It's all the virus's fault!
The term "stomatitis" is derived from the merger of two Greek words: stoma (mouth) and itis (inflammation). There are a great variety of different types of disease - serous, aphthous, allergic, etc. The most dangerous is herpetic, or cold sore, stomatitis caused by a virus. Its main manifestations are painful ulcers covering the oral mucosa. The trigger mechanism of the disease is the activation of herpes simplex virus types 1 and 2. First of all, the disease threatens those who have a weakened immune system and, as a result, the body simply does not have the strength to give a worthy rebuff to viruses.
Forms of the disease
Lightweight
It is considered the most beneficial for the body. In this form, people with high immunity suffer from herpes stomatitis. It flows without temperature. It is distinguished by single rashes that do not cause discomfort and disappear on their own without consequences.
Average
General disorders are added: weakness, drowsiness, fatigue, loss of appetite. Rashes appear in several places at the same time. The temperature rises to 37-37.6°C.
Heavy
This form of stomatitis indicates extremely low immunity. The rashes are multiple and painful. Severe headache, chills, and vomiting appear. The temperature exceeds 38oC.
If the disease is mild, the patient may not notice any external signs!
How to distinguish herpes from stomatitis?
Many patients try to find an answer on the Internet to the question: “Do I have stomatitis or herpes? How to recognize? Herpes stomatitis can be easily distinguished from ordinary stomatitis by 3 key signs.
- With herpes infection, the rash is localized in the gum area. Whereas with stomatitis - on the soft tissues of the oral cavity (tongue, cheeks).
- A herpes rash first appears as blisters, which then ulcerate, while stomatitis begins with the appearance of ulcers.
- Herpetic stomatitis is characterized by a stable appearance of the rash in the same places, and with ordinary stomatitis its location often changes.
Kinds
- The most common is simple or, as it is also called, flat leukoplakia . It is usually discovered by chance during an examination by a dentist, since the patient does not experience any subjective sensations. A burning sensation occurs extremely rarely, and the appearance of the mucous membrane may change. If the disease affects the tongue, loss of taste may occur.
- Hairy leukoplakia of the tongue resembles stomatitis. The shape of the spot that appears, as well as its size, can be different, the color - from pale gray to white. The surface of the mucous membrane at the site of the lesion becomes slightly rough, which can be felt to the touch. On the cheeks it appears as solid or broken lines. It can also be found on the lips, where it looks like thin paper pasted on.
- Verrucous leukoplakia is the second stage of the development of the disease. The keratinization thickens, the affected area seems to rise above the nearby tissues. When you touch it with your fingers, you feel a compaction.
- Erosive form . Untimely diagnosis of the two previous stages of the disease leads to a worsening of the situation - the person feels pain when exposed to any irritants, erosions or ulcers are visible in the mouth.
- Soft leukoplakia is a type of cancer. Its distinctive feature is peeling of tissue in the area of the lesion. To clarify the diagnosis, a histological method of studying cells is required.
- Tappeiner's leukoplakia . This form of the disease affects people who abuse smoking. According to studies, daily smoking 10 cigarettes a day increases the chance of developing the disease by 50 times (as the number of cigarettes increases, the risk also increases)
The disease begins with the formation of lesions on the roof of the mouth (sometimes they appear on the gums). The mucous membrane changes its color to a pronounced gray or bluish, which is noticeable to the naked eye, folds appear on it. Reddish nodules may begin to appear, which is accompanied by infectious inflammation of the oral cavity (caused by the accumulation of salivary gland secretions in the tissues).
Herpetic or aphthous?
It will be somewhat more difficult to distinguish between herpetic and aphthous stomatitis. The latter got its name from the Greek term “aftha”, which means “ulcer”.
If with herpetic stomatitis there are many ulcers, but they are small, then with aphthous stomatitis there are few of them, and the size can reach 7–8 mm.
The second important distinguishing feature is the absence of swelling of the gums with aphthous stomatitis.
