Oral leukoplakia is a pathological condition in which changes occur in the epithelium of the oral mucosa. The main symptom of oral leukoplakia is keratinization of the epithelium (normally it is non-keratinized). The changes affect not only the epithelium of the mucous membrane, but also the red border of the lips, the mucous membrane of the nasal cavity, genitals and rectum.
Leukoplakia of the oral cavity is a precancerous condition, and compared to other pathological precancerous conditions it is more common, recorded in 18 percent of patients with diseases of the oral mucosa.
Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Electrocoagulation
Treatment using electrocoagulation is one of the cheapest. However, today few doctors recommend this traumatic procedure. The fact is that during electrosurgery the surrounding healthy tissues are also damaged, healing occurs very slowly and there remains a risk of recurrence of the disease and its further spread.
For example, leukoplakia of the oral mucosa can develop into a lesion of the larynx if the affected areas were not completely cauterized. And since leukoplakia of the throat is much more dangerous than damage to the oral mucosa, it is better to choose treatment that guarantees a 100% recovery result.
Symptoms
The first signs of the disease often go unnoticed because they do not cause any pain or discomfort in the patient. Nevertheless, a specialist will be able to determine the onset of leukoplakia by the appearance of the mucous membrane, lips and the area where the teeth meet.
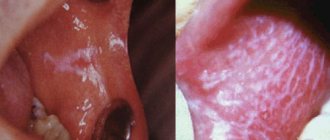
The first sign of the disease is the appearance of a keratinized gray area, which can appear on the palate (in smokers), in the corners of the mouth, on the inside of the cheek, etc. An easily removable white plaque forms in this area, but after a few days the formation makes itself felt again . The patient may feel tightness in the mouth, but, as practice shows, most people simply do not pay attention to this.
Plaques with a diameter of no more than 4 centimeters are formed. They may appear:
- on the inner surface of the cheeks;
- on the tongue (on the back or sides);
- in the sky;
- on the gums;
- in the corners of the mouth.
The process of plaque formation takes up to one month. At the first stage, the area of the future formation seems slightly swollen; when you feel it with your fingers, the compaction is not felt. However, over time, another symptom of oral leukoplakia appears - the mucous membrane at the site of the swelling loses its original shine and becomes rough, which is noticeable when touched.
There is no pain in this case: only sometimes a feeling of dryness at the site of the outbreak is possible.
Gradually, the color of the spots changes from gray to bright white. The spots in most cases have clear boundaries. Their increase is possible when the disease enters its second stage, called verrucous.
The disease often causes candidiasis and malignant cancers. In an advanced state, leukoplakia is very difficult to treat: the affected areas become even more keratinized, ulcers can form, and the infection gradually spreads to other areas of the mouth.
Nutrition
Since in most cases of disease the patient does not experience any complications or pain symptoms, there is no need to follow a diet for leukoplakia. However, most often the cause of the formation of plaques is a low level of immunity, and therefore, nutrition should be complete, healthy and rich in vitamins.
In advanced and severe forms of the disease, when it is difficult for the patient to open his mouth and chew food due to the formation of erosions and ulcers in places where the mucous membrane is damaged, it is recommended to switch to a porridge-like and puree-like consistency of food. It is also necessary to avoid eating too spicy and too hot foods.
Kinds
- The most common is simple or, as it is also called, flat leukoplakia . It is usually discovered by chance during an examination by a dentist, since the patient does not experience any subjective sensations. A burning sensation occurs extremely rarely, and the appearance of the mucous membrane may change. If the disease affects the tongue, loss of taste may occur.
- Hairy leukoplakia of the tongue resembles stomatitis. The shape of the spot that appears, as well as its size, can be different, the color - from pale gray to white. The surface of the mucous membrane at the site of the lesion becomes slightly rough, which can be felt to the touch. On the cheeks it appears as solid or broken lines. It can also be found on the lips, where it looks like thin paper pasted on.
- Verrucous leukoplakia is the second stage of the development of the disease. The keratinization thickens, the affected area seems to rise above the nearby tissues. When you touch it with your fingers, you feel a compaction.
