Simultaneous instrumentation and permanent obturation of the root canals is performed in the absence of contraindications to filling. If there is pain, swelling, abscesses, exudate and an unpleasant odor, drug treatment must be carried out before closing the cavity. It includes exposing the treatment area to medications that eliminate existing problems and prepare the canals for the installation of a permanent filling.
What is a root canal?
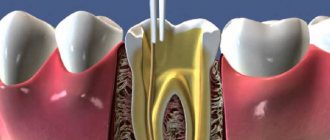
Each tooth, except for enamel and dentin, has an internal space - a pulp chamber, communicating with thin cavities running along the entire length of the roots of the teeth - root canals. Different dental groups have different numbers of roots, and, accordingly, canals. The front group has 1 channel, the side ones - from 2 to 4.
Narrow, winding, thin tubes with many branches - this is how to characterize the root canals of teeth. The entrance to them is located at the apex of the tooth root, it is called the apical foramen. Through it, through each root canal, passes neurovascular tissue, which is responsible for the blood supply and innervation of the tooth.
Endodontic treatment is a procedure for removing infected, inflamed or dead neurovascular tissue, followed by cleaning and disinfection of the resulting space, and completely sealing the dental canals.
Modern endodontic treatment
The main cause of inflammation of the pulp (neurovascular bundle) and periodontitis (surrounding tissue of the apex of the tooth root) is microorganisms and their toxins, which can enter from the carious lesion into the tooth cavity (with pulpitis) and from the inflamed or infected pulp into the periodontium (with apical periodontitis). ).
Treatment of complicated caries – pulpitis and periodontitis – remains an important and pressing problem of modern dentistry. This is confirmed by the data that visits among the population of the Republic of Belarus for pulpitis and periodontitis account for more than 40% of all visits to the dentist. It should also be emphasized that, unfortunately, apical periodontitis is one of the main reasons for tooth extraction. In addition, it can lead to a decrease in the immunological reactivity of the body and can serve as a background for the development of pathology of internal organs.
The main goal of treatment of pulpitis and periodontitis is, as a rule, reduced to the removal of pathologically altered pulp, infected hard tissues (dentin) and hermetically sealing the lumens of the root canals, isolating them from the oral cavity, which prevents the spread of the process to the surrounding tissues of the tooth root. Successful treatment is facilitated by the use of new technologies and equipment, which improves the quality of diagnosis and treatment, reduces the time of medical manipulation, and prevents complications. The use of 3D computed tomography allows detailed diagnosis and treatment planning.
The main stages of modern endodontic treatment
- Diagnostics.
- Anesthesia.
- Isolation of the surgical field.
- Preparation.
- Pulp removal.
- Determination of the length of the root canal.
- Mechanical (instrumental) and medicinal treatment of root canals.
- Filling root canals in three-dimensional space.
- Assessment of the quality of treatment in the immediate and long term.
An endodontic diagnosis is made on the basis of patient complaints, medical history, clinical examination, X-ray examination and data from clinical tests (zoning, percussion, palpation, temperature test, EDI)
Before instrumental (mechanical) treatment of the root canal, it is necessary to completely remove carious dentin, thereby preventing bacteria from entering the root canal. Removal of coronal pulp is carried out using an excavator or a spherical bur. After this, I determine the position of the root canal mouths using an endodontic probe and extirpate (remove) the pulp in the root canals.
The quality of filling depends on determining the length of the root canal. A well-sealed root canal involves filling it with filling material tightly to the apex of the root. If the tooth is not filled to the top, then microorganisms begin to multiply in the lumen of the unsealed part. Over time, the infection spreads beyond the root apex, which leads to the destruction of bone tissue at the root apex and the development of a focus of inflammation there. Length determination in modern dentistry is carried out using a special electronic device - an apex locator. The apex of the tooth root has a certain electrical resistance, which is measured using a pair of electrodes usually connected to the lip and endodontic file. The principle is simple, as soon as the file reaches the root tip, the resistance decreases sharply. The device signals this event with a sound or light signal, or with digital readings on the display. The final control of the length of the root canals is carried out using an x-ray.
Purposes of mechanical and medicinal treatment:
- Removal of infected pulp or its decay.
- Removal of infected dentin from the walls of the root canal.
- Removal or suppression of the vital activity of microorganisms in the canal or its branches.
- Giving optimal shape for obturation.
There are two types of root canal treatment: using hand instruments; using a special endodontic tip in which endodontic instruments are fixed. When instruments vibrate and rotate in the root canal, their sharp edges remove dentine chips from the walls of the canal and expand it.