If you are looking for differences between herpetic and aphthous stomatitis, then the third thing you should pay attention to is the localization of the rash. Aphthous is characterized by the appearance of ulcers in the oral cavity, while herpes infection can spread to the border of the lips.
Symptoms of inflammatory diseases
Inflammation in the oral cavity is manifested by both general and local symptoms [1]. Even before the onset of local manifestations, general malaise, pain, irritation, rashes in the mouth, increased body temperature, and decreased appetite are noted [1]. In addition, inflammation in the mouth itself can act as a symptom of another disease or general pathology [1].
Symptoms of certain inflammatory diseases
Stomatitis is a wide group of diseases that can be caused by individual pathogens, for example, fungi (candidal stomatitis) or the herpes simplex virus (herpes stomatitis), and systemic diseases, for example, chronic diseases of the gastrointestinal tract (aphthous stomatitis) [2] .
Most often, stomatitis appears as rashes (ulcers, blisters or other forms) on the oral mucosa. The nature of the rash is a striking distinctive feature that plays an important role in diagnosis. For example, with aphthous stomatitis, the ulcers never appear on the outer surface of the lips, as is the case with lesions caused by the herpes simplex virus [2].
Herpetic stomatitis, as a rule, accompanies a general infection of the body and is characterized by rashes on the inner surface of the cheeks, tongue, palate, and lips [2].
With insufficient oral care, bacterial microflora may develop and cause deeper lesions of the mucous membrane.
If the necessary treatment of acute herpetic stomatitis is not carried out, a recurrent form occurs, which is accompanied by regular rashes on the oral mucosa of vesicles and aphthae "Microbiology, virology and immunology of the oral cavity", ed. Doctor of Medicine V. N. Tsareva.
Catarrhal stomatitis occurs quite often and develops due to the lack or poor hygiene and the presence of chronic foci of infection in the oral cavity. Symptoms of this type of stomatitis are swelling of the mucous membrane, the appearance of plaque on it, first white, then brown, and bad breath [1].
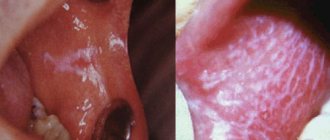
Candidiasis (candidal stomatitis, thrush) is caused by fungi of the genus Candida, which are normally always present in the mouth in small quantities [2]. Factors contributing to the sharp growth of fungi are long-term use of antibiotics and some other drugs, hypovitaminosis, endocrine and other disorders.
A striking symptom of candidiasis is the appearance of a white or yellowish-white coating on the tongue and the mucous membrane of the cheeks due to the development of inflammation in the mouth. The plaque is easily removed, revealing reddened, inflamed and eroded areas of the oral mucosa underneath.
Leukoplakia refers to chronic inflammatory diseases. It develops in response to constant irritation of the oral mucosa, for example, from a part of a denture, a sharp edge or chipped tooth, hot drinks or food, alcoholic beverages, or smoking [1]. Leukoplakia manifests itself in the form of whitish thickenings, usually in the cheek area along the line of closure of the teeth, in the corners of the mouth, on the back and on the lateral surfaces of the tongue.
How to distinguish herpes sore throat from stomatitis?
Despite the fact that these medical terms have the same grammatical root, herpetic sore throat and herpetic stomatitis are two different diseases. Unlike stomatitis, herpes sore throat occurs not due to the penetration of the herpes virus, but as a result of an adenovirus infection (in particular, the Coxsackie A virus). Children are more likely to suffer from this disease than adults. The rashes are localized, for the most part, on the soft palate and tonsils. Typical symptoms of stomatitis include pain in the abdomen and abnormal bowel movements.
Attention!
The disease begins acutely, with a jump in temperature to 40 degrees, and is severe, so differential diagnosis should only be carried out by a doctor.
Syphilis of the oral mucosa
Syphilis of the oral mucosa is a manifestation of a general chronic disease that affects the entire body. In principle, all doctors, both general practitioners and dentists, know: the idea that syphilis can only manifest itself on the genitals is a misconception.
