Today, one of the pressing problems of modern dentistry remains the treatment of caries and its complications. At the same time, modern requirements for dental restoration are such that treatment should be minimally traumatic with a maximum service life of the restorations.
However, the problem of choosing structures, be it a simple restoration, an inlay or a crown, always remains a stumbling block and causes controversy among specialists from different countries. This publication, of course, will not resolve these disagreements. The purpose of the article is to demonstrate the benefits of treating cases of complicated caries using modern dental materials.
The greatest practical significance are those methods of treating patients that, at a minimum, do not reduce the average service life of the restoration, but reduce the cost for the patient and the time spent in the chair.
At the same time, the time spent on all visits to treat similar nosologies is equally expensive for both the patient and the doctor. Saving time for the patient reduces his stress and fatigue from treatment, which increases his motivation to “get treated quickly” and reduces the risk of the patient leaving the clinic due to long-term treatment.
Saving time for the doctor reduces fatigue and increases the turnover of funds and fixed assets of the clinic, i.e. the doctor can accept a new patient in the time freed up from multi-stage treatment and receive additional income, which at the end of the year can amount to plus several tens, or even hundreds of thousands rubles The main question remains: how to do this without losing quality.
Content
- Dental restoration methods
- Dental restoration with pins
- Dental restoration with inlays
- Dental restoration with crowns
The success of endodontic treatment largely depends on the subsequent restoration of the upper part of the tooth. It is the correct restoration of the crown after filling that is the key to a long-term, high-quality result without the risk of re-infection. Canal treatment is not considered complete until the doctor can guarantee that there is no risk of re-contamination.
Carrying out treatment
All manipulations are performed under local anesthesia. The tooth to be treated is prepared, the pulp affected by caries is removed, after which the canals are cleaned to ensure easy access for dental instruments.
The root canals are mechanically processed and chemically disinfected.
For mechanical treatment of root canals, special tools are used - files; they are somewhat similar to a needle with a rough surface resembling a saw. Files vary in size, length and taper. Since the root canal must be processed along its entire length with files, up to the apical foramen (but in no case beyond it), it is extremely important to find out its length. To do this, the dentist places files into the root canals and takes an x-ray.
After this, chemical disinfection is carried out by irrigating the root canals with special needles.
When the canals are completely dry, you can begin filling them. Gutta-percha and pastes are most often used for this purpose. Gutta-percha is a cone-shaped rubber rod that is coated with a paste and placed into the root canal. Then a temporary filling is placed on the tooth, which is replaced with a permanent one at the next appointment.
| Tooth destroyed by caries, inflamed pulp | Mechanical treatment of root canals with a file tool | Filling canals with gutta-percha, filling a tooth with a temporary and then permanent filling | For further protection, the tooth can be covered with a porcelain crown. |
Methods of dental restoration after endodontic treatment
Severely damaged teeth must be strengthened with additional means. This will help avoid fracture of the tooth stump and maintain its strength for a long time. Intra-canal pins and stump inlays are used as support. The choice of support element depends on how badly the tooth is damaged and what method will be used to restore it. Installation of an intracanal pin is advisable if there are only two walls of the crown, the height of which should not be less than three millimeters.
Unsealing of root canals and their treatment
Today it is no secret to anyone that the primary treatment of complicated caries, as well as orthograde revision of the root canal system, should be carried out using a rubber dam. With this type of isolation of the surgical field, it is possible to successfully carry out excavation of caries, opening of the tooth cavity, mechanical and medicinal treatment of the root canal system.
The Start-X™ ultrasonic tip system is very suitable for opening canal orifices and searching for additional canals.
For primary navigation and widening of narrow canals, today's flexible and durable nickel-titanium continuous rotation PathFile™ files are indispensable.
This very convenient range of instruments, consisting of 3 files, reduces the risk of fracture of the main file when expanding the root canal system, especially in severely curved sections. Next, if everything went well and the doctor confidently treated the root canals, he will have to obturate them. This can be done using both the good old method of lateral condensation of gutta-percha, and vertical condensation using various devices for heating gutta-percha and its condensation. For example, using the Calamus® Dual system for vertical condensation or the new Gutta Core™ obturator, which solves the problem of a plastic carrier that made it difficult to unfill the root canal in the long term. So, we have everything for root canal obturation, essentially, in one visit.
