A tongue burn is an injury that damages the mucous membrane, and in some cases even muscle tissue. This problem brings a lot of discomfort - from pain and the inability to eat or drink liquids to death. It is very important to urgently contact a specialist who, after studying the cause of the burn, will prescribe treatment. If you neglect the help of a qualified dentist, serious complications can occur, including necrotic decomposition of soft tissues and infection of the entire body.
Types of tongue burns
Depending on the cause of origin, the following types of injury are distinguished:
- Chemical burn of the tongue or oral cavity - when tissues are damaged as a result of exposure to aggressive chemical compounds;
- Thermal - when the surface was exposed to a high temperature object.
- Electrical - occurs as a result of tissue contact with electricity. For example, when performing dental procedures. Electric current affects not only the tissues of the tongue, but the entire body as a whole.
Causes of burns and methods of preventing them
The most common cause of burns is contact of oral tissues with liquids or high-temperature steam. The oral mucosa turns red, swelling appears, and then the upper layer peels off. Electrical burns occur due to incorrect electrophoresis. The size of the lesion will correspond to the size of the electrode.
Chemical burns most often occur in children when trying to test household chemicals, but burns sometimes occur in the dental chair. This can occur upon contact with silver nitrate, solutions for cleaning the dental canal, etc. In case of a chemical burn, the severity of the condition depends on the chemical composition of the substance that has entered the mouth and the strength of its concentration. Ionizing radiation is used in radiation therapy and can also cause burns to the mouth and larynx.
It must be said that the method of preventing burns is basic caution. Drinks or food that are too hot should not reach the table. Steam inhalations for children under 14 years of age are extremely dangerous and do not have any therapeutic effect. As for chemical burns in children, household chemicals must be carefully isolated and have warning labels. Do not pour chemical solutions into other containers, especially drinking bottles.
Symptoms of a tongue burn
Symptoms depend on the extent of soft tissue damage:
First degree - a burn occurs due to short-term exposure to high temperature tissue. The patient experiences slight redness and swelling of the mucous membrane. Often, a burn condition is provoked by consuming too hot food or liquid.
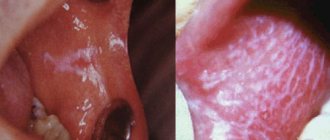
Second degree – swelling of the mucous membrane, redness, and multiple blisters on the surface are observed.
Third degree - accompanied by tissue death, large blisters, redness of the surface, the organ itself seems to “change its consistency.” As a rule, it occurs due to exposure to gases, liquids at elevated temperatures, or chemical compounds.
The fourth degree is a severe lesion when the tissues are charred. This burn condition is rarely compatible with life.
Medical Internet conferences
Relevance: According to WHO, the number of acute and chronic poisonings in children in economically developed countries is increasing from year to year, the cause of death of 20% of children under the age of 15 years is exogenous intoxication. In our country, over the past 5 years, the number of poisonings in children has doubled (an annual increase of 3-15%). Among nosological forms, more than 80% are poisonings with medicinal substances, food and household chemicals, with the maximum number of poisonings (from 77.2% to 85%) occurring between the ages of 1 and 3 years. Accidental use of various chemical substances by children is often accompanied by the development of burns of the upper digestive tract (UGT) of varying severity. In recent years, there has been a trend toward an increase in the number of chemical burns of the esophagus in children, which is explained by an increase in the number and types of aggressive substances, as well as their easy availability to the consumer.
Purpose: to study the outcomes of damage to the upper parts of the VOPT due to the accidental use of various chemical substances by children.
Materials and methods: According to the archives of the KB named after. S.R. Mirotvortsev SSMU conducted a retrospective analysis of 612 case histories of children aged 9 months to 15 years hospitalized with suspected oral poisoning by various chemicals and drugs (2009 – 2013). Signs of poisoning were diagnosed in the emergency room in 544 children and sent for treatment to the children's intensive care unit (DORIT). Due to a suspected chemical burn of the VAPT, 68 children were urgently hospitalized at the children's surgical clinic (DSC). In the conditions of the DHC, all children (100%) underwent a general clinical laboratory examination (CBC, OAM, ECG); instrumental examination was carried out in 43 (63.2%) patients: FGDS - 38 (55.8%) patients, fluoroscopy of the upper digestive tract (UGDT) with Susp. BaSO4 – 5 (7.3%) patients. The children were consulted by an ENT doctor and a pediatrician. The depth of tissue damage in a burn of the esophagus (endoscopic picture) was assessed according to the classification (S.D. Ternovsky, E.N. Vantsyan, 1971). Both conservative and surgical treatment methods were used (bougienage of the esophagus with COOK bougies, gastrostomy placement).