- Erosive form . Untimely diagnosis of the two previous stages of the disease leads to a worsening of the situation - the person feels pain when exposed to any irritants, erosions or ulcers are visible in the mouth.
- Soft leukoplakia is a type of cancer. Its distinctive feature is peeling of tissue in the area of the lesion. To clarify the diagnosis, a histological method of studying cells is required.
- Tappeiner's leukoplakia . This form of the disease affects people who abuse smoking. According to studies, daily smoking 10 cigarettes a day increases the chance of developing the disease by 50 times (as the number of cigarettes increases, the risk also increases)
The disease begins with the formation of lesions on the roof of the mouth (sometimes they appear on the gums). The mucous membrane changes its color to a pronounced gray or bluish, which is noticeable to the naked eye, folds appear on it. Reddish nodules may begin to appear, which is accompanied by infectious inflammation of the oral cavity (caused by the accumulation of salivary gland secretions in the tissues).
What does leukoplakia look like?
The disease can affect not only the oral cavity, but also other organs (esophagus, bladder, genitourinary organs, etc.) that have a mucous membrane, however, it is in the mouth that the lesion can be diagnosed earlier than in other places.
Foci of damage to the mucous membrane are characterized by plaques and growths of whitish or gray color, ranging in size from a few millimeters to three to four centimeters. During a quick examination of the oral cavity, plaques located under the tongue and on the walls of the cheeks can be quite difficult to notice. At the initial stage of the disease, the plaques practically do not rise above the rest of the surface of the mucous membrane, but later they can become hard, heterogeneous, ulcerated, and acquire sharp edges that cause discomfort.
Focal leukoplakia can form over months and even years, however, most often the lesions are visually determined within a couple of weeks after the onset of the disease. In this case, in most patients there is no pain, only a slight increase in the sensitivity of the affected area to temperature effects.
Diagnosis of oral leukoplakia
Treatment of any disease begins with diagnosis: leukoplakia is no exception in this regard.
During the examination, the doctor interviews the patient to determine the factors contributing to the development of the disease. These include regular exposure to tobacco smoke, working in hazardous conditions, recent dental surgery, etc.
Next, laboratory tests are prescribed. The following procedures can be carried out:
- tissue sampling (biopsy). Accompanied by anesthesia;
- examination of the collected material under a microscope. The method allows you to determine the presence or absence of cancer cells in the formation;
- a smear of the mucous membrane is taken;
- A Schiller test is done (the mucous membrane is stained with a solution consisting of water and iodine - foci of leukoplakia are not stained);
- blood is taken for analysis (an increase in ESR may indicate the presence of malignant neoplasms).
In addition, the doctor may additionally prescribe a urine test, conduct a biochemical blood test and request the result of fluorography. You may need to consult an oncologist (if cancer is suspected), a therapist (to rule out infectious diseases) and a dermatologist (to look for other foci of disease).
Consequences
Many patients, having received a similar diagnosis from a doctor, are interested in whether leukoplakia is dangerous. Most doctors consider simple forms of this disease to be safe and do not require special treatment. Leukoplakia in the initial stage has a favorable prognosis, especially if it is caused only by external irritants, and not by a functional disorder of the internal organs.
However, there are also frequent cases of precancerous leukoplakia - the danger of this form is clear to everyone. If atypical cancer cells are detected in the histological analysis of the obtained material, this type of disease requires immediate surgery. If left untreated, the consequences of leukoplakia at the cancer stage can be disappointing. After the operation and the end of the rehabilitation period, the patient is recommended to undergo periodic examinations and take a course of medications aimed at a speedy recovery.
Leukoplakia of the oral cavity: treatment with medications
Treatment involves the complete elimination of irritating factors that led to the development of the disease:
- to give up smoking;
- grinding down sharp edges of teeth;
- sanitation of the oral cavity;
- replacement of fillings;
- use of products to protect the surface of the lips.
Additionally, a course of vitamin A is prescribed, lasting at least a month, which inhibits the process of tissue keratinization.