We have gone through and expanded the canal system well, treated it with sodium hypochlorite solution, etc., and if there are no direct indications for temporary medicinal investment and we have done everything according to the protocol recommended by the manufacturer of instruments for processing the canal system, we can dry the root canal well (no exudation and bleeding), nothing prevents us from obstructing it immediately.
We don't need another visit, for which both the patient and the doctor still need to find time. Time for coffee, time to prepare the office and chair, put on an apron, ask about the patient’s well-being, listen to the answer... say goodbye. All this can be avoided (and accepted at the next visit of a new patient) if you follow the recommended parameters of treatment and work with materials and instruments.
Selection of sealer
We just need to add to the above a neutral polymer sealer for obturation, which will allow you to enjoy all the benefits of adhesive dentistry in the same visit. As we know, oil-based sealers, for example, do not provide such an opportunity. Particularly convenient in the automatic mixing system, AH Plus® Jet™ polymer sealer is ideal for our one-visit treatment concept. And in combination with the AH Plus® cleaner system, a special composition of alcohols, it will not only obturate, but also clean the walls of the tooth cavity from sealer and prepare them for standard adhesive technology immediately after filling. If everything is so simple, why do we need to wait until the next day to finally restore the tooth?
You should probably wait for the final polymerization of the sealer. What happens to the sealer during polymerization? If we accept the statement that hot gutta-percha shrinks as it cools to body temperature (i.e. almost instantly), then the sealer remains shrinking for 8 hours before hardening at 37 degrees. The shrinkage of the AH Plus® sealer is 1.76%; if we imagine a thin film of sealer and its actual volume along the canal walls, we get negligible shrinkage and a negligible effect on the final restoration. And if so, we can not wait for the sealer to harden and completely restore the tooth in one visit, if there is no doubt that this work can be completed in one patient visit. The risks of such treatment are minimal (always at the discretion of the doctor), but the benefits are enormous. If we take into account the reduction in fatigue of the patient and the doctor, the saving of time and money for both the clinic and the patient, the absence of bacterial contamination, the tightness of the system, etc., there are practically no advantages. The only thing is that the doctor needs to understand the future fate of the tooth being restored and competent planning of possible prosthetics. But even here we get a tooth almost ready for prosthetics. According to some researchers (Sorensen JA, Martinoff J T., et al.), after covering with crowns, only about 50% of endodontically treated teeth survive in a 5-year period. It is important that resistance to fractures is determined to a greater extent by the presence of hard dental tissues and the location of the defect, and to a lesser extent by the method of post-endodontic restoration.
Restoration with pins
Modern dentistry is increasingly using fiberglass pins, abandoning the usual metal pins and cast inlays. Fiberglass itself does not have enough strength, but when properly combined with composite materials, the tooth receives a very strong fixation. The material has elasticity close to natural dentin. Another advantage of fiberglass reinforcement is aesthetics. The fiber is transparent and will not spoil the appearance of the tooth after restoration.
PROMOTION
Ceramic veneers
RUB 12,500
Pin installation
The pin is installed in the root canal of the tooth, filled with gutta-percha, at the end of endodontic treatment. To do this, part of the gutta-percha is removed, a pin is inserted into the canal and fixed with cement. The top of the tooth is covered with filling material in order to restore its anatomical shape. If necessary, an artificial crown is placed on the tooth.
Installation of root pins and pin inlays is an important stage in tooth restoration using fixed dentures.
If the crown part of a tooth is completely destroyed, it is restored using standard pins, cast core inlays, standard pins made of carbon fibers, and other structures.
Three complex curvatures of one root canal
initial situation
Complaints of discomfort in the area of the upper right incisors and the presence of a fistula. Lateral incisor with a “creeping” composite restoration of reduced aesthetics, dark color of the cervical part; endodontic treatment was not performed. A Straumann implant with a narrow neck is installed in the area of the central incisor. At the implantation stage, the neurovascular bundle of tooth 1.2 was disrupted, which caused pulp necrosis.
Formation of access
Analysis of the radiograph of 1.2 teeth revealed 3 severe curvatures of the root canal (Fig. 34).
Rice. 34. X-ray 1.2 with a gutta-percha cone in the fistula tract
When opening the cavity, hemorrhagically altered replacement dentin was discovered:
| Rice. 35 ac. Formation of access to the mouth of the root canal of 1.2 teeth |
Extremely atypical anatomy - the mouth of the root canal is located not at the bottom of the pulp chamber, but on the wall!
