Oral mucosa: what to pay attention to
Regular dental examinations are an important part of the prevention of not only dental and periodontal diseases, but also pathologies of the oral mucosa. They make it possible to detect cancer, leukoplakia, stomatitis and other dangerous diseases in the early stages.
Inspection algorithm
The American Dental Association recommends that your oral examination include the following steps:
- a thorough visual examination of the lips, buccal mucosa, gums, anterior part of the tongue, floor of the mouth and palate;
- examination of the throat (pharynx), including tonsils, root of the tongue;
- palpation of the jaw and neck to detect nodes, tumors, any abnormalities or abnormalities.
This procedure allows you to timely identify foci of pathological processes in the oral mucosa (OM), including erosion, ulcers, compactions, and also assess the condition of the lymph nodes.
Russian specialists adhere to a similar inspection algorithm. He suggests that the dentist should pay attention to any visible abnormalities in the structure of the face, nose, cheeks or chin. Pathological changes, taking into account their localization, are recorded using special codes. Thus, ulcerations of the mucous membranes, wounds, tissue erosions, cracks, enlarged lymph nodes and any other lesions are necessarily noted.
Oral diseases
The most common symptoms of stomatitis encountered in dental practice. Acute herpetic stomatitis accounts for 85% of all diseases of the oral mucosa; chronic recurrent aphthous stomatitis is also common [1].
Aphthous stomatitis is considered a diagnostic feature of aphthous stomatitis - oval ulcerations on the oral mucosa with clear edges, with a diameter of 3-12 mm or more, surrounded by a halo of hyperemia. Herpetic stomatitis is characterized by blistering rashes not only on the surface of the mucous membrane, but also on the lips and skin around the mouth.
Data from multicenter studies in different countries of the world also indicate a high level of prevalence of other oral diseases: leukoplakia, candidiasis, lichen planus.
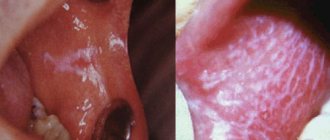
Leukoplakia is characterized by the presence of foci of keratosis in the form of whitish thickenings on the oral mucosa and the red border of the lips. With candidiasis, spots of white plaque with a cheesy consistency form on the mucous membrane, which are easily scraped off with a spatula. With secondary bacterial infection and erosion, the plaque may acquire a brownish tint.
The most common sign of oral lichen planus is also gray-white spots. They appear on the inner surfaces of the cheeks, tongue and gums. Due to the similarity of these manifestations with the symptoms of other diseases, in particular leukoplakia, visual diagnosis can be difficult.
Unfortunately, in recent years the number of cases of oral cancer has been increasing. The World Dental Federation attributes this to widespread smoking and alcohol consumption. Therefore, early diagnosis of cancer of the oral mucosa is becoming increasingly important. It is precisely this that makes it possible to identify precancerous and cancerous states of cells at stages when treatment can be anatomically gentle.
Experts advise paying attention to the following signs, which may be symptoms of oral cancer:
- long-term non-healing wound or irritation;
- red or white spots;
- sensation of pain, numbness, sensitive areas in the mouth or on the surface of the lips;
- tumors, thickening, roughness, erosion and other changes;
- difficulty chewing, swallowing, speaking, or moving the tongue or jaw.
The number of visits to dentists by Russians is approximately 15 million per year [2]. This figure is higher than any other medical specialty. Therefore, the doctor’s compliance with the external examination algorithm, thoroughness and accuracy during its implementation are the key to the success of early detection of many dangerous diseases of the oral cavity.
List of sources
[1] Zarkumova A.E. Structure of morbidity of the oral mucosa // Bulletin of KazNMU. 2022. No. 3. URL: https://cyberleninka.ru/article/n/struktura-zabolevaemosti-slizistoy-obolochki-polosti-rta (date of access: 05/22/2020).
[2] Astakhov P. Chief dentist of the Ministry of Health: mortality in the dentist’s chair is below 0.001% // RT, June 7, 2022. URL: https://russian.rt.com/russia/news/397438-glavnyi-stomatolog-minzdrav-smertnost (access date: 05/22/2020).
Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Leukoplakia of the oral cavity: treatment with medications
Treatment involves the complete elimination of irritating factors that led to the development of the disease:
- to give up smoking;
- grinding down sharp edges of teeth;
- sanitation of the oral cavity;
- replacement of fillings;
- use of products to protect the surface of the lips.
Additionally, a course of vitamin A is prescribed, lasting at least a month, which inhibits the process of tissue keratinization.
If the measures taken do not cause complete disappearance of the manifestations of the disease, surgical intervention is allowed: the lesion is excised, depending on the degree of development of the disease, cryodestruction or electrocoagulation is used.