Etiology of syphilis
The etiology of syphilis is associated with a bacteria called Treponema pallidum. The route of infection is sexual, but it can also occur oral. In general, in order for the disease to develop, it is only necessary for Treponema pallidum to penetrate through the damaged mucous membrane or skin. Cases of penetration through intact skin and mucous membranes have been recorded. Syphilis is quite common; about 40% of children have manifestations of primary syphilis in the oral cavity. Secondary recurrent syphilis is less common, occurring in about 10% of cases in adolescents.
Syphilis in the 21st century is a medical and social problem.
Clinical picture of syphilis
The clinical picture of syphilis primarily depends and differs, of course, from the period of syphilis. There are 3 periods in the development of syphilis. Each period has its own characteristics in the manifestation and treatment of the disease. It must be remembered that congenital syphilis is also included in a separate group of syphilitic diseases.
For the clinical picture of syphilis to develop, it is necessary for about 3 to 4 weeks to pass, which is the incubation period of syphilis. But it is possible to shorten it to 1 - 1.5 weeks, or lengthen it to six months.
So.
Clinical picture of syphilis - First period of syphilis
The clinical picture of the primary period of syphilis is associated with the appearance at the site where treponema has invaded, the appearance of hard chancre - primary syphiloma.
Primary syphiloma will be clinically noticeable within 1.5 - 2 months, that is, about 6 - 8 weeks. What does chancre look like? In principle, a hard chakra can be either in the form of an ulcer or in the form of erosion. Often oval or round in shape, may be saucer-shaped. The edges are always smooth and crisp. Syphilitic chancre is always at the same level with the mucous membrane of the oral cavity.
In rare cases, the edges of the ulcer may be raised. The bottom of the chancre is smooth, shiny, bright red. The literature specifies that the bottom may be “greasy”, that is, slightly colored with a dull white coating. The main sign by which a tuberculous ulcer can be distinguished from a chancre is complete painlessness on palpation of a chancre. There have been cases when the size of the chancre was almost equal to the area of the entire mucous membrane of the hard and soft palate, but it did not cause any subjective sensations in the patient. Also, in the presence of hard chancre, there are no acute inflammatory processes in the surrounding mucous membrane.
Chancre is painless upon palpation, we have sorted this out, but in its consistency it is dense and “cartilage-like”.
This means the patient walks like this for 3 or 4 days. Then a week passes. And nothing seems to bother him: “Well, there’s something red in the mouth, but it doesn’t hurt.” So after a week, maximum 10 days, the lymph nodes are involved in the process. Lymph nodes in the primary period of syphilis increase in size, are dense, elastic, and painless on palpation. The lymph nodes do not merge with the skin, and the color of the skin does not change.
In addition, primary syphilis can manifest itself not only in the form of erosion or ulcers, but can also be a regular abrasion. The favorite places when primary syphilis appears in the form of an abrasion are the corners of the mouth - identical to jams, only unlike them, the abrasion will be dense at the base. On the transitional fold - elongated, on the tongue - this is the middle third, one abrasion, maximum two. If primary syphilis appears on the gums, then it will be an ulcer, bright red in color, its length corresponding to the width of 1 - 2 teeth.
Very rare cases of manifestation of primary syphilis on the tonsil. However! Primary syphilis on the tonsil is characterized by its unilateral enlargement, painlessness, with the presence of purulent plugs.
With primary syphiloma, hard chancres can be located close to each other and merge, forming a herpetiform chancre. This manifestation of primary syphilis is the most rare of all the manifestations in the oral cavity that have previously occurred.
To summarize, this is what you should remember: primary syphilis occurs 6-8 weeks after infection. Its first manifestation is chancre (here you need to read the description of chancre again), which can be located on the mucous membrane of the cheeks, palate, lips, transitional fold, tongue, and in rare cases on the tonsil. Lymph nodes enlarge a week after the onset of chancroid. The diagnosis will be established only after identifying chancre in the punctate and lymph nodes - treponema pallidum. Serological reactions are positive 4-5 weeks after infection.