The use of medicinal treatment of root canals allows you to: destroy microorganisms, dissolve tissue decay products and pulp residues, mechanically wash infected chips from the root canal and treat places that are inaccessible for treatment with an instrument (deltoid branches at the apex).
Today, solutions of sodium hypochloride 0.5-5.5% and chlorhexidine gluconate 0.2-2.0% are most often used for irrigation (washing) of root canals. Ultrasonic tips are widely used to activate irrigation. After mechanical treatment and irrigation of the root canals, the number of microorganisms in them sharply decreases (by orders of magnitude), however, some of them still remain (especially in places inaccessible to instruments). Currently, for the final and most thorough antiseptic treatment, temporary filling of root canals with calcium hydroxide is used, and ozone therapy is also used, which allows, with a single impact on the microflora of the root canal, to significantly reduce the level of contamination.
Root canal filling has the following purposes:
A) isolate the root canal and periapical tissues from the entry of microorganisms from the oral cavity.
B) isolate the root canal from the ingress of liquid from the surrounding tissues, which can serve as a breeding ground for microorganisms.
C) isolate remaining microorganisms from food sources.
Materials used to fill the root canal are divided into three groups:
- Sealants (sealers).
- Filling pastes.
- Hard materials (pins).
Currently, the low effectiveness of using sealants and pastes in their pure form for filling canals has been proven, and therefore they are used only in combination with solid materials (pins) to fill root canals. The use of solid materials for filling root canals (pins) allows you to fill the root canal in three-dimensional space (length and diameter). Among solid materials, gutta-percha points are the most commonly used. Gutta-percha is a hard but elastic material that has remarkable characteristics: low toxicity, biocompatibility, the ability to fill the root canal as much as possible when heated, and ease of removal from the root canal if necessary.
methods of root canal filling are distinguished :
- Compaction of cold gutta-percha in the root canal (lateral condensation technique and its variations).
- Consolidation of gutta-percha heated in the root canal (vertical condensation).
- Injection of preheated gutta-percha into the canal:
— on hard media (“Thermafil”); on gutta-percha carrier (“Guttakor”)
— from a syringe (“Ottura”, “Ultrafil”);
— thermomechanical condensation (“Quickfil”).
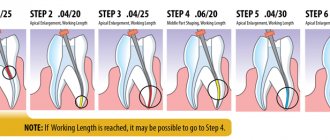
Currently, one of the most popular techniques is lateral condensation. The following stages are distinguished:
- Selection of the main gutta-percha point. The pin is selected depending on how much the root canal was expanded during mechanical treatment.
- Filling the root canal with sealer, after which the main pin is inserted.
- Condensation (compaction) of the gutta-percha pin using a special tool - a spreader. The compaction process consists of performing rotational-translational movements with a spreader, with the help of which gutta-percha is pushed towards the walls of the root canal and space is freed up for the introduction of new gutta-percha pins.
- Excess gutta-percha is removed at the level of the root canal orifice with a hot instrument. And vertical condensation is carried out with a small plugger or plugger.
For more complete isolation of all branches of the root canal, a method of vertical condensation of gutta-percha was proposed. Its essence is as follows.
- The main gutta-percha pin is inserted into the root canal and shortened by 2 mm from the working length. The pluggers are adjusted so that one goes through the coronal part, the other goes through the middle part, and the last one does not reach 2 mm to the working length.
- The pin is inserted into the root canal and heated, the pin is compacted with a plugger in the vertical direction and the gutta-percha is partially removed. The cycle is repeated until the last plugger is within 2 mm of the working length.
- Standard blanks 2-3 mm long are inserted into the root canal, heated and compacted with pluggers. Gutta-percha is not removed. Filling is carried out to the mouth of the root canal.
The technique makes it possible to obstruct the lateral canaliculi and branches at the apex, however, it is technically difficult. In order to simplify, methods have been proposed for introducing preheated gutta-percha into the root canal.
Injection administration (“Ottura”).
Stages of the method:
- The root canal is dried, and gutta-percha is heated in a special apparatus to a temperature of 185-200°C. The needle is adjusted so that it reaches the border of the middle and apical third of the root canal and is not blocked by the walls of the root canal. The plugger is adjusted so that it freely reaches the apical part at a distance of 2 mm less than the working one.
- A sealer is applied to the walls of the root canal.
- Heated gutta-percha is introduced into the root canal through a needle (without pressure towards the apex) and fills the apical part of the canal (2-5 seconds), after which it begins to push the instrument upward.