Ulcers deserve special attention, as they can develop into cancerous tumors. For their treatment, drugs are prescribed that enhance the process of tissue regeneration and epithelization. If there is no positive dynamics, surgical intervention cannot be avoided.
A person with leukoplakia must constantly visit the dentist for examination to prevent malignant degeneration of the cells.
In addition to quitting smoking, the patient’s diet is adjusted: during treatment, spicy and too salty foods are excluded from the diet, and it is recommended to eat more vegetables and fruits.
Drugs prescribed:
- products that restore the epithelium (the most effective was 30 percent tocopherol acetate, which is applied to damaged areas three times a day for 15 minutes, after which it is washed off with water);
- antiseptics (after each meal it is recommended to rinse your mouth with a solution of chlorhexidine at a concentration of 0.05%);
- analgesics (their use is justified in the presence of pain. Lidocaine, applied to the mucous membrane before meals, has worked well).
Under no circumstances should you use drugs that have an irritating effect, as otherwise this can lead to the formation of cancer cells.
If there is no improvement within a couple of weeks, surgery is prescribed: this can be either excision with a scalpel or the application of cold in the form of a liquid stream of nitrogen.
Symptoms
The first signs of the disease often go unnoticed because they do not cause any pain or discomfort in the patient. Nevertheless, a specialist will be able to determine the onset of leukoplakia by the appearance of the mucous membrane, lips and the area where the teeth meet.
The first sign of the disease is the appearance of a keratinized gray area, which can appear on the palate (in smokers), in the corners of the mouth, on the inside of the cheek, etc. An easily removable white plaque forms in this area, but after a few days the formation makes itself felt again . The patient may feel tightness in the mouth, but, as practice shows, most people simply do not pay attention to this.
Plaques with a diameter of no more than 4 centimeters are formed. They may appear:
- on the inner surface of the cheeks;
- on the tongue (on the back or sides);
- in the sky;
- on the gums;
- in the corners of the mouth.
The process of plaque formation takes up to one month. At the first stage, the area of the future formation seems slightly swollen; when you feel it with your fingers, the compaction is not felt. However, over time, another symptom of oral leukoplakia appears - the mucous membrane at the site of the swelling loses its original shine and becomes rough, which is noticeable when touched.
There is no pain in this case: only sometimes a feeling of dryness at the site of the outbreak is possible.
Gradually, the color of the spots changes from gray to bright white. The spots in most cases have clear boundaries. Their increase is possible when the disease enters its second stage, called verrucous.
The disease often causes candidiasis and malignant cancers. In an advanced state, leukoplakia is very difficult to treat: the affected areas become even more keratinized, ulcers can form, and the infection gradually spreads to other areas of the mouth.
Diagnosis of oral leukoplakia
Treatment of any disease begins with diagnosis: leukoplakia is no exception in this regard.
During the examination, the doctor interviews the patient to determine the factors contributing to the development of the disease. These include regular exposure to tobacco smoke, working in hazardous conditions, recent dental surgery, etc.
Next, laboratory tests are prescribed. The following procedures can be carried out:
- tissue sampling (biopsy). Accompanied by anesthesia;
- examination of the collected material under a microscope. The method allows you to determine the presence or absence of cancer cells in the formation;
- a smear of the mucous membrane is taken;
- A Schiller test is done (the mucous membrane is stained with a solution consisting of water and iodine - foci of leukoplakia are not stained);
- blood is taken for analysis (an increase in ESR may indicate the presence of malignant neoplasms).
In addition, the doctor may additionally prescribe a urine test, conduct a biochemical blood test and request the result of fluorography. You may need to consult an oncologist (if cancer is suspected), a therapist (to rule out infectious diseases) and a dermatologist (to look for other foci of disease).
Oral leukoplakia: how to treat it at home
In addition to drug treatment, oral leukoplakia can be treated with traditional medicine.
There are many recipes, here are just the main ones:
- rinsing with herbs (infusions of oregano, chamomile, ginseng and other adaptogens that reduce the inflammatory process and increase the body’s resistance to harmful factors are suitable);
- regular consumption of nuts and tinctures based on them;
- rinsing with decoctions of calendula, St. John's wort, eucalyptus. Alternation works well - once the oral cavity is rinsed with a soda solution, after a couple of hours - with an infusion of herbs. This procedure should be repeated at least 5 times a day;
- lubricating the lesions with sea buckthorn and olives (the fruits must first be mashed in your hands so that the juice appears).
Timely detection of the disease and compliance with all doctor’s recommendations is the key to recovery in the shortest possible time and reducing the risk of complications. If you start treatment at the initial stage, you can reduce the likelihood of complications to almost zero.