Symptoms of caries
Diagnosis of the disease should only be carried out in the dentist's office. But the person himself can determine the presence of this pathology by very characteristic symptoms:
- the appearance of dark spots on the teeth: most often they appear on the chewing surface, but often inflammation develops between the teeth (but it is usually not possible for the patient to see this - special equipment will be required),
- there is a roughness of the surface of the teeth,
- When eating food, aching pain appears, teeth react to sweet and sour, as well as cold and hot. But the unpleasant sensations subside immediately as soon as contact with the irritant ceases - this is how caries, even deep ones, differs from pulpitis - inflammation of the dental nerve,
- Breath odor may become unpleasant,
- a carious cavity can even be felt with the tongue; food debris often gets clogged into it, which causes discomfort or even swelling of the tooth - for example, if a small gap appears under a filling.
Periodontitis
If the carious process is complicated by pulpitis, which is not treated, inflammation of the tissues surrounding the causative dental unit develops. Symptoms of periodontitis are bleeding of the gingival margins during hygienic sanitation of teeth and an unpleasant odor emanating from the oral cavity. Possible pain from thermal irritants.
Periodontitis is classified into acute and chronic. In an acute process, severe pain occurs, which intensifies with load on the causative tooth. Pain symptoms can also arise from the action of thermal irritants. The gums around the causative tooth become swollen, hyperemic, an abscess often appears, which spontaneously opens and purulent contents come out through it, after which the patient’s condition improves. Patients note that the causative tooth becomes higher than other dental units in the jaw.
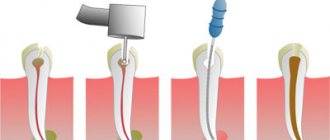
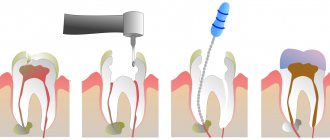
Treatment of acute periodontitis consists of opening the pulp chamber, through the resulting defect the tooth is cleansed of purulent contents or pulp decay. To make this process go faster, dentists at Dr. Granov’s clinic recommend rinsing the mouth with a soda-saline solution. After 2–3 days, the inflammatory process stops and the tooth can be filled. If the patient’s condition does not improve, then an incision is made into the mucous membrane and periosteum in the area of the periodontitis tooth, and a rubber drainage is placed into the resulting incision. If this does not give a positive result, then the tooth is removed.
If the acute form of periodontitis is not treated, then after 7–14 days the process becomes chronic. Symptoms of chronic periodontitis:
- Excessive tooth mobility.
- Gaps appear between the teeth.
Reasons for the development of the carious process
The development of caries largely depends on the individual characteristics of the body. For example, in women with hormonal imbalances, plaque accumulates on the teeth more often, which leads to an increased attack from bacteria. In general, caries is caused by pathological microorganisms, which become much more numerous in the oral cavity than good bacteria. And their appearance is caused by the following reasons:
- lack of proper hygiene: brushing your teeth for 20-30 seconds in the morning and evening is very little. Dentists' recommendations are at least 2 minutes twice a day, as well as removing food debris that accumulates in narrow spaces after eating. Gradually they transform into plaque, which is a provocateur of many dental diseases, including caries,
- poor nutrition: excessive consumption of sweet foods and changes in the PH composition of saliva - all this again contributes to the formation of plaque and an increased attack of bacteria,
- age: it has been established that the destructive processes of primary teeth actively develop in the first years of children’s lives. As you get older, the likelihood of developing dental diseases decreases. This is influenced by the fact that adults pay more attention to oral hygiene. In old age, the risk of caries increases again - this is the result of various diseases of the body and insufficient oral hygiene,
- pregnancy and lactation, that is, during those periods when a woman loses many vitamins and minerals, in particular calcium and fluoride,
- lack of vitamins and, as a result, increased fragility of tooth enamel,
- genetics: a predisposition to many diseases of the gums and teeth is passed on from parents.