Instrumental cleaning, irrigation and disinfection
It is very difficult to effectively irrigate a curved root canal without proper instrumentation; in this case, it is a silicone nozzle for a syringe manufactured by Vista Dental Products (Fig. 36):
| Rice. 36. Flexi-Glide Silicone Tip, Vista Dental Products |
The root canal is expanded with ProTaper instruments (Fig. 37) with copious irrigation with hot 5% sodium hypochlorite (NaOCl) solution; ProTaper Protocol: Printed Version - Clifford J. Ruddle. Form of success. // Clinical endodontics. – 2007.– Volume 1. – No. 1-3.– P.3-9
| Rice. 37 ac. Shape of the root canal mouth of 1.2 teeth: sequential increase |
At the end of the medicinal treatment, photodynamic sterilization of the lumen and walls of the root canal was carried out with tolonium chloride solution at a concentration of 12.7 mg/l (Fig. 38):
| Rice. 38. Photoactivation of the sterilization process |
Obturation and restoration
The root canal of 1.2 teeth was filled using the vertical condensation technique of hot gutta-percha according to Schilder; the coronal part and palatal surface were restored with a hybrid composite (Fig. 39, 40).
| Fig.39. Gutta-percha level – 2 mm below the periodontal junction | Fig.40. Completed direct restoration |
X-ray inspection
The 3D root canal is obturated, repeating the anatomical configuration, the apical curvature and delta are sealed (Fig. 41).
Rice. 41. Control radiograph 1.2
Control inspection
- A week later: no complaints, the fistula closed.
- The patient was recommended to remove the implant, orthodontic treatment, followed by bone grafting and correct installation of the implant in position 1.1 of the tooth.
conclusions
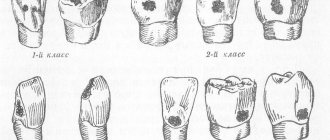
1. Laboratory studies have shown that restoration of teeth after endodontic treatment with dual-curing nanocomposite materials in combination with a fiberglass-reinforced composite pin leads to an increase in their strength: in the presence of three walls of the coronal part (class II according to Peroz, IROPZ 0.5-0.6) — by 3.9±5.8% ( p
>0.05), in the presence of two (III class according to Peroz, IROPZ 0.6-0.7) and one wall (IV class according to Peroz, IROPZ 0.7-0.8) - by 12.6±5, 9 and 24.2±4.2%, respectively (
p
<0.05), compared to teeth where similar defects in the coronal part were restored only with dual-curing nanocomposite material containing zirconium oxide.
2. The use of support for restoration in the form of fiberglass composite-reinforced pins (LuxaPost) significantly reduces the number of clinical complications associated with the destruction of restorations in the first two years after treatment by 12.8% with two intact walls (Peroz class III, IROPS 0 .6–0.7) and 27.5% with one intact wall (IV class according to Peroz, IROPZ 0.7–0.8) of the coronal part of non-vital teeth, compared with the restoration of the above defects only with dual-curing nanocomposite material ( p
<0,05).
3. Restoration of teeth of classes III and IV according to Peroz (IROPS 0.6-0.8) after endodontic treatment should be carried out using fiberglass composite-reinforced pins, since this method leads to a significant reduction in the number of clinical complications associated with the destruction of restorations in the long term. observations ( p
<0.05).
For the restoration of Peroz class II teeth (IROPS 0.5-0.6) after endodontic treatment, it is sufficient to use a dual-curing nanocomposite material containing zirconium oxide, since no statistically significant differences in strength characteristics were found with teeth restored using fiberglass composite-reinforced pins ( p
>0.05).
Results and discussion
Laboratory results
An analysis of the results of a study of the physical and mechanical properties of the LuxaCore-Dual and LuxaCore Z-Dual materials showed that the diametric strength of samples from the LuxaCore Z-Dual nanocomposite was 64.40 ± 3.59 MPa. The corresponding values for LuxaCore-Dual were 20.37±5.35% less and amounted to 51.28±3.45 MPa ( p
<0.01).
The average flexural strength of LuxaCore Z-Dual samples was 107.92±8.71 MPa. This strength parameter for LuxaCore-Dual was 91.83±7.06 MPa, which is 14.97±6.53% less ( p
<0.01).