- Gradually, withdrawing the needle, fill the root canal to the mouth.
- The gutta-percha is compacted in the apical direction using a plugger. Gutta-percha is added to the root canal as needed.
To simplify the method, 2 types of gutta-percha were proposed: high fluidity and easily fluid gutta-percha.
Ultrafil technique
also applies to injection and has some differences from “Obtura”:
- gutta-percha blanks of 3 degrees of viscosity are used - high, medium and low;
- gutta-percha is injected from a special syringe, which automatically dispenses its amount with each press.
Injection methods make it possible to densely fill root canals and branches, however, there is a high risk of material being removed beyond the apical foramen and burns to periodontal tissues.
Thermafil system
allows you to introduce heated gutta-percha on a rigid base (metal or plastic), or on a gutta-percha carrier (“Guttacor”), which bends well and presses the softened gutta-percha into the branches of the root canal.
Stages of the method:
- A metal blank is placed into the root canal, which follows the shape of the carrier with gutta-percha. It should freely enter the root canal to its working length.
- A sealer is applied to the walls of the root canal.
- A pin coated with gutta-percha is placed in a special oven and heated until the gutta-percha gives a fluid consistency.
- The pin is inserted into the root canal, not reaching 1-2 mm to the working length (the length is marked with a stopper).
- The pin is cut off at a level of 1 mm from the mouth using a bur. While removing excess, pressure is maintained in the apical direction so as not to displace the pin.
Thermo-mechanical compaction of gutta-percha in the root canal Method steps:
- The main pin is fitted in the root canal and inserted with sealer to the working length.
- A rotating condenser is inserted into the root canal to a length > 4 mm less than the working one or until resistance occurs, and then carefully withdrawn without stopping rotation (3500-4000 rpm).
- Gutta-percha is compacted vertically with a plugger.
Results of endodontic treatment in the long term after treatment (after 12 months):
- The patient has no symptoms.
- There should be no signs of inflammation or fistula in the tooth area.
- Radiologically, the periapical tissues should be normal (if there were no radiological signs of pathology before treatment) or show signs of restoration of destruction (if they were observed before treatment).
Diseases that require endodontic therapy
Treatment of tooth canals is performed only if there are strict indications, since as a result of the intervention, the tooth is deprived of the vessels and nerve endings that feed it, which makes the dental tissues less durable and more susceptible to destruction. Indications for intervention include inflammation and infections accompanying caries or traumatic tooth damage:
- Pulpitis is inflammation of the pulp (neurovascular tissue) - soft, fibrous tissue, including blood and lymphatic vessels, nerve endings and connective tissue.
- Periodontitis is inflammation of the tooth root and surrounding tissues (periodontal tissue).
These diseases are usually accompanied by the following symptoms:
- Acute, throbbing or aching pain in the tooth, increasing at night or intensifying with load on the tooth.
- Swelling, discoloration of the gums, formation of ulcers and fistulas on it.
- Putrid odor from the mouth.
In some cases, there are no pronounced symptoms and the development of pulp necrosis is detected only during a doctor’s examination. Only a specialist can accurately determine whether endodontic treatment will solve the problem and select the most effective therapeutic regimen.
Methods of treatment of dental canals
Not so long ago, arsenic paste was used for endodontic treatment. The dentist opened the dental chamber, put the paste into it and, after the pulp died, removed it from the tooth. Next, the tooth was filled and considered cured. The resorcinol-formalin method was also widely used - a resorcinol-formalin mixture placed in the cavity slowly hardened, stopping the disintegration of the partially removed pulp.
But such technologies have significant disadvantages:
- Arsenic and formalin saturated with resorcinol are very dangerous, toxic substances that can accumulate in various organs.
- These substances cannot always kill the nerve completely, which contributes to severe pain when trying to extract the pulp.
- Infected neurovascular tissues that are not completely removed become a source of repeated inflammation.
These methods were used because there were no sufficiently strong anesthetics that would allow removal of the affected pulp painlessly. Today they are completely irrelevant - modern dentistry treats tooth canals using a completely different technology.
Modern methods of dental canal treatment
There are two main methods of treating tooth root canals:
- Therapeutic (biological) in which the entire pulp or part of it is preserved. Manipulations can be carried out directly - the dentist puts a medicinal product into the dental cavity, separates the pulp chamber with an insulating gasket and installs a temporary filling. Or drugs can be delivered through the dentin, using antibiotic dressings, etc. Such drug therapy is effective only at the initial stage of inflammation.