Clinical picture of syphilis - Secondary period of syphilis
The secondary period of syphilis is characterized by a long course, namely from 3 to 5 years. The secondary period of syphilis will begin 1.5 - 2 months after the appearance of chancre. An important difference between the secondary period of syphilis and the primary period is not only the elements of the lesion, but also the peculiarity of the course. Since the secondary period of syphilis occurs in waves. What this means is that in the second period of syphilis there is both an active period, when there are elements of the lesion, and a latent period, when there are no elements visible to the eye.
During the active secondary period of syphilis, the clinical picture will be characterized by the presence of elements such as roseola, papules, pustules - secondary syphilides. These are elements that occur both on the skin and on the mucous membrane. The outlines of the elements in the secondary period of syphilis are rounded, smooth, the boundaries are clear and sharp. The color ranges from bright pink to scarlet and red. These elements do not have the ability to merge with each other. Secondary syphilides pass quickly, do not cause itching, and do not leave scars.
Secondary syphilides can occur in addition to the skin and mucous membranes of the lips and cheeks on the tongue, soft palate and tonsils. The main feature of the occurrence of secondary syphilides in these places is their constant tendency to merge, forming large lesions. The mucous membrane in these places is hyperemic, swollen, and pain may occur when swallowing.
However, the most common lesions on the mucous membrane are papules. Papules in secondary syphilis are round, dense, painless on palpation, surrounded by a halo of hyperemia. The size of papules can vary from 3 – 10 mm. Localization varies.
Papules can appear on the tongue; there are some peculiarities here:
- With atrophy of the filiform papillae, smooth, shiny, oval-shaped surfaces may form just below the level of the mucosa. This clinical picture is called “Mowed meadow”
- Papules on the tongue can increase in size, that is, hypertrophy, change in color, and become pale red. This type of secondary syphilis on the tongue is called hypertrophied papules;
- “Opal papules on the tongue” - trauma to the papules occurs, the surface becomes wrinkled, the papules will be loose, pale with a whitish tint.
Clinical picture of syphilis - Tertiary period of syphilis
The clinical picture of the tertiary period of syphilis is the most complex, characterized by the appearance of syphilitic gummas or tubercles, sclerosing glossitis. At the same time, syphilitic gummas differ from secondary syphilides by deeper penetration into the skin and mucous membranes and involvement in the pathological process of the central nervous system and other body systems. Tertiary syphilis can cause paralysis due to irreversible destructive processes.
The tertiary period of syphilis, fortunately, is rare, since patients seek help at the first stage of the disease. The tertiary period of syphilis is observed in patients who have undergone either poor quality treatment for syphilis or incomplete treatment. The literature identifies some predisposing factors for the occurrence of the tertiary period of syphilis:
- Childhood or old age;
- Alcoholzym;
- Presence of concomitant difficult-to-treat pathology
The tertiary period of syphilis lasts 8–10 years. For syphilitic gummas to appear, not 1, but at least 3 months must pass. An important feature of the course of the tertiary period is that after the disappearance of the gumma, scars remain.
If a bump appears, it is most often on the lips. The clinical picture of tubercular syphilis: the tubercles are red-blue in color, initially located singly, merge over time, after the collapse of which ulcers appear: painful, deep, small, with undermined edges. The ulcer heals - a scar for life.
Syphilitic gummas will be located in the oral cavity. There are always few of them. Either in a group or alone. The size of syphilistic lips is small, often compared to a nut. After the gumma disintegrates, an ulcer appears, which has undermined, uneven edges, often covered with granulations, and a dense bluish-red ridge at the bottom. Gummas can perforate the hard/soft palate if left untreated.
Most often, syphilitic gummas occur on the tongue, which leads to the development of syphilitic sclerous glossitis. The tongue thickens, becomes dense and less mobile. Permanent deformation of the tongue occurs.