The results of laboratory studies to assess the influence of the degree of destruction of the coronal part of teeth restored with LuxaCore Z-Dual nanocomposite material on their resistance to compressive loads are reflected in Table. 3. Significant differences were revealed in the influence of the degree of destruction of the coronal part of the tooth restored with the LuxaCore Z-Dual nanocomposite material on the strength characteristics. Thus, the absence of one side wall of the coronal part of the tooth (class II according to Peroz, IROPZ 0.5-0.6) leads to a decrease in its strength by 9.5 ± 3.4%, compared with the strength of intact teeth ( p
<0.05).
Absence of two walls (Peroz class III, IROPV 0.6-0.7) - by 20.6±5.0% ( p
<0.05).
The absence of three lateral walls of the coronal part, which is typical for class IV defects according to Peroz (IROPD 0.7-0.8), leads to a decrease in the tooth strength index by 33.3±6.7%, compared with intact teeth ( p
< 0.05).
Table 3. Comparative assessment of the strength of test samples of teeth with varying degrees of destruction of the coronal part, restored with LuxaCore Z-Dual nanocomposite material (groups I-III), and restored with nanocomposite material supported by a fiberglass composite-reinforced pin (groups A, B, C) Note .
* — p<0.05. When using a fiberglass composite-reinforced pin when restoring a tooth with three preserved walls after endodontic treatment (group A, Peroz class II, IROPS 0.5-0.6), the tooth strength was on average 6.0±5.3% less ( p
<0.05), compared with the strength of intact teeth (Table 3).
When testing samples of teeth with two (group B, class III according to Peroz, IROPS 0.6–0.7) and one (group C, class IV according to Peroz, IROPS 0.7–0.8) intact walls, restored with nanocomposite restoration with support on a fiberglass composite-reinforced pin, the differences in the strength of teeth with intact teeth were 10.6 ± 4.7% and 17.2 ± 2.8%, respectively ( p
<0,05).
The results of a comparative laboratory study to study the degree of influence of a fiberglass composite-reinforced pin on the strength of non-vital teeth with varying degrees of destruction of the coronal part, restored using nanocomposite material and fiberglass composite-reinforced pins (groups A, B and C), with the strength of teeth restored only with double nanocomposite curing (groups I, II and III), are reflected in table. 4.
Table 4. Comparative assessment of the strength of teeth restored with nanocomposite material (groups I, II and III) and glass fiber composite-reinforced posts with nanocomposite material (groups A, B and C) Note. * — p>0.05; ** — p<0.05.
Thus, the destruction of dental samples after endodontic treatment with three intact walls (group A, class II according to Peroz, IROPS 0.5-0.6), where fiberglass composite-reinforced pins were used for restoration, occurred at a load of 402.73 ± 22. 40 N, which was 3.9±5.8% more than the strength of the tooth samples (group 1), where a similar defect was restored using only nanocomposite restoration ( p
>0,05).
Strength of non-vital teeth in the presence of two (group B, class III according to Peroz, IROPZ 0.6-0.7) and one (group C, class IV according to Peroz, IROPZ 0.7-0.8) retaining walls using fiberglass reinforced composite pin was significantly greater by 12.6±5.9% and 24.2±4.2%, respectively ( p
<0,05).
Strength of teeth with three preserved walls (Peroz class II, IROPS 0.5-0.6), when restored using fiberglass composite-reinforced pins (group A), compared with teeth whose crowns were restored only with nanocomposite material (1 -th group), had a statistically insignificant tendency to increase ( p
>0,05).
Thus, as the results of our laboratory study showed, only in case of significant loss of hard tooth tissues (classes III and IV according to Peroz, IROPS 0.6-0.8) the use of fiberglass composite-reinforced pins as a retention support for nanocomposite restoration significantly increases the strength of teeth samples restored after endodontic treatment by 18.4±8.2%, compared with samples where the above pins were not used ( p
<0,05).
Clinical trial results
The results of clinical studies based on assessing the quality of our restorations according to Ryge criteria, as well as data from x-ray examination and electrometry of the teeth, performed 24 months after completion of treatment, showed that among teeth with three intact walls (II class according to Peroz, IROPS 0.5 -0.6), where the restoration of the coronal part was carried out using fiberglass composite-reinforced pins, the number of restorations with good results was 87.5% ( n
=21).
The number of restorations rated as satisfactory was 12.5% ( n
= 3). No unsatisfactory results were identified (Fig. 1).
Rice.