- Surgical (pulp extirpation) - removal of all neurovascular tissue, cleaning, disinfection and sealing of dental cavities. Root canals are treated in one of the following ways: classic filling of tooth canals - filling the voids with filling material.
- Vertical condensation by injection of thermoplasticized gutta-percha.
- filling using thermophiles - hot gutta-percha on a carrier.
In some cases, endodontic treatment requires resection of the root apex - in the presence of granuloma, fibroma, cyst, perforation and other problems near the root apex.
Medicines for the treatment of root canals in children
Today, pediatric dentists have a huge selection of medications for treating intracanal cavities at their disposal. The products most actively used by leading dental clinics in Moscow are represented by the following categories and types:
- antibiotics (Metronidazole, Gramicidin, Polymyxin M);
- bactericidal compounds (Chlorhexidine, Sodium hypochloride, iodine, Iodinol, Lugol's solution, hydrogen peroxide, 30% urea solution);
- anti-inflammatory (Dicamphen, Iodex, Camphorphen, Guaifen, Pulposeptin, Indextrol);
- calcium hydroxide (powder, solution or paste composition) and hydroxyapatites (Hydroxyapol, Kergap, Ostim-100);
- MTA preparations (mineral trioxide aggregate) – Biodentin, Restapex, Trioxident and others.
When choosing the optimal therapeutic drug, it is important not only to correctly assess the condition of the root canals and the general well-being of the patient, but also the nature of the problem. You should also take into account the quality of the substance used: biocompatibility, non-toxicity, moisture tolerance, hypoallergenicity, effectiveness, etc. Upon completion of medication treatment, it is imperative to re-examine the canals and perform their permanent obturation.
Stages of treatment
- Diagnostics
If damage to the dental canal is suspected and in order to detect a pathological focus, an X-ray examination (orthopantomogram, CT) or a study of the patient’s existing images is performed. Based on the examination results, the endodontist selects the appropriate treatment method.
- Pulpectomy
After anesthesia, the dentist opens the tooth, removes all damaged and necrotic tissue, gives the canal the required shape and rinses it with an antiseptic.
- Canal filling
Open channels are hermetically filled with filling material. For this purpose, plastic (gutta-percha, paste), hardening (cement group) and hard materials (pin structures) are used. The most progressive method is filling the canals with hot gutta-percha.
- Restoration of the crown part of the tooth
The correct anatomical shape of the tooth is restored using direct (filling) or indirect (crown, inlay) restoration.
Obturation with medicinal materials
Drug treatment of dental canals can be carried out either by direct treatment or by installing a temporary filling. In the second case, the dentist fills the intradental cavity with special non-hardening materials of plastic consistency, which have certain healing properties. The period of temporary canal filling can range from 1-5 days to several months. The main preparation is pastes. Also in pediatric dentistry, liquid products are actively used, which are used in turundas and dressings immediately after instrumental opening.
Temporary obturation of canals with therapeutic fillings allows you to solve the following problems:
- antiseptic treatment and cleaning of canals and dentinal tubules;
- neutralization of toxic substances and suspension of resorption;
- anti-inflammatory effect on the site of periodontitis development;
- stimulation of natural regeneration of soft and bone tissues;
- isolation of the open cavity from the environment if it is impossible to complete treatment.
Features of root canal treatment under a microscope
Modern dentistry cannot be imagined without the use of innovations that take root canal treatment to a new level. One of the most advanced methods of root canal treatment is the use of a dental microscope. Powerful optics allow you to increase your view by 32 times, given that the diameter of the channel is usually no more than 1 mm, it is simply impossible to process it efficiently without the help of optics.
Advantages of dental treatment under a microscope:
- The endodontist sees in detail the mouths of the canals, the features of their structure, each branch, depth and direction. This is especially important if the tooth canal has a complex, convoluted shape.
- The microscope makes it possible to remove only diseased and dead tissues without damaging healthy ones.
- Thanks to the targeted effect on the tissue, the best result of the intervention is ensured, eliminating the likelihood of perforations, as well as other problems and complications.
The use of a dental microscope allows the dentist to successfully solve even the most complex clinical problem.
Drug treatment
- hydrogen peroxide
Preparations for expanding the root canal.
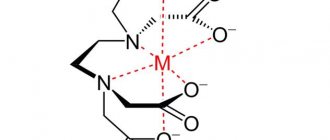
Root canal enlargement preparations generally contain ethylene diamine tetraacetic acid (EDTA), which dissolves the inorganic components of dentin. Dentin calcium combines with EDTA to form a stable chelate. Also, such preparations often include carbamide peroxide and distilled water.