If the measures taken do not cause complete disappearance of the manifestations of the disease, surgical intervention is allowed: the lesion is excised, depending on the degree of development of the disease, cryodestruction or electrocoagulation is used.
Ulcers deserve special attention, as they can develop into cancerous tumors. For their treatment, drugs are prescribed that enhance the process of tissue regeneration and epithelization. If there is no positive dynamics, surgical intervention cannot be avoided.
A person with leukoplakia must constantly visit the dentist for examination to prevent malignant degeneration of the cells.
In addition to quitting smoking, the patient’s diet is adjusted: during treatment, spicy and too salty foods are excluded from the diet, and it is recommended to eat more vegetables and fruits.
Drugs prescribed:
- products that restore the epithelium (the most effective was 30 percent tocopherol acetate, which is applied to damaged areas three times a day for 15 minutes, after which it is washed off with water);
- antiseptics (after each meal it is recommended to rinse your mouth with a solution of chlorhexidine at a concentration of 0.05%);
- analgesics (their use is justified in the presence of pain. Lidocaine, applied to the mucous membrane before meals, has worked well).
Under no circumstances should you use drugs that have an irritating effect, as otherwise this can lead to the formation of cancer cells.
If there is no improvement within a couple of weeks, surgery is prescribed: this can be either excision with a scalpel or the application of cold in the form of a liquid stream of nitrogen.
Treatment methods
Treatment of leukoplakia may require a collegial approach: the participation of the oncologist in developing an action plan. The basis of therapy is the elimination of provoking factors: quitting smoking, changing jobs due to occupational hazards, following a soft diet with no spices, etc. According to indications, correction of dentures, replacement of fillings, treatment of caries, removal of teeth that cannot be restored and other measures are carried out .
As part of complex treatment, the doctor may prescribe the following medications:
- Preparations for restoring the normal structure of the oral epithelium. It is usually used in the form of applications to the affected areas.
- Antiseptics. Used for the prevention and treatment of inflammatory complications of the disease.
- Painkillers and symptomatic therapy. Systemic medications or applications of local anesthetics used in dentistry may be used.
Self-medication for leukoplakia in the mouth is strictly not recommended. Many drugs, including some anti-inflammatory drugs, are irritating and increase the risk of developing malignant tumors.
If the disease is severe, hospitalization may be required. The presence of ulcers and erosions is an indication for the use of hormonal anti-inflammatory drugs, proteolytic enzymes, etc. Surgery is indicated when conservative treatment is ineffective. Cryodestruction and excision with a scalpel are usually used.
Oral leukoplakia: how to treat it at home
In addition to drug treatment, oral leukoplakia can be treated with traditional medicine.
There are many recipes, here are just the main ones:
- rinsing with herbs (infusions of oregano, chamomile, ginseng and other adaptogens that reduce the inflammatory process and increase the body’s resistance to harmful factors are suitable);
- regular consumption of nuts and tinctures based on them;
- rinsing with decoctions of calendula, St. John's wort, eucalyptus. Alternation works well - once the oral cavity is rinsed with a soda solution, after a couple of hours - with an infusion of herbs. This procedure should be repeated at least 5 times a day;
- lubricating the lesions with sea buckthorn and olives (the fruits must first be mashed in your hands so that the juice appears).
Timely detection of the disease and compliance with all doctor’s recommendations is the key to recovery in the shortest possible time and reducing the risk of complications. If you start treatment at the initial stage, you can reduce the likelihood of complications to almost zero.
Diagnosis of the disease
The diagnosis is made based on examination and questioning of the patient. Mandatory diagnostic studies confirming the diagnosis include:
- Cytology is the collection of epithelial cells to identify cancerous lesions.
- Histology is taken to perform a biopsy, which allows examination of the affected epithelial tissue to detect cancer cells.
- Blood from a vein.
Additional clarifying studies make it possible to distinguish leukoplakia from other pathologies.