When the syphilitic gum disintegrates on the alveolar process, pathological mobility of the teeth occurs; percussion will be positive.
Congenital syphilis
Congenital syphilis occurs in children when Treponema pallidum penetrates the placenta from a mother who has syphilis. Intrauterine infection occurs at the border between 3 and 4 months of pregnancy.
Congenital syphilis can be early, that is, it appears immediately after birth, within 1 - 2 months; may be late - manifests itself between 5 and 14 years.
Early congenital syphilis - Clinical picture
The clinical picture of early congenital syphilis is entirely variable. The pathological process involves not only the skin and mucous membranes, but also bones, organs, and the central nervous system.
If the manifestation is on the skin, it is syphilitic pemphigus. The bubbles are dense, with a purple rim around them.
The manifestation of early congenital syphilis on the skin of the chin or lips is characterized by Hochsinger infiltration. That is, erythema occurs either in the form of a focus or in the form of diffusion. After which infiltration develops. The skin becomes dense and loses elasticity. Lips swell and increase in size. The lips also change in color, a yellowish tint appears. If a child screams, this leads to injury, as cracks appear. The cracks often bleed and subsequently become covered with crusts. If treatment aimed at epithelization is not effective or is not carried out, then Robinson-Fournier scars appear - radial scars in the area of the corners of the mouth.
Late congenital syphilis - Clinical picture
The clinical picture of late congenital syphilis manifests itself in the period from 5 to 14 years and is characterized by the most severe changes that cause deep damage to tissues and organs.
There are two groups of symptoms by which late congenital syphilis can be diagnosed:
- Reliable signs: Hutchinson's triad: keratitis, Hutchinson's teeth, deafness;
- Probable signs: perioral scars, buttock-shaped skull, saddle nose, saber-shaped shins, purse-shaped first molars and canines.
Treatment of syphilis
Treatment of syphilis should be carried out by a dermatologist in specialized medical institutions. The dentist can only carry out local treatment: oral hygiene, antiseptic rinses, elimination of irritants.
The article was written by N. Shidlovskaya specifically for the OHI-S.COM website. Please, when copying material, do not forget to provide a link to the current page.
Bacterial or viral?
In addition to viral origin, the disease can be caused by bacteria: streptococci and staphylococci are normally present in the microflora of the oral cavity and begin to multiply uncontrollably during the inflammatory process. The latter may be caused by caries or periodontitis (read more about the disease in the article).
How to distinguish viral stomatitis from bacterial one? It is extremely difficult to do this at home, so it is better to consult a doctor. The main differential feature is the localization of the rash. With viral herpetic stomatitis, vesicles with transparent contents first appear on the tongue (its tip, along the side surfaces and under it), and then can even spread to the pharynx and tonsils.
For bacterial stomatitis, the location of the rash on the gums and those areas where the skin borders the mucous membrane (for example, on the red border of the lips) is more common. Also, with a disease caused by streptococci, “jams” are often observed - pustules on the corners of the mouth, which quickly begin to bleed, become covered with a crust, crack and cause constant discomfort while eating and talking.
Types of diagnostics
An experienced doctor can identify herpetic stomatitis in adults during an initial examination, relying on only two methods.
- Clinical picture.
Based on the totality of the patient’s specific complaints and distinctive external signs, the dentist will not only assess the severity of the disease, but also differentiate it from ordinary stomatitis, candidiasis, etc. - Immunofluorescence.
Express microscopy method, the most accurate for diagnosing acute herpetic stomatitis.
How to get rid of stomatitis and other inflammatory diseases of the oral cavity
Treatment of stomatitis and other inflammatory diseases is usually comprehensive, aimed at alleviating the patient’s condition, eliminating the root cause and risk factors.
Often, inflammation of the oral cavity is painful, accompanied by itching, irritation, and swelling of the mucous membrane. Because of this, patients have difficulty eating. To alleviate the condition, the affected areas are treated with various anesthetic and antiseptic rinses, powders, and solutions. This also prevents possible complications of diseases, for example, the transition of aphthae or foci of inflammation into ulcers, which require more time to heal.
