Filling the root canals of teeth is an endodontic dental procedure, the purpose of which is to close their lumen. Its “scientific” name is “obturation.” The process uses special materials, including ethonium and two-component pastes, as well as gutta-percha. The former is especially preferred as it fills the canal evenly and can be easily removed if the need for re-treatment arises. Filling with its use is called “three-dimensional obturation of root canals.” If the patient has indications, the procedure is combined with pin fixation. The latter is used to further strengthen the tooth if it is severely damaged and to provide prosthetics.
Tooth root filling in Moscow can be done at the dental department of CELT. Our multidisciplinary clinic has been represented on the domestic market of paid medical services for almost three decades. In our dentistry, we see orthopedists, surgeons, endodontists and therapists, who have many years of experience in scientific and practical work. Treatment is carried out according to international standards with the conclusion of an official contract and provision of guarantees. You can find out its price by going to the “Services and Prices” tab in this section. We regularly update our price list, but to avoid misunderstandings, please check the numbers with our information line operator or during a consultation with your doctor.
Root canal obturation - RUB 1,500.
Canal filling using lateral condensation method - RUB 2,200.
Application of an intracanal pin—RUB 2,500.
Three-dimensional obturation of one root canal with thermoplasticized gutta-percha - 4,000 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a consultation with a dentist-therapist is 1,000
Make an appointment
Temporary and permanent obturation of root canals: what is it and why is it needed?
Filling the root canals of teeth is an endodontic dental procedure, the purpose of which is to close their lumen. Its “scientific” name is “obturation.” The process uses special materials, including ethonium and two-component pastes, as well as gutta-percha. The former is especially preferred as it fills the canal evenly and can be easily removed if the need for re-treatment arises. Filling with its use is called “three-dimensional obturation of root canals.” If the patient has indications, the procedure is combined with pin fixation. The latter is used to further strengthen the tooth if it is severely damaged and to provide prosthetics.
Tooth root filling in Moscow can be done at the dental department of CELT. Our multidisciplinary clinic has been represented on the domestic market of paid medical services for almost three decades. In our dentistry, we see orthopedists, surgeons, endodontists and therapists, who have many years of experience in scientific and practical work. Treatment is carried out according to international standards with the conclusion of an official contract and provision of guarantees. You can find out its price by going to the “Services and Prices” tab in this section. We regularly update our price list, but to avoid misunderstandings, please check the numbers with our information line operator or during a consultation with your doctor.
Causes of urinary tract obstruction
Narrowing of the urinary tract cavity can be observed in people of different age categories. But if in children obstruction is most often congenital, then in adults in most cases it occurs due to disorders of the urinary system. The cause of obstruction of the urinary tract may be a mechanical defect in patency caused by a tumor, kidney stones, blood clots, foreign bodies (with a prolonged stay of the catheter in the ureter). Also, swelling that appears as a result of an inflammatory process in the bladder or ureter can cause a narrowing of the lumen of the canal. Obturation itself is not a disease, but only a condition indicating the occurrence of pathology in the body. Regardless of the etiology of obstruction, it can lead to the development of renal failure.
Temporary and permanent obturation of root canals: what is it and why is it needed?
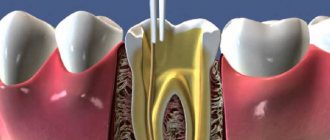
Filling the tooth canals is a mandatory stage of their treatment, the purpose of which is to stop the inflammation of periodontal and pulp tissues. It is carried out for such dental pathological conditions as caries, periodontitis and pulpitis: the latter are often complications of carious processes that did not receive timely treatment. In addition, endodontic manipulation may be required when re-treating canals or in the process of preparatory measures for prosthetics. They themselves are quite complex, and therefore require the endodontist to have not only the appropriate knowledge and skills, but also equipment - a dental microscope (in some cases), as well as professional tools.
This approach is relevant, since the procedure for permanent filling of tooth canals involves working with its internal structures. They are the ones who ensure its functionality and nourish it, prolonging its life. Failure to comply with technology and making mistakes can lead to serious complications and – often – the loss of the entire unit... But thanks to proper treatment, a tooth can be saved, sometimes in the most difficult cases. Before starting the procedure, the dentist removes the necrotic pulp from the canal and expands it in order to extract all fragments of the affected tissue. The next step is disinfection and drying, and only then sealing.