Caries and its causes, classification and effect on the body
Caries (lat. caries - “rotting”) is a pathological process in the hard tissues of the tooth, which develops under the long-term complex influence of unfavorable external and internal factors and leads to softening of hard tissues and the formation of defects in the form of cavities. Caries, if left untreated, disrupts the chewing process up to the complete loss of this function, therefore, has an extremely negative effect on digestive function and causes diseases of the gastrointestinal tract. In general, caries has a negative impact on the general condition of the body and on a person’s quality of life, being a constant source of infection and intoxication.1
Treatment methods
Cure caries, especially at the initial stage, is not difficult - this involves removing the inflamed tissue and then filling it. In the presence of deep lesions, binoculars and a microscope can be used, which allow you to increase the working space and remove even the smallest inflamed cells, while preserving healthy tissue. Depending on the situation, it may also be necessary to restore the coronal part if it has been severely damaged.
Fissure sealing A method that allows you to stop the carious process. Essentially, this is the prevention of inflammation. Fissures or depressions (grooves) on the surface of the enamel are filled with a special sealant, which evens them out and thereby prevents the accumulation of bacteria and plaque.
Price:
from 2500 rubles more details about the solution
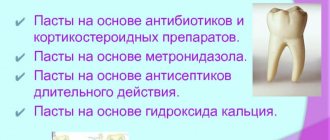
Treatment of caries If the doctor notes caries at the spot stage, then the main procedure is remineralization (restoration of the required mineral content) using a special solution. If the caries is superficial, medium or deep, then the resulting cavity will need to be treated, followed by filling using composite materials. When the carious process penetrates into the deep layers, it is advisable to use medicated pads containing calcium hydroxide - this way additional protection is created to preserve the dental nerve.
Price:
2500 rubles more details about the solution
Installing an inlay In a number of situations, when the tooth is quite badly damaged and a large filling will not hold, you can develop an individual inlay made of ceramic or zirconium dioxide. It will accurately follow all the curves of the tooth and be securely fixed inside the cavity. At the same time, it will last many times longer than a large filling.
Price:
from 20,000 rubles more about the solution
Introduction
In recent years, thanks to the introduction of new technologies, instruments and materials into endodontic practice, there have been positive trends in increasing the effectiveness of endodontic dental treatment, but this does not mean that in clinical dentistry the number of unsuccessful treatment outcomes for complicated caries has currently decreased. The success of primary endodontic treatment in Russia remains at a fairly low level of 32%. The main errors that occur during endodontic treatment are:
- tooth perforation;
- breakage of an endodontic instrument or pin in the root canal;
- poor-quality passage and expansion of the root canal;
- inadequate antiseptic treatment of the root canal;
- poor quality filling (obturation) of the root canal.
The effectiveness of endodontic treatment is guaranteed by three components: cleaning, sterilization and obturation of the root canal system. And at each stage of endodontic treatment there is a significant number of errors and, as a consequence, the development of complications. Thus, according to an X-ray study, it was found that only in 13.4% of cases the root canals were filled satisfactorily. Even with high-quality obturation, inflammation in the periodontium is observed in 5-8% of cases.
Features of the anatomy and topography of all groups of teeth
The structure of the root canal system differs from each other in different groups of teeth. They have additional, lateral channels, which can branch off from the main one at any level and have different configurations - from simple to complex. In structure, root canals can be compared to the crown of trees. Currently, there are 9 types of root canal structure. Type I - there is one root canal, which begins at the bottom of the pulp chamber and continues, gradually narrowing to the apex of the root. This type of root canal is most often found on the upper central incisors. Treatment of teeth with this type of canal structure is not difficult. Type II - the structure is represented by two root canals, which open at the bottom of the pulp chamber separately from each other, and near the root apex they merge into a common lumen, which ends in one apical opening. The root systems of the lower incisors and upper premolars most often have this structure. Type III - one orifice and one root canal open at the bottom of the pulp chamber; along the course of the root, the common canal bifurcates in the lower third of the root into two independent canals, which then unite again at the apical part and open with a common opening. This configuration is observed in the teeth of the lateral groups.
Type IV - characterized by the presence of two independently running root canals in one root, which in the area of the root apex open with two independent apical openings. The lower molars, premolars and lower incisors have this type of root canal. This is a fairly simple anatomical situation for endodontic treatment. Type V is characterized by the presence of one canal inside one root, but near the root apex the common canal is divided into two ending with independent apical foramina. This type is more often observed in the lower premolars. In some clinical situations, it can be quite difficult to treat both branches to the apical foramen. Type VI - two canals open at the bottom of the pulp chamber of the tooth, which unite into a common canal approximately in the middle of the root length, and then again divide into two independent passages and open with two apical openings. This structure of the canal system is difficult to process and fully clean the entire lumen of the root canal.