Another important area of treatment is the elimination of local causes of inflammation of the oral mucosa. These include local foci of infection, for example, caries , dental plaque (tartar), traumatic chipped teeth, protruding parts of fillings or dentures [1]. For this purpose, appropriate treatment and professional hygiene are carried out.
And finally, a significant part of therapy is devoted to the diagnosis and elimination of a general disease that can provoke inflammation of the oral cavity (for example, endocrine disorders or chronic diseases of the gastrointestinal tract) [1]. In special cases, antiviral drugs [5], antimycotics [6] and antibiotics [1] are used.
Prevention of stomatitis and other inflammatory diseases includes [7]:
- treatment of major systemic diseases;
- strengthening general immunity: adherence to the principles of a healthy lifestyle, nutrition, giving up bad habits, eliminating hypo- and avitaminosis;
- strengthening local immunity: regular careful hygiene, avoiding injury and irritation of the mucous membrane in the mouth.
Regular individual and professional oral hygiene is a key way to prevent intraoral inflammation. It must include:
- brushing your teeth twice a day, after breakfast and before bed, with a soft-bristled brush and toothpaste;
- the right choice of toothpaste: if you are prone to inflammation of the mouth and gums, as prescribed by a specialist, you should give preference to pastes with anti-inflammatory and antiseptic properties;
- use of antibacterial rinses with anti-inflammatory effects;
- cleaning interdental spaces with dental floss or tape;
- regular visits to the dentist (once every 6 months) for a preventive examination and professional removal of dental plaque.
Causes of herpes stomatitis
There are two types of herpetic stomatitis: acute and chronic. Acute herpetic stomatitis, according to Dr. Komarovsky, occurs only in children under 3 years of age, when for the first time the child’s body, already deprived of antibodies to the herpes virus received from the mother, is first exposed to a viral attack from the outside. Moreover, the source of infection, as a rule, is the parents themselves - carriers of the virus, who kiss the baby or lick his pacifier or feeding spoon.
Recurrent or chronic stomatitis is already the lot of adults. The disease is recurrent in nature as soon as the body’s immune forces are weakened. In this case, primary infection can occur either through airborne droplets (sneezing), or through household contact (for example, through the use of the same dishes with a virus carrier) or hematogenous (through blood during injections, etc.). The incubation period of the disease can last up to two weeks depending on the state of the immune system.
Attention!
The pathogenesis of the disease in dentistry is still unknown. But if the body is weakened, any injury to the palate or gums can provoke activation of the herpes virus types 1 and 2!
Types of inflammatory diseases of the oral cavity
These diseases are classified depending on what causes the inflammation, as well as on the location of its source in the mouth.
Thus, general lesions of the mucous membrane are called stomatitis [1]. If the mucous membrane of only the tongue, lip, palate, gums or alveolar process becomes inflamed, they speak of glossitis , cheilitis, palatinitis, gingivitis or periostitis, respectively.
Depending on the reasons that caused the inflammatory process, these diseases are divided into:
- infectious;
- traumatic;
- symptomatic;
- specific.
If left untreated, inflammation can occur with complications and have negative consequences both for the teeth, gums, mouth and pharynx, and for the general health of a person.
Treatment of herpetic stomatitis
How to treat herpes stomatitis? Unfortunately, the herpes virus, once entered into a person’s blood, remains in a “dormant” state for the rest of his life. But treatment of viral stomatitis is possible provided that you do not delay visiting the dentist when the first signs of the disease are detected. During the period of therapy, in order to avoid infecting loved ones, you should eat and drink from separate containers and avoid kissing. The patient is recommended a diet that excludes spicy, smoked, sour and salty foods, which can irritate the damaged oral mucosa, and an increased drinking regimen (up to 2.5 liters per day), aimed at combating the manifestations of general intoxication of the body.