Endolubricants can be produced in either liquid or gel form. Gels are more convenient, as they “lubricate” the canal walls and prevent jamming of the endodontic instrument.
Preparations for antiseptic treatment of the root canal.
Hydrogen peroxide and chlorine-containing products.
- Hydrogen peroxide. A 3% hydrogen peroxide solution is used to flush the canal. Upon contact with tooth tissue, peroxide dissociates with the release of atomic oxygen (bubbles). This has an antiseptic effect (on anaerobic bacteria) and promotes mechanical cleansing of the canal. Has a hemostatic effect.
- Chlorine-containing products. (0.2-1% chlorhexidine, 3-5% sodium hypochlorite, 2% chloramine). Dissolves necrotic tissue, has a bactericidal effect on Gr+ and Gr- bacteria, fungi and viruses.
- sodium hypochlorite – has a pronounced antiseptic effect due to the formation of chlorine gas. Has the ability to penetrate dentinal tubules. Dissolves remaining organic matter in the canal. ATTENTION – do not move beyond the apex.
In case of contact with periapical tissues – sharp pain, profuse bleeding, development of edema (aseptic inflammation)
Currently, the root canal is treated according to the following scheme: sodium hypochlorite - after each change of instrument and after the end of mechanical treatment of the canal, then - hydrogen peroxide, then - distilled water.
Iodine preparations, nitrofurans.
- Iodine preparations –
- 1% iodinol solution (blue) - a compound of iodine with polyvinyl alcohol, has a strong bactericidal and fungicidal effect, stimulates the phagocytic activity of leukocytes, accelerates tissue regeneration. It is an indicator upon contact with tissue decay products, microbes, purulent discharge - it loses its dark blue color and becomes white.
If, when turunda with iodinol is introduced into the root canal, it retains its color, the root canal is clean. Iodine preparations can be used as an antidote to arsenic in acute arsenic periodontitis. A cotton swab or paper point soaked in one of the iodine preparations (5% unithiol solution, 1% iodinol solution, 3–5% iodine tincture) should be inserted into the root canal and left in it for 1–2 days.
ATTENTION! – before using iodine preparations, it is necessary to find out whether the patient is allergic to iodine.
2. Nitrofurans (0.5% furatsilin, 0.1-0.15% furadokin, fursalidone) - These drugs have a strong bactericidal effect, including on those microorganisms that are resistant to other medications. This is due to the influence of nitrofurans on the enzymes of microbial cells. In addition, nitrofurans enhance the phagocytic activity of leukocytes and have a pronounced anti-exudative effect.
Quaternary ammonium compounds
0.1% decamine solution. It has a bactericidal effect on spore-forming microorganisms and yeast-like fungi.
Dimexide, dimethyl sulfoxide
It has antiseptic, anti-inflammatory, analgesic, bacteriostatic, fungicidal effects.
Proteolytic enzymes (trypsin, chymotrypsin, lysozyme):
– selectively break down necrotic masses;
– thins exudates, viscous secretions, blood clots;
– accelerate the outflow of exudate from the source of inflammation without causing harm to living periodontal tissues;
– stimulate phagocytosis;
– destroy bacterial toxins;
– have anti-inflammatory and anti-edematous effects;
– enhance the effect of antibiotics and other medications on the microflora of the root canal.
Widely used for washing root canals in the treatment of acute and chronic periodontitis.
Enzymes can be used either alone or in combination with antibiotics and sulfonamides under a bandage that is left in the root canals for the period between visits, but not more than 1–2 days.
It is important to know
that when treating the root canal with proteolytic enzymes,
you cannot
simultaneously use other antiseptics, alcohol and ether, which inactivate both enzymes and antibiotics.
Methods of medicinal treatment of root canals.
- on Turunda:
A cotton turunda is wrapped around the endodontic instrument, moistened with an antiseptic, and inserted into the root canal.
- Using a paper pin
. A dry paper pin is inserted into the root canal, after which an antiseptic is dripped onto it (with tweezers), then the pin is removed from the canal.
- Using an endodontic syringe.
Special needles for the endodontic syringe are used (hole on the side) so that the antiseptic is not discharged into the periodontium.
RULES FOR WASHING THE CHANNEL FROM A SYRINGE:
- Always use only endodontic needles
- never push the needle deeper than ½ channel
- never inject antiseptic under pressure
- make sure that the needle does not “jam” in the canal
— With sound or ultrasonic treatment
– antiseptic is used as a coolant. It is advisable not to use strong antiseptics, as there is a risk of their penetration into the periodontium.