Type VII has the following structure: one root canal begins at the bottom of the pulp chamber of the tooth, then narrows towards the middle of the root like an hourglass, then it is divided into two independent canals, which in the apical part again unite into a common canal and immediately at the apex of the root they re-branch and open with two apical openings. This type is very complex and is observed in the teeth of the lateral groups of the lower jaw. Type VIII - 3 independently running root canals in one root. This type of structure is very simple and is found in various morphological groups of teeth. However, the incidence of this type of root canal structure is not very high. Type IX - the presence of 3 root canals along the entire length, which are then combined into one canal. This type is found in wisdom teeth.
It is necessary to highlight some structural features of the root canals of teeth of different groups. Endodontic treatment of the central upper incisors is not difficult, but sometimes there are clinical situations when there may be 2 canals at the root of the central upper incisor. During instrumentation of the lateral incisor canal, problems such as perforation or apical displacement can sometimes occur, especially when using rigid or large files, since about 70% of the upper lateral incisors have a pronounced distal bend. The lateral incisors, just like the central ones, can have 2 canals in one root. Endodontic treatment of the upper canines can be problematic during root canal treatment, since their structure has a buccal curve at the root apex (last 2-3 mm). There is also evidence of the presence of a canine structure with 2 canals. The most difficult is endodontic treatment of the lower incisors. In 40% of cases there are 2 channels. To create conditions for straight-line access of endodontic instruments, the tooth cavity is expanded in the vestibular-lingual direction, and the width of access must correspond to the width of the pulp chamber. Treatment of the lower canines can also cause problems with endodontic treatment, since in 10% of cases the lower canines may have 2 canals. An atypical form with the presence of 2 roots may also occur. In this case, the main difficulty in treating the root canal is the passage of both branches. However, this task will require pre-bending of the tools. The difficulty in treating upper premolars is that the apical part of the root canal ends in very narrow and curved apices. Therefore, these channels should be treated with care and precision. Often, in the area of the bottom of the pulp chamber, you can see a common mouth and a division into 2 independent canals, which runs significantly below the neck of the tooth, which makes it difficult to access the pulp chamber. In addition, the upper premolars may have 3 canals, 2 buccal and one palatal. When treating lower premolars, the dentist must remember that these teeth have a rather complex canal structure system; in 20% of cases there are 2 canals, buccal and lingual. In most cases, the buccal canal is located more directly, and the additional, second canal is located lingually. In some cases, lower premolars may have 3 canals. The lower second premolars may also have 2 roots. When forming a tooth cavity, the walls of the burr hole of the lower premolars should smoothly transition into the wall of the pulp chamber and reach the tops of the cusps. It is also important to take into account the anatomical location of the mental foramen and the vessels and nerves passing through it. Due to the proximity of these structures, an acute inflammatory process in the area of the lower premolars can cause temporary paresthesia. Exacerbation of the pathological process in this area is more pronounced and more difficult to treat conservatively. The upper first molars have a complex anatomical and morphological system. Therefore, during root canal treatment of these teeth, the highest percentage of endodontic errors and complications is observed. There is evidence that in 95% of cases there are 2 canals in the mesial-buccal root, which looks like spread out, flattened, and this determines the presence of 2 canals. The additional canal is identified on the line connecting the main mesiobuccal canal and the mouth of the palatine canal. The orifice of the main mesial-buccal canal, as a rule, is located almost under the apex of the mesial-buccal cusp of the crown, and the mesial-palatal orifice is located closer to the center relative to the apex of the mesial-palatal cusp. In dentistry, there are clinical cases where the upper first molars may have 3 canals in the palatal root and even 2 palatal roots. Therefore, the dentist must carefully examine the bottom of the tooth cavity to identify all existing canal mouths. The upper second molars are characterized by significant diversity in structure. For example, they have 2 mesiobuccal, 2 distobuccal, 2 palatal roots and canals. There may be one root and one canal, 3 roots and 3 canals, there may be cases of a two-root structure with 2 canals and even the presence of 4 roots, sometimes 3 roots fused together. In lower molars, in 30% of cases, 4 canals can be found: 2 canals in the distal root and 2 in the mesial root. These teeth can have 3 roots. The third root is distal-lingual. It is necessary to identify and treat all existing root canals, since “skipping” any of them will subsequently lead to the development of an inflammatory process in the periodontium. Along with knowing the percentage of the number of root canals, knowledge of the average (calculated) length of the root canal is also important, which helps to initially set the working length. However, we should not forget about the individual characteristics of the length of the root canals. For example, the average length of a lower molar ranges from 20 to 21 mm. In clinical practice, there are canals of this group of teeth up to 26 mm long.