Results. All patients hospitalized at DHC ingested the chemical accidentally due to adult carelessness. Gender distribution: 45 boys (66.2%), 23 girls (33.8%); by age: up to 1 year – 1 (1.5%) child; from 1 year to 3 years - 54 (79.4%) people; from 3 to 6 years – 10 (14.7%) people; 6 to 9 years old – 3 (4.4%) people (diagram 1); average age of patients – 2.17±0.12 years.
A burn to the esophageal mucosa was detected when using acetic essence (acetic acid) in 36 (52.9%) children, alkali - in 10 (14.7%) patients, potassium permanganate crystals - in 17 (25%) patients, and other chemicals ( glue, ammonia-anise drops, ammonia, tincture of iodine, etc.) – in 5 (7.4%) children.
Chemical burns of the mucous membrane of the oral cavity with acid and alkali were clinically manifested by swelling and hyperemia of the lips, hyperemia and bleeding of the oral mucosa, hypersalivation; when consuming potassium permanganate crystals, the mucous membranes of the mouth and tongue turn black. In severe cases, fibrin deposits on the oral mucosa, dysphagia, and dysphonia were noted in 8 (11.7%) people. Complications in the form of acute renal and liver failure were not registered in these children.
Primary FGDS was performed in 47 (69.1%) patients, 4 patients underwent fluoroscopic examination of the VOPT with Susp. BaSO4 within 1 to 7 days. Parents of 12 children refused endoscopic examination (FGDS). The endoscopic picture of a 1st degree burn was diagnosed in 12 children (25.5%), a 2nd degree burn in 8 patients (17%), a 3rd degree burn in 11 patients (23.4%), a burn in 16 cases (34.1%). the esophagus was not endoscopically confirmed (diagram 2). As a result of FGDS, the localization of the burn surface was verified: a burn of the mucous membrane of the upper third of the esophagus was diagnosed in 12 patients, a burn of the mucous membrane of the middle third of the esophagus - in 4 children, a burn at the border of the upper and middle third of the esophagus - in 3 patients, a burn at the border of the middle and lower third of the esophagus - in 1 child, burn of the mucous membrane of the lower third of the esophagus – in 2 patients.
Primary FGDS was not performed in 21 patients. In 5 children there were no clinical signs of a chemical burn of the VA.
Esophageal stenosis as a complication of a chemical burn due to accidental use of chemical substances was diagnosed in 14 (45.2%) patients. All patients with esophageal stenosis underwent therapeutic bougienage using a conductor string, Cook bougies, and in severe cases (III degree burn) - in combination with the application of a gastrostomy.
Chemical burns of the esophageal mucosa were accompanied by inflammatory changes in the hemogram (ESR acceleration - 17.2±2.05 mm/h, leukocytosis - 13.3±1.7*109/l). All children received conservative treatment: gastric lavage, early antibacterial therapy to prevent secondary infection, in order to accelerate epithelization of the mucous membrane, oral sea buckthorn oil, short courses of glucocorticosteroids (5-7 days), enveloping agents (Almagel), infusion therapy as a component of anti-shock therapy ( according to indications). To remove unabsorbed crystals of potassium permanganate and reduce the cauterizing effect of the substance on tissue, the oral mucosa was treated with a swab with 1% ascorbic acid solution.
Conclusions:
1. FGDS is the defining diagnostic method that verifies the diagnosis of “Chemical burn of the esophagus.”
2. Every third child examined endoscopically (22 people (32.3%)) was diagnosed with a burn of the esophageal mucosa due to accidental use of various chemicals. 3. Symptoms of damage to the mucous membrane, revealed during examination of the oral cavity and pharynx, are not reliable signs of the severity of damage to the mucous membrane of the esophagus and stomach.
4. Accidental use of aggressive chemicals (acids, alkalis) by children can lead to the formation of cicatricial stenosis of the esophagus, which negatively affects the child’s quality of life.
How to properly treat a tongue burn?
Treatment methods depend on the type of thermal injury.
What to do in case of a thermal burn of the tongue?
- rinse your mouth with cool water;
- apply ice or a cold object to the damaged area;
- treat the burn site with a disinfectant solution;
- rinse with a disinfectant to prevent bacteria from entering the oral cavity;
- use local anesthetic compounds;
- while the tongue is recovering, eat liquids, fruits and vegetables rich in vitamins C and B. Avoid spicy, pickled foods, foods that can have a mechanical effect on tissue (nuts, crackers, seeds, etc.).
- rinse the mouth thoroughly;
- neutralize aggressive chemicals. Depending on the source of the burn, a specific neutralizer is used;
- After neutralization, the burning sensation should go away. For pain relief, it is worth using anesthetics and antihistamines;
- if the mucous membrane is severely burned, with damage to the structure of the tongue and muscle tissue, it is necessary to urgently go for an examination to a doctor.