Preparations for antiseptic dressings.
Phenol derivatives.
Antiseptic dressings are medications that are placed in the tooth cavity, hermetically sealed with temporary filling material and left between visits. Used for:
- destruction or reduction of bacterial flora remaining in the root canal after its instrumental and medicinal treatment, especially with destructive changes in periodontal tissues;
- preventing or reducing pain;
- reducing the inflammatory process in the periodontium
- stimulating bone tissue regeneration during destructive processes in the periodontium.
Application rules: the root canals are treated mechanically and medicinally, dried, a cotton swab is moistened with an antiseptic, wrung out well, and placed on the bottom of the tooth cavity.
Phenol derivatives have a strong bactericidal effect;
- combine well with other drugs (glucocorticoids, antibiotics, etc.)
- When used correctly, there are no side effects from the periodontium.
- Phenol derivatives:
1) Eugenol – essential oil.
Eugenol is a chemical derivative of clove oil, related to phenol.
It has a mild antiseptic and pronounced analgesic effect. At the same time, eugenol has an irritating effect on living periodontal tissue. Used as a therapeutic dressing, which is left in the root canal for 72 hours. During this period, the released antiseptic vapors provide the greatest bactericidal effect.
2) Camphorophenol
It is an oily liquid consisting of 5 parts camphor, 3 parts phenol and 2 parts liquid petroleum jelly.
Has a weak disinfectant effect. Used as an antiseptic dressing. Before inserting into the tooth cavity, a cotton ball moistened with camphorophenol is squeezed out well so that excess drug does not penetrate into the periapical tissues.
It can be used in conjunction with arsenic paste, covering it with a wrung-out swab on top, which promotes better diffusion of arsenic into the tissue.
An analogue of camphorophenol is “Cresoden”, produced domestically, which contains camphor and parachlorophenol.
Contains a corticosteroid hormone - declamethasone and strong bactericidal substances - parachlorophenol, thymol.
It has a pronounced anti-inflammatory and antiallergic effect. Used for treating root canals before filling in the treatment of pulpitis and periodontitis.
Shown
as an antiseptic dressing for 2–3 days:
- in the treatment of difficult-to-pass canals;
- impossibility of complete pulp excision;
- with a pronounced inflammatory reaction of periodontal tissues.
3) Preparations "Rockle"
The composition includes phenol, formaldehyde, guaiacol, dexamethasone.
They differ from each other in the amount of formalin included in each drug
Aldehydes and antibiotics.
Aldehydes.
1) Formaldehyde
– the most popular antiseptic in domestic endodontics. Formalin is the main substance of the resorcinol-formalin method.
Formaldehyde, penetrating into the dentinal tubules of the root, converts the albumins located there into insoluble and aseptic mixtures, resulting in deep sterilization of the dentinal tubules.
2) “Abscess remedy liquid”
(PD Germany). The drug contains 40% formaldehyde, creosote, thymol and alcohol, and has a strong antiseptic and bactericidal effect.
3. Antibiotics.
Of greatest interest for endodontics are antibiotics with a pronounced local antimicrobial effect (chloramphenicol, erythromycin, gentamicin, neomycin), as well as their combination with corticosteroids and enzymes.
However, the widespread use of antibiotics contributes to the emergence of new forms of microorganisms that are resistant to antibiotics. When treating periodontitis, it is recommended to use a combination of two or more antibiotics and only taking into account the sensitivity of the microflora isolated from the root canals before starting treatment
.
Hemostatic agents.
- 3% hydrogen peroxide solution (H 2 O 2 )
- "Katalyugem" (Moscow)
Stops bleeding due to the content of aluminum chloride, and also has powerful antiseptic properties due to the presence of catamine AB. The drug is a clear liquid that does not irritate the tissues in contact with it.
To achieve hemostasis, it is introduced into the root canal on a turunda or paper pin for 40 seconds - 1 minute. If bleeding is not stopped completely, repeat the procedure.
- Racestyptine
It has a hemostatic effect due to the presence of aluminum chloride in it. Used to stop apical bleeding and bleeding from the perforation area.
- Solutio
Adrenalini hydrochloridi 0.1%
Stops bleeding due to local vasoconstrictor action. A turunda or a paper pin moistened with an adrenaline solution is inserted into the root canal.
6
Recommendations after treatment
Endodontic treatment demonstrates high success rates. After the intervention, you must adhere to the following recommendations:
- Avoid too hot, spicy, or cold foods for several days (while teeth sensitivity remains).