The most important condition for achieving positive results in endodontic treatment is the formation of correct access to the root canal. Basic requirements for the formed tooth cavity: - there should be no overhanging edges or undercuts; — the entrance to the cavity should be straight and smooth. For all teeth of the frontal group, the entrance to the pulp chamber in 95% of cases passes through the cutting edge or near the cutting edge. The endodontic instrument must enter the root canal freely and not bend, this is especially important when using rotating nickel-titanium instruments. When forming a dental cavity in the chewing group, access must fully correspond to the volume of the roof of the pulp chamber. In some cases, it is necessary to excise part of the wall of the tooth crown. However, in this case, one must be guided by the principles of biological expediency, since the removal of an excessive amount of hard tooth tissue (removal of part of the tooth) leads to a decrease in the tooth’s resistance to stress.
Dentists - attention: diagnostics
Already at the diagnostic stage, as well as in the subsequent process of endodontic treatment, errors can be made. Examination of patients is of great importance for making an accurate diagnosis:
- careful history taking;
- analysis of patient complaints;
- analysis of the results of an oral cavity examination.
Dentistry and statistics show: a large number of diagnostic errors are due to insufficient frequency of X-ray examinations. According to literature data, in private clinics, diagnostic X-rays for inflammation of the dental pulp are performed in 19% of cases, and in municipal institutions - only in 8%. Neglect of the mandatory X-ray examination procedure before the start of endodontic treatment, which makes it possible to study the anatomical features (the number and configuration of roots and canals, the size and structure of the pulp chamber), the angle and radius of curvature of the root canals, as well as to objectify the criteria for the degree of root formation, leads to the occurrence of perforations of the cavity bottom tooth, root canal walls, over-expansion of the root canal, apex transportation, under-detection of the main and additional root canals, etc. During the process of endodontic treatment, the doctor, using an x-ray method, controls the working length and the degree of mechanical treatment of the root canals, and also determines the quality of obturation and long-term results of treatment. However, when conducting an x-ray examination, it is important to observe patient safety in order to avoid excessive radiation exposure. For this purpose, at certain stages of treatment, the electrometric method using an apex locator is used. An important problem is also the lack of knowledge by practicing doctors of the anatomical and morphological features of the structure of root canals and the percentage of their number.
How to relieve pain
Even mild pain can cause many problems. They are distracting and annoying, so it’s only logical to take steps to eliminate them.
Important: we are talking about pain, which is a consequence of the treatment of deep caries and is not a symptom of complications. You can reduce it and at the same time speed up the tissue healing process in the following ways:
- taking painkillers;
- rinsing the mouth with a soda-saline solution;
- rinsing and bathing with a decoction of sage and chamomile;
- temporary removal of hot and cold foods from the diet;
- refusal of spicy, sour, and also too hard foods;
- avoiding too much stress on the tooth;
- quitting smoking and alcohol.
If the treatment procedure was carried out correctly, the pain will begin to subside on the third day and completely disappear on the fifth day.
Recommendations for eliminating the causes of pain in a filled tooth
If you experience discomfort or pain in a filled tooth, it is recommended:
- eliminate the load on the diseased tooth;
- seek professional dental care immediately;
- stop using traditional medicine.
Procedures related to filling replacement, removal of granulomas and cysts are performed on an outpatient basis and do not require much time.
At the same time, timely seeking dental care at a 24-hour dentistry allows you not only to get rid of unpleasant symptoms in the shortest possible time, but also to prevent the development of serious complications.