape or merge into one large spot. By the way, they may not hurt or bother you at all, and ulcers may not appear either. But, nevertheless, even if there are no pronounced symptoms of stomatitis, treatment is necessary, otherwise stomatitis can become acute. In addition, the lack of proper and timely treatment can provoke recurrent stomatitis - an inflammatory disease of the oral cavity that is chronic, but has periods of remissions and exacerbations. Sometimes it occurs as an independent disease.
One of the common manifestations of stomatitis in both children and adults is severe swelling of the tongue, which thickens and becomes covered with ulcers. After epithelial detachment, red, atrophied areas of skin remain, which cause a burning sensation. It becomes painful to eat and talk. One of the symptoms of the disease in a child is often tearfulness, moodiness, and restless behavior. If they appear, you should immediately consult a doctor. As a rule, stomatitis in children develops much faster and more painfully.
There are several types of stomatitis on the tongue:
- Catarrhal: characterized by high fever and profuse salivation, and may cause bad breath.
- Aphthous: the appearance of small ulcers (aphthous) that are covered with a yellowish coating.
- Ulcerative-necrotic: characterized by the appearance of ulcers covered with a gray coating.
Local treatment of erosive and ulcerative lesions of the oral mucosa
S. I. Tokmakova Doctor of Medicine, Professor, Head of the Department of Therapeutic Dentistry, Altai State Medical University (Barnaul)
T. N. Ulko Ph.D., Associate Professor, Department of Therapeutic Dentistry, Altai State Medical University (Barnaul)
O. V. Bondarenko Ph.D., Associate Professor, Department of Therapeutic Dentistry, Altai State Medical University (Barnaul)
O. V. Sysoeva Candidate of Medical Sciences, Associate Professor of the Department of Therapeutic Dentistry, Altai State Medical University (Barnaul)
Among the pathological processes localized on the oral mucosa (OM) and the red border of the lips, erosive and ulcerative lesions in leukoplakia and lichen planus (LP) occupy a special place. This is due to the fact that when treating them, a practitioner often has to deal with difficulties associated with the presence in patients of a long, persistent course of these diseases with frequent relapses [1, 3, 6, 7].
Complex treatment of this pathology includes measures aimed at reducing pain, relieving inflammation and accelerating regeneration processes after the maximum possible elimination of causative factors. However, the possibility of using medication and physiotherapeutic treatment in these patients is often limited due to the presence of concomitant general somatic diseases.
The relevance of the problem is also determined by the fact that this type of lesion has a significant prevalence (in the population of Barnaul in various age groups it ranges from 2 to 28% of cases) and is classified as an optional precancer with a high incidence of malignancy [1, 3—6]. This requires oncological alertness of the doctor and increased efficiency and timeliness of treatment. The experience of using a complex ointment developed at the Moscow State Medical University (2005) for the treatment of chronic lip diseases is interesting [2].
Purpose of the study
To evaluate the clinical effectiveness of using a complex ointment in the complex treatment of erosive and ulcerative lesions of the oral mucosa with leukoplakia and lichen planus.
Material and methods
Clinical studies were carried out from 2008 to 2011 at the Department of Therapeutic Dentistry of ASMU. Under observation were 35 patients diagnosed with K.13.2 “leukoplakia” (20 people) and L.43 “lichen planus of the oral mucosa, erosive-ulcerative form” (15 people).
During the clinical examination of patients, the presence of past and concomitant diseases, bad habits, and occupational hazards was revealed during the interview process. In addition, attention was paid to allergic status and heredity. The duration of the disease, the nature of the complaints, as well as the time of onset of the first symptoms were determined. They found out whether treatment was carried out for this disease and what its effectiveness was.
Examination and palpation of the maxillofacial area included determination of color, integrity, skin turgor, condition of the skeletal and muscular system, and regional lymph nodes. When assessing the state of the oral mucosa, we paid attention to the architectonics, color, moisture, and the presence of pathological elements. The condition of periodontal tissues, teeth, the presence of dissimilar metals was determined, and traumatic factors were identified.
Dental examination of the oral mucosa was performed using a “Visioner 21A” light stomatoscope from Morita Corporation (Japan) at a magnification of 10 to 40 times. Signs of malignancy were excluded visually and by palpation; if necessary, the patient was referred to an oncologist to clarify the diagnosis.
The study of the medical history of the examined patients, the results of laboratory tests, and advisory opinions made it possible to establish the background diseases accompanying the erosive-ulcerative form of leukoplakia and PL. All patients had pathology of the gastrointestinal tract (100%) and nervous system (100%). Three patients suffered from diseases of the cardiovascular and endocrine systems (9%).
To assess the timing of pain disappearance, we used the pain index (PIB) according to the Hossli-Bergman scale. The assessment was made in points from 0 to 4 before and after treatment: no pain - 0 points, mild pain - 1 point, moderate pain - 2 points, severe pain - 3 points, unbearable pain - 4 points.
The treatment plan included sanitation of the oral cavity, professional hygiene, and elimination of traumatic factors. Patients were advised to give up bad habits: smoking, drinking alcohol, biting lips and cheeks.