If there are bubbles on the surface of the tongue, you should urgently seek help from a dentist! Under no circumstances should you open blisters yourself! You may need hospital treatment under the supervision of a doctor.
How to treat a chemical burn of the tongue?
Note! If the oral cavity is burned with an alkaline solution, it cannot be rinsed with water, since moisture promotes more active penetration into the soft tissues of the tongue.
Clinical researches
Repeated clinical studies have proven that the two-component oral skewers ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component skewers - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Consumer Reviews
Natasha (vseotzyvy.ru)
“Mouth rinse Vertex JSC Asepta mouth rinse is sold in pharmacies, that’s why I bought it, it has more medicinal properties than just a cosmetic product, and indeed this rinse perfectly removes bad breath, disinfects gums, menthol gives freshness for almost a day perfectly helps smokers."
Dilya09 (otzovik.com)
“Hello to all readers of my review! I wanted to tell you my story about how I started using the Asepta oral brush.
It all started with the fact that I had an implant installed instead of an extracted tooth and was given strict instructions to rinse my mouth with chlogrexidine and, preferably, an oral scavenger. At the pharmacy, my choice fell on the Asepta drug, despite the price, because after the implantation procedure I had the feeling that now I would brush my teeth after every meal and rinse my mouth (it was just creepy). The price of this skimmer in pharmacies is above 160 rubles.
It doesn’t taste very nasty like some skimmers; after rinsing, it freshens your breath due to the “Lime” and “Mint” flavors. By the way, I don’t use it regularly anymore, I often forget to rinse my mouth, but, nevertheless, it is always present in the bathroom.
Of course, over the years, the memories of implantation have become dull, much has been forgotten, but Asepta and I are now friends. I take not only the skimmer, but also toothpaste. In general, not only is the skipper good, but the whole series is good. I recommend it to everyone who uses oral skewers.”
How exactly to neutralize a chemical burn in the mouth?
Carbolic acid is well neutralized by glycerol.
Baking soda and water neutralize acidic compounds.
If alkali gets into your mouth, rinse the cavity with citric acid diluted in water.
If exposed to aggressive household chemicals, the mouth should be rinsed with cool running water.
It is important! Tongue burns take a long time to heal. Unfortunately, these tissues cannot be made motionless for a certain time; the tongue is constantly in motion. On average, it can take several weeks for the tongue to recover from injury.
Treatment
The treatment process should begin at the scene of the incident.
For burns caused by chemicals, the poisons must first be neutralized. Burns caused by alkalis are treated with weak acid solutions and vice versa. For burns with ammonia and caustic soda, it is necessary to rinse the throat with a 0.1% solution of hydrochloric acid, and for burns with acid, use a 2% solution of sodium bicarbonate. If they are unavailable, you should use water with added milk or whites from raw eggs. In case of a thermal burn, the affected areas should be lubricated with a 5% solution of potassium permanganate or rinsed with a solution of the same drug, which has a pink color. In the case of second and third degree burns, anti-shock measures are necessary simultaneously with neutralization of the poison, and detoxification is also carried out. The victims require immediate hospitalization in an ENT hospital.
Treatment of a burn to the oral cavity in a child
According to statistics, a large percentage of patients who turn to a doctor for help as a result of a burn to the mouth or tongue are children. Young patients up to a year and older can unknowingly “taste” household chemicals or alcoholic drinks accidentally left on the table by their parents. Also common causes of burns are eating too hot food.
The mucous membrane of a child’s tongue is more delicate and thin, and therefore requires more delicate handling in case of a burn. For treatment, you must urgently contact a pediatric dentist.
How to avoid complications?
In order not to aggravate the situation when treating gum burns, it is important to be attentive to yourself until the injury passes.
- For any type of gum burns, dentists do not recommend eating spicy, sour, or salty foods until the tissues are completely restored. Strong flavors irritate the affected tissues and can significantly prolong the healing process.
- You should not eat too hot foods - both during treatment and in the future, when the gums recover after the burn.
- All medicines, household chemicals, paints, solvents, and building materials must be stored in specially designated areas out of the reach of children.
If the pain from a burn becomes excruciating, we can take painkillers or use light anesthetic gels with analgin or benzocaine.
Complex gum burns, in which soft tissue dies, can only be treated surgically. The doctor in the hospital removes dead pieces of tissue and covers the damaged areas with donor parts. Such a “jewelry” operation often requires repetitions and additions. After treatment, the surgeon must prescribe antibiotics to the patient so that bacteria and microbes do not appear in the wounds and dangerous suppuration does not begin.
We hope that all of the above tips on caring for burnt gums will be for informational purposes only. Be careful and attentive to yourself, and accidents will bypass you.