Treatment and prevention of the disease
If you find any manifestations that resemble leukoplakia, you should immediately consult a doctor! Since this disease is a type of precancerous condition, it is critically important to identify it in time and carry out a set of treatment measures. One of the important reasons for timely treatment of leukoplakia is the fact that more than thirty percent of cancer patients diagnosed with squamous cell carcinoma of the tongue and oral mucosa were previously diagnosed with oral leukoplakia. Often, as a result of histological analysis of leukoplakic plaques, it turns out that the patient has cancer.
Treatment of leukoplakia must be comprehensive. The dentist must clean the oral cavity (sanitation), as well as identify and eliminate traumatic factors - fragments of teeth, uneven edges of fillings and crowns. The patient, in turn, must be aware of the importance of giving up alcohol and smoking in the early stages of treatment. Most likely, incorrectly installed dentures and fillings will be removed. It is also necessary to avoid spicy and solid foods.
The patient will have to undergo studies to identify possible somatic diseases that accompany leukoplakia in most cases. Thus, you should prepare for an appointment not only with a dentist, but also with an endocrinologist, therapist and, first of all, with an oncologist.
Causes
Different localizations of leukoplakia are caused by different reasons and require an individual approach in developing a treatment strategy.
Hairy leukoplakia develops against a background of reduced and weakened immunity, so most often this type of disease is diagnosed in patients with HIV, various immunodeficiencies and during rehabilitation after organ transplantation, when a course of immunosuppressants is prescribed.
- Leukoplakia of the external genitalia in women develops most often during menopause, when reverse development processes occur in tissues and cells. Mucous tissues and skin become drier, hair loss is observed, which is a normal physiological process.
- Leukoplakia of the esophagus develops after heartburn or burns of the mucous membrane of this organ; more than half of the cases of this disease cause the appearance of a cancerous tumor.
- Leukoplakia in the oral cavity is most often localized on the mucous membranes of the inner side of the cheek, the hard and soft palate, as well as in the angular folds of the mouth. Leukoplakia of the tongue is extremely rare in medicine.
To this day, official medicine does not know the exact reasons for the development of this disease in the mouth. However, a number of factors have been identified that increase the chances of developing leukoplakia:
- metabolic disorders;
- genetic predisposition;
- lack of vitamin A;
- smoking;
- chronic injuries to the mucous membranes (for example, due to improperly manufactured dentures);
- activities associated with direct contact with coal and coal tar, as well as their processing processes;
- HIV and AIDS;
- chronic inflammatory processes in the mouth associated with neurological disorders.
Leukoplakia of the bladder is a protracted chronic disease that is characterized by the degeneration of transitional epithelial cells into squamous epithelial cells. The keratinized epithelium is unstable to urine components, which causes inflammation in the bladder cavity. The main cause of the development of the disease is ascending infection with sexually transmitted pathogens. Therefore, leukoplakia in the bladder develops more often in women - their urinary canal is much shorter than the male one, so it is easier for infections to penetrate through it.
In some cases, the cause of leukoplakia can be a downward infection, when a pathogen penetrates through the bloodstream from nearby organs: staphylococci, Proteus, streptococci, E. coli and others. The development of the disease is favored by:
- chronic diseases of the abdominal organs located next to the bladder;
- all factors that reduce immunity: hypothermia, stress, bad habits, chaotic lifestyle;
- foci of chronic inflammation located at a distance from the bladder: tonsillitis, caries, sinusitis, etc.;
- disturbances in the functioning of the endocrine system;
- the IUD was not removed in time in the uterine cavity;
- promiscuous sex life without the use of barrier contraception.
Leukoplakia of the cervix is called whitish formations (spots or plaques) that appear on the mucous membrane. To diagnose the disease, a preventive examination using a gynecological speculum is sufficient.
Like dysplasia, cervical leukoplakia requires mandatory treatment, since it is a precancerous disease. There are many reasons for the appearance of such tissue changes:
- decreased immunity for various reasons;
- injuries due to careless examination, termination of pregnancy, childbirth;
- interruptions in the functioning of the endocrine system;
- ovarian dysfunction;
- current or previous infectious diseases of the genital organs.