- Maintain good hygiene – brush your teeth twice a day, use dental floss and an irrigator.
- Do not chew anything hard (do not chew nuts, candies, etc.), as this may result in damage to the root canals and tooth destruction.
- Undergo medical examinations with a dentist and hygienist (at least 2 times a year).
Immediately after the procedure, tooth sensitivity increases greatly. This is explained by the reaction of the tissues to the filling material. The discomfort will disappear in a few days.
Expert opinion
Lyubov Ivanovna Kopylova
dentist-therapist
Experience: more than 10 years
If you have the opportunity to go to a dental clinic equipped with an electron microscope, take advantage of it! Even the most experienced dentist works with canals without a microscope by touch. This means that there is a risk of underfilling or, on the contrary, excessive deepening into the canal, leading to perforation. The use of a microscope, when the working field is clearly visualized and the doctor efficiently cleans and seals even the thinnest and most curved canals, will allow this situation to develop.
Cost of root canal treatment in Moscow
The price of endodontic treatment depends on the number of root canals of the diseased tooth, the method used, complexity (including re-treatment) and volume of intervention, type of filling, etc. Processing 1 channel requires less work than 2 or 3, which affects the cost.
| Group of teeth | Cost of pulpitis treatment | Cost of periodontitis treatment |
| 1 canal tooth | 6500 rub. | 8500 rub. |
| 2 channel tooth | 7500 rub. | 9500 rub. |
| 3-channel tooth or more | from 8500 rub. | from 10,500 to 12,000 rub. |
The price includes the entire list of procedures performed for the treatment of dental canals. When using a dental microscope and laser equipment in complex therapy, the cost of treatment increases.
Results of a study of gels for chemical expansion of dental root canals
O. P. Krasnikova Ph.D., assistant at the Department of Clinical and Pediatric Dentistry of VSMA
E. A. Alferova Candidate of Medical Sciences, Assistant of the Department of Clinical and Pediatric Dentistry of VSMA
E. V. Vusataya Candidate of Medical Sciences, Assistant of the Department of Clinical and Pediatric Dentistry of VSMA
S. Yu. Khavantsev Assistant, Department of Clinical and Pediatric Dentistry, VSMA
A. V. Sushchenko Doctor of Medical Sciences, Professor, Head of the Department of Clinical and Pediatric Dentistry of VSMA
Today, endodontics has extensive information about the structure of the root canal system. It is known that the overwhelming majority of root canals have an irregular shape, different diameters in the buccolingual and mesiodistal directions, numerous lateral canals, anastomoses and isthmuses, the presence of a delta in the apical part, the formation of not one, but several apical foramina, etc.
In this regard, it becomes obvious that such a complex system is not possible to clean only mechanically [4]. It is known that one of the most important stages of endodontic treatment, which has a significant impact on its prognosis, is mechanical and medicinal treatment of the root canal system [1, 2, 5].
To facilitate the passage and expansion of narrow and obliterated root canals during instrumental treatment, complexons or so-called chelates with an affinity for alkaline earth metals are used. Expansion of the canal using chelates is based on their ability to form complex compounds with dentine calcium, as a result of which the latter goes into solution.
As a result of this reaction, the walls of the root canal are decalcified and softened, which facilitates the process of instrumental treatment of the root canal. Complexons are non-toxic, easy to use, do not require special storage conditions, and remain active for a long period of time [3].
The pre-marked instrument is lubricated with gel, inserted into the canal, and mechanical processing is carried out with the prepared file. Alternately, you should irrigate the root canal with a solution of sodium hypochlorite and perform mechanical treatment of the canal with a file lubricated with gel. During irrigation with sodium hypochlorite, foam will form, which will help remove the contents of the canal.
You cannot leave the gel in the canal until the next visit. Finally, it is necessary to thoroughly rinse with water and dry the canal with a liquid for drying and degreasing the root canals, after which you can begin filling.
Today, the dental market offers a wide range of EDTA-based products, which are produced in the form of gels, solutions, and liquids. We conducted a comparative analysis of agents for chemical expansion of root canals RC-prep (USA), Canal + (Septodont), Edetal (Omega) and Dilaton+ (Celite). In the experiment, such properties of the preparations as fluidity, the pH value of the gel, the ability to remove dentin particles, the foaming effect when adding sodium hypochlorite, etc. were studied (Table No. 1).