1. Long-term results of treatment of teeth with three intact walls of the coronal part (%). Main group - the restoration is made with a nanocomposite material supported by a pin; comparison group - restoration was made with nanocomposite material. In the comparison group, in patients who underwent restoration only with dual-curing nanocomposite material, with three intact walls of the coronal part of the tooth (Peroz class II, IROPZ 0.5-0.6), the score “good” was 87.0%, “ satisfactory" - 13.0% of restorations in this subgroup; no unsatisfactory results were noted.
Thus, we did not find significant differences in the results of treatment of teeth with three intact walls (class II according to Peroz, IROPZ 0.5-0.6) depending on the method of restoring the coronal part ( p
>0,05).
In the subgroups of the main group and the comparison group, which included teeth with two intact coronal stacks (Peroz class III, IROPD 0.6–0.7), the following distribution of results was observed (Fig. 2). When restoring the coronal part of a tooth with two preserved walls using a dual-curing nanocomposite supported by a glass fiber composite-reinforced pin, good results were noted in 61.5% of cases ( n
=16), satisfactory - in 19.2% (
n
=5).
Unsatisfactory results were identified in 19.2% ( n
=5).
Rice.
2. Long-term results of treatment of teeth with two intact walls of the coronal part (%). Main group - the restoration is made with a nanocomposite material supported by a pin; comparison group - restoration was made with nanocomposite material. When restoring teeth with two intact walls (Peroz class III, IROPZ 0.6-0.7) with one dual-curing nanocomposite material (comparison group), good treatment results were noted in 52.0% of cases, satisfactory - in 16.0% cases. In 32.0% of cases, the quality of the treatment provided was considered unsatisfactory (Fig. 2).
Thus, when analyzing the results of treatment of teeth with two intact coronal walls (class III according to Peroz, IROPS 0.6-0.7), it was found that when restorations were carried out only with nanocomposite material, the number of good results in this subgroup decreased by 9.2% , and the number of complications increased by 12.8%. The differences were significant ( p
<0,05).
When restoring teeth with one preserved wall of the coronal part (class IV according to Peroz, IROPZ 0.7-0.8) using a fiberglass composite-reinforced pin (main group), the number of results assessed by us as good was 48.0%. At the same time, the number of satisfactory results was noted in 36.0% of cases, and unsatisfactory results in 16.0% of cases.
While good results in the subgroup of teeth with one intact wall (IV class according to Peroz, IROPD 0.7-0.8), restoration of which was performed with nanocomposite material (comparison group), were noted for 12 (52.2%) restorations, the quality of treatment was considered satisfactory in 1 (4.3%) case. The highest percentage of complications (43.5%) occurred in restorations of this subgroup, which indicates the inadequacy of the method of restoring the coronal part of teeth only with nanocomposite materials for this type of defect in the coronal part (Fig. 3).
Rice. 3. Long-term results of treatment of teeth with one intact wall of the coronal part (%). Main group - the restoration is made with a nanocomposite material supported by a pin; comparison group - restoration was made with nanocomposite material.
Thus, in teeth with one intact wall (class IV according to Peroz, IROPZ 0.7-0.8), we noted significant differences between the restoration of the coronal part only with nanocomposite material and a nanocomposite supported by a fiberglass composite-reinforced pin in the amount of “satisfactory” and “unsatisfactory” treatment results. The number of satisfactory results was 31.7% less when carrying out restorations with dual-curing nanocomposite material than when using fiberglass composite-reinforced posts and nanocomposite materials ( p
<0,05).
The results of an electrometric study of the marginal fit of restorations in all subgroups of the main group and the comparison group at the end of the observation period were on average identical and amounted to 1.8±0.3 μA. It is worth noting that we have not obtained reliable data on the influence of the restoration method, including the use of a pin retention support for restorations, when using the LuxaCore Z-Dual nanocomposite material on the quality of the marginal fit of fillings.
Thus, the long-term results of our study showed that the number of complications in non-vital teeth with defects of the coronal part III (IROPZ 0.6-0.7) and IV (IROPZ 0.7-0.8) classes according to Peroz was 12 less .8% and 27.5%, respectively ( p
<0.05), when using fiberglass composite-reinforced pins as a retentive support for direct restorations made of dual-curing nanocomposite material, than in the case of restoring the coronal part of the tooth only with dual-curing nanocomposite material.
In the presence of a defect in the coronal part of the tooth of class II according to Peroz (IROPD 0.5-0.6), when comparing the two above restoration methods, we did not find any significant differences ( p
> 0.05).