Drug therapy
Rinse
To stop the spread of infection throughout the oral cavity, as well as to prevent the occurrence of sore throat, anti-inflammatory drugs such as Stomatidine and Miramistin are prescribed. The greatest effect is achieved by repeating the rinsing procedure every 3 hours, strictly adhering to the instructions for medicinal solutions.
Antiviral drugs
To suppress the reproduction of the herpes virus, the patient is advised to take “Immudon” and “Acyclovir” orally according to the scheme, and for external use - “Viferon” ointment or “Silicea” gel.
Vitamin therapy
Tablet vitamin complexes such as “Complivit” help improve immunity.
Attention!
Before use, consultation with a specialist is recommended!
Treatment at home with folk remedies
On the Internet you can often come across the question: “How to treat herpetic stomatitis with folk remedies?” Let’s make a reservation right away: when treating this disease, you cannot rely solely on traditional medicine methods. Therapy must be comprehensive, and only a doctor can choose it correctly.
An effective folk remedy for rinsing the mouth is propolis tincture diluted with boiled water 1:3. In case of pronounced “jams” in the corners of the mouth and painful ulcers inside, applications with natural sea buckthorn oil have an analgesic and wound-healing effect.
Prevention measures
- Strengthening the immune system.
Avoid excessive exercise and stress. Take a multivitamin in the fall and spring. Regular exercise and hardening increase the vitality of the body. - Healthy lifestyle.
Get rid of bad habits: scientists have proven that excessive smoking and alcoholic beverages can become a catalyst for the activation of the herpes virus in the body. - Timely treatment of chronic diseases.
Do not forget that simple stomatitis, if you do not seek medical help in a timely manner, can develop into herpetic stomatitis. Chronic caries and acute respiratory viral diseases suffered “on the legs” also seriously undermine the body’s immune defense. - Maintain personal hygiene.
According to statistics, it is poor oral hygiene that most often opens the way for herpes infection. - Avoid oral trauma.
Even a minor microcrack from a prick with a fish bone or careless use of a toothpick can become an “entry gate” for the herpes virus.
Attention!
With reduced immunity, herpes stomatitis becomes chronic and relapsing: the disease can recur 2-6 months after recovery.
Causes of development of inflammatory diseases
The human oral cavity is inhabited by many beneficial, opportunistic and pathogenic microorganisms, the totality of which is called microflora [2]. Aerobic and anaerobic bacteria, various types of fungi, viruses, and protozoa were found in it [3]. If a person is healthy, the composition of the microflora is balanced, due to which the health of the entire oral cavity is maintained. However, under the influence of various unfavorable factors, general and local immunity can decrease, and the balance of microflora can be disrupted due to the excessive development of certain pathogenic microorganisms
Often these reasons act in a complex manner - against the background of a chronic or acute disease, the patient’s immune defense decreases, which leads to intensive reproduction of a certain strain of microorganisms, its predominance in the intraoral flora and the start of the inflammatory process. For example, candidal stomatitis is caused by fungi of the genus Candida. The causative agent of herpetic stomatitis is the herpes simplex virus.
Risk factors for oral inflammation [1]:
- systemic diseases (diabetes, chronic diseases of the gastrointestinal tract, endocrine and other disorders);
- weakened immunity (for example, due to HIV, unfavorable environmental conditions, hypo- and avitaminosis, poor nutrition);
- past infectious diseases, especially in children (ARVI, influenza, chicken pox) [4];
- long-term use of potent medications, in particular antibiotics;
- unsuccessful prosthetics;
- prolonged stress;
- lack or insufficient oral hygiene ;
- bad habits (smoking), etc.
Thus, it is believed that one of the key reasons for the development of aphthous stomatitis is chronic diseases of the gastrointestinal tract. Oral candidiasis can develop due to long-term use of antibiotics, and leukoplakia can develop in response to constant irritation of the mucous membranes of the lips and oral cavity, for example, with a poorly fitted denture [1].