Table No. 1. Comparative analysis of gels for chemical expansion of root canals
| Indicators | Rc—prep(USA) | Canal+ (“Septodont”) | "Edetal" ("Omega") | "Dilaton+" ("Celite") |
| Package | Syringe without rubber piston, plastic bag, label, 1 pc., cannula (curved), no instructions | Syringe without rubber piston, box, label, instructions, 5 cannulas | Syringe with rubber piston, label, instructions, box | Syringe with rubber piston, label, instructions, box |
| Weight | 9 g | 5 g | 5 ml | 5 g |
| Appearance, consistency | Homogeneous viscous gel, opaque, white, well lubricates endodontic instruments | Homogeneous viscous gel, opaque, white, well lubricates endodontic instruments | Homogeneous thick gel, opaque, white | Homogeneous viscous gel, opaque, white, well lubricates endodontic instruments |
| Fluidity of 0.1 g gel, mm at a load of 2.5 kg | 32—34 | 28—30 | 25—26 | 34—35 |
| pH value of the gel | 6 | 6 | 6 | 6 |
| Floating agent content (ability to remove dentin particles), % | 11,5 | 5 | 5 | 5 |
| Foaming effect when adding sodium hypochlorite | Active foaming | Moderate foaming | Moderate foaming | Moderate foaming |
| Amount of main substance Trilon B, wt % | 17,5 | 15,5 | 14,5 | 15 |
| Water washability | + | + | + | + |
| Dissolution in water | Dissolves slowly, presence of undissolved sediment, cloudy solution | Dissolves quickly, presence of undissolved sediment, transparent solution | Dissolves slowly, the solution is transparent, there is no sediment | Dissolves quickly, the solution is transparent, there is no sediment |
All presented drugs demonstrated similar values. The study found that the highest content of floating agents that promote the removal of dentin particles was found in RC-prep (USA). In addition, a comparative study of the clinical effectiveness of the use of drugs RC-prep (USA), Canal + (Septodont), Edetal (Omega) and Dilaton+ (Celite) was conducted. Chemical expansion of 20 root canals of teeth in 15 patients was performed (5 canals per preparation).
To obtain comparable results, chemical expansion of the canals was carried out only on teeth of the lower jaw that had not previously been treated endodontically. The method of administration of the drugs was identical. Each of them was introduced into the root canal using a hand-held endodontic instrument, and mechanical expansion of the canal immediately began.
The procedure was repeated 3-5 times. At the end of the procedure, the tooth cavity was washed with water. The effectiveness of the intervention was assessed by the time spent on expanding the canal (Table No. 2).
Table No. 2.
| A drug | Average time spent on one root canal (min.) |
| RC-prep(USA) | 2,6 |
| "Dilaton+" ("Celite") | 3,4 |
| Canal+ (Septodont) | 4 |
| "Edetal" ("Omega") | 4,2 |
When using RC-prep (USA), all root canals were completed to the apical foramen within 1-5 minutes from the start of expansion, an average of 2.6 minutes. When using Canal + (Septodont), all root canals were completed to the apical foramen within 1-8 minutes from the start of expansion, an average of 4 minutes.
When using "Edetal" ("Omega"), all root canals were passed to the apical foramen within 1-9 minutes from the start of expansion, an average of 4.2 minutes. The time spent using the drug “Dilaton +” (“Celite”) ranged from 1 to 7 minutes, with an average of 3.4 minutes. It should be noted that when using all drugs, no side effects were observed in patients; no irritation of periapical tissues was observed in the immediate period after treatment (1-7 days).
Thus, our study indicates a higher efficiency of the drug RC-prep (USA), and, apparently, it should be given preference when choosing a gel for chemical expansion of the root canal. However, the cost of drugs must also be taken into account - when analyzing price categories, domestic drugs undoubtedly win. Therefore, when choosing a particular drug, a practicing dentist must take into account all the parameters.
- Cohen S., Burns R. Endodontics: Trans. from English - St. Petersburg, 2000.
- Krammer I., Schlepper H. Guide to endodontics. User of endodontic instruments. Per. with him. - M., 1999. - 96 p.
- Makeeva I.M., Pimenov A.B. Smear layer of the root canal and its removal Endodontics today. - 2002. - T.2, - No. 1-2. — P. 5-10.
- Pimenov A. B. Areas of root canals inaccessible for instrumentation // Endodontics today. - 2003. - T. 3, - No. 1-2. — P. 23-25.
- Poltavsky V. P. Intracanal medicine: Modern methods. - M.: Medical Information Agency, 2007. - 88 p.
- Information materials, "VladMiVa", "Omega-Dent", "Raduga-R", Septodont.