After local elimination of traumatic factors, treatment of erosive and ulcerative lesions was carried out according to the following scheme:
- Application anesthesia (gel “Kamistad”, “Cholisal”, “Lidochlor”, pyromecaine ointment 5%, etc.).
- Applications of proteolytic enzymes (0.1% solution of trypsin or chymotrypsin).
- Treatment with antiseptics (0.05% chlorhexidine solution, 1% iodinol solution, herbal decoctions, etc.).
- Application of a complex ointment developed at Moscow State Medical University (2005).
Composition of complex ointment:
- Sol. Retinoli acetatis olesae - 1.0
- Sol. Tocopheroli olesae - 1.0
- Thiamini bromidi - 0.2
- Insulini acropidi - 3.0
- Ung. Celestodermi - 30.0
- Ung. Solcoseryli - 20.0
- Mf unguentum
- DS For applications to the oral mucosa.
The components included in the ointment had a complex effect on various parts of the pathogenesis of diseases. An oil solution of vitamin A, when applied topically, stimulates epithelization processes, and when taken orally, helps normalize the condition of the epithelium. A solution of tocopherol acetate is an antioxidant, promotes protein synthesis, cell proliferation and acceleration of reparative processes, and also improves neurotrophic processes. Vitamin B1 normalizes the functions of the nervous system and improves local trophism. Insulin, when applied topically, helps loosen membranes and prolongs the effect of other components of the ointment. Celistoderm has anti-inflammatory and antipruritic effects. Solcoseryl improves metabolic processes, accelerates tissue regeneration, especially with neurotrophic lesions, and also has an angioprotective effect.
results
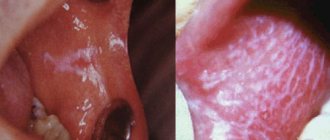
When studying the clinical picture before treatment in patients in the oral cavity, erosions and ulcers measuring from 0.5 to 2.2 cm were determined against the background of edematous, hyperemic mucosa with papules merging into a mesh pattern (43% of cases), against the background of flat foci (31% of cases). ) or verrucous leukoplakia (26%). The most common location of erosive and ulcerative lesions was the mucous membrane of the cheeks and tongue, less often the gingival margin and floor of the mouth (Fig. 1).
Rice. 1. Erosion and ulcers of the tongue with leukoplakia (before treatment).
Skin rashes characteristic of LP were present in 3 patients (20%). Dental examination revealed alternating areas of hyperemia and hyperkeratosis with epithelial defects. The surface relief of the oral mucosa was smooth or finely lumpy, keratinization of varying degrees of severity, angioarchitecture in the form of specks, stripes and loop-shaped vessels.
After a course of treatment using applications of a complex ointment, initial epithelization was observed in all patients on the 2nd day. Patients noted a decrease in pain when eating and an improvement in their general condition. After 3 days, the pain completely disappeared (Fig. 2), and after 1.5 weeks, complete epithelization of the mucous membranes was observed (Fig. 3).
Rice. 2. Epithelization of erosions and ulcers of the tongue in leukoplakia (on the 4th day of treatment). Rice. 3. Condition of the tongue 1.5 weeks after treatment of leukoplakia.
Dentoscopically, a smooth relief was noted on the oral mucosa, there was no keratinization, and the vascular architecture was presented in the form of speckles and stripes.
To increase local immunity and prevent relapses, patients were prescribed the topical immunostimulating drug Imudon, 6-8 tablets per day sublingually for 20 days.
Long-term results of treatment of patients with erosive and ulcerative lesions were monitored for 5 years. Relapses were observed after six months in 7 patients due to dietary violations and exacerbation of general somatic diseases.
Based on the above, we can conclude that the complex ointment is an effective remedy in the complex treatment of erosive forms of PL and leukoplakia of the oral mucosa and is recommended for implementation in dental practice.
- Borovsky E. V. Therapeutic dentistry / E. V. Borovsky. - M.: Medical Information Agency, 2006. - 800 p.
- Brusenina N.D. Lip diseases: Textbook / N.D. Brusenina, E.A. Rybalkina. Ed. Barera G.M. - M.: Federal State Educational Institution "VUNMC" of Roszdrav, 2005. - 184 p., ill.
- Bykova I. A. Cytological characteristics of prints of the oral mucosa using the cell differentiation index / Bykova I. A., Agadzhanyan A. A., Banchenko G. V. // Laboratory work. - 1987, No. 1. - P. 33-35.
- Vasiltsova S.V. Dental morbidity and effectiveness of therapeutic and preventive care for the population of the city of Barnaul: abstract of thesis. dis. Ph.D. honey. science / S. V. Vasiltsova. - Novosibirsk, 2005. - 24 p.
- Therapeutic dentistry: textbook: in 3 hours / Ed. G. M. Barera. - M.: GEOTAR-Media, 2005. - Part 3. - P. 195-211, 218-233.
- Therapeutic dentistry: national guide / Ed. L. A. Dmitrieva, Yu. M. Maksimovsky. - M.: GEOTAR-Media, 2009. - 912 p.
- Tokmakova S.I. Oral mucosa in elderly and senile people and its changes in visceral pathology // Dis. Dr. med. Sci. - Omsk, 2002. - 291 p.