Sources:
- The problem of treating inflammatory periodontal diseases in patients suffering from type 2 diabetes mellitus E.A. KHROMOVA* Ph.D., Associate Professor of the Department I.V. KULIK* Ph.D., Associate Professor of the Department N.A. UDALTSOVA**, ***candidate of medical sciences, associate professor of the department; Deputy Chief Physician for Organizational and Methodological Work A.K. IORDANISHVILI****,*****Dr.Med.Sci., Professor, Professor of the Department *Department of General Dentistry, North-Western State Medical University named after. I.I. Mechnikov" of the Ministry of Health of Russia; ** St. Petersburg State Budgetary Healthcare Institution “Dental Clinic No. 29”, Frunzensky District, St. Petersburg; ***Department of Maxillofacial Surgery and Surgical Dentistry of the Federal State Budgetary Educational Institution of Higher Education "St. Petersburg State University" of the Government of Russia ****Department of Orthopedic Dentistry of the Federal State Budgetary Educational Institution of Higher Education "North-Western State Medical University named after. I.I. Mechnikov" of the Ministry of Health of Russia; *****Department of Maxillofacial Surgery and Surgical Dentistry of the Federal State Budgetary Educational Institution of Higher Education "Military Medical Academy named after S.M. Kirov" of the Russian Ministry of Defense;
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
Clinic
The clinical picture is dominated by the following symptoms: pain (retrosternal or epigastric), difficulty breathing, drooling, dysphagia, refusal to take fluids, vomiting. The clinical picture does not always predict the degree of damage to the esophagus. One study examining the correlation between the severity of esophagitis and the presence of three symptoms: nausea, drooling and difficulty breathing found that in the absence of all three symptoms, as well as in the presence of only one of them, there was no significant damage to the esophagus, whereas a combination of two symptoms has always been associated with severe damage.
Alkalis
Unfortunately, alkalis are tasteless and practically odorless, which makes their accidental use more likely. Burns of the oral cavity are typical for the use of alkali, but their absence in no way indicates the absence of damage to the esophagus; in 25% of cases, in children with no pathology in the oral cavity, severe damage to the esophagus was observed after consuming alkalis. The stomach is affected in 20-25% of cases. When exposed to alkali on the esophageal mucosa, liquefaction necrosis occurs, quickly spreading to the underlying layers until the alkali is neutralized by tissue fluid. Accordingly, the higher the alkali concentration, the deeper the damage it causes, even to the point of perforation. There are three stages of the effect of alkali on the esophagus: the stage of liquefaction necrosis, the stage of repair and the stage of scarring. Reparation begins on day 5-6 and can last up to 2-3 or more weeks. During this phase, the scab is rejected, granulation tissue appears, and re-epithelialization occurs. Massive deposition of collagen in the third phase leads to the formation of scar strictures.
When to perform endoscopic examination?
Initial endoscopic examination should be performed within the first 2-3 days after injury. Contraindications to it are: shock, respiratory disorders, perforation, mediastinitis.
In the period from 5 days to 3 weeks, during the repair stage, the wall of the esophagus is thinnest and the risk of perforation during endoscopy is very high, therefore, it is highly undesirable to perform it at this time. After three weeks, dense fibrous tissue usually forms and endoscopy becomes safer. In addition to endoscopic examination, radiography of the chest and abdominal cavity, clinical blood test, urea, and liver tests are indicated.
Degree of tissue burns
Doctors distinguish between the following degrees of damage:
- first: slight redness, pain, aggravated by pressure, swelling;
- second: bubbles appear, burning, pain, severe itching, ulcers form in place of the burst bubbles;
- third: severe degree, in which ruptures and wounds form, unbearable pain, and necrosis develops.
Any degree requires the attention of a doctor. It is impossible to treat burns on your own, as this leads to a worsening of the situation, the development of an abscess or necrosis.
First aid and treatment
Before contacting a doctor, the following first aid measures are recommended:
- contact with the irritant should be stopped immediately;
- The mouth should be rinsed with warm plain water;
- in case of severe pain, take a painkiller;
- you need to visit a doctor or call an ambulance.
Treatment is prescribed based on the condition of the patient and tissues, the degree of damage, and the type of irritant. The greatest difficulty is observed with chemical lesions, since the tissues are affected quite deeply. To relieve pain, anesthetics are prescribed, antibacterial agents and rinses are also prescribed.
Traditional methods can only be used on the recommendation of a doctor. These are products such as sea buckthorn oil, decoctions based on oak, chamomile and other herbs. They do not have a serious therapeutic effect, but they alleviate the condition and disinfect the affected area. Such methods are used together with drug therapy, but only under the supervision of a doctor.