As for temporary obturation of root canals, it is also carried out after endodontic manipulations are completed. In the process, the dentist also fills the canals with a special composition, but not in order to close the gap, but in order to cure them and eliminate the possibility of complications. As a rule, the medicine is placed for several days or even months, excluding the penetration of pathogens. This approach is intended to:
- stop the inflammation of periodontal tissues;
- ensure high-quality disinfection of root canals and dentinal tubules;
- guaranteed to clean them by removing microfragments of pathological tissues from them;
- stimulate the regeneration of periodontal tissues and bone tissue of the alveolar process;
- isolate the root canal and the processes occurring in it, if permanent filling in one visit is not possible.
Most often, temporary filling of root canals is practiced during the period of manipulation to eliminate periodontitis. Depending on the situation, it can last more than one month and requires that medications be placed directly into the canals.
results
Initially, based on the results of trial instillations for 2-3 days, the optimal “artificial tear” preparation for each patient (based on subjective sensations) was selected. It was found that among low-viscosity preparations, preservative-free preparations of 0.1% hyaluronic acid were most preferable in patients with both mild and extremely severe forms of ocular surface xerosis. Among the gel preparations (for patients with severe and moderate forms of the disease) is a preservative-free gel based on 0.3% hyaluronic acid.
According to the results of an examination of all 85 patients (143 eyes) after 1 month of artificial tear instillation, drug therapy turned out to be effective and sufficient to compensate for the xerotic process in 31 (35.0%) patients (50 eyes). Therapeutic measures were continued for all of them.
The remaining 54 patients (93 eyes): 15 patients of group 1 (15 eyes) and 39 (78 eyes) of group 2 underwent obturation of the lacrimal ducts: the first stage was temporary, and then, if it was effective, permanent.
The results of temporary obturation of the lacrimal canaliculi are presented in table. 1.
Table 1. Some clinical and functional parameters of xerosis of the ocular surface 5 and 14 days after temporary obturation of the lacrimal canaliculi Note. *—differences compared to the initial values are statistically significant (p<0.05—0.001). In it, all patients are combined into the two pathogenetic groups already mentioned above, differentiated in turn by the severity of corneal-conjunctival xerosis.
From those given in table. 1 data shows that the positive dynamics of almost all controlled parameters of the xerotic process were noted on the 5th day after obturation, and by the 14th day of observation there was an ambiguous trend: in relation to objective signs of xerosis and the degree of staining of the ocular surface - to further improvement, and in in relation to subjective symptoms and the tear meniscus index - to deterioration, but not reaching the level of initial values.
The considered pattern was especially pronounced in patients with severe and extremely severe dry eye syndrome due to a combined violation of the stability of the tear film and tear production. Moreover, the duration of the clinical and functional effect of temporary obstruction of the lacrimal canaliculi in such patients corresponded to the duration of the induced disruption of lacrimal drainage (according to the results of a repeated color nasolacrimal test).
Based on the results of temporary obturation of the lacrimal canaliculi, its clinical effectiveness (according to the above criteria) was established in 48 (87.1%) (81 eyes) out of 54 patients.
Accordingly, all of them subsequently underwent permanent obturation of the lacrimal ducts with one of those mentioned in the table. 2 ways
Table 2. Structure of patients with dry eye syndrome with occlusion of the lacrimal canaliculi, performed in various ways and, in the absence of effect from these interventions (including repeated ones), ligation of the horizontal part of the lacrimal canaliculi.
As a result of observations of these patients, it was established that permanent obturation of the lacrimal ducts (performed by any of the methods listed above) complements the clinical effect achieved on the 14th day of temporary occlusion of the lacrimal ducts. At the same time, the positive effect of constant obturation of the lacrimal ducts tends to increase over time, especially in groups of patients with decreased tear production (including in combination with impaired tear film stability). It was manifested by a decrease in the severity of clinical signs of corneal-conjunctival xerosis and the degree of staining of the ocular surface with diagnostic dyes, an increase in the stability of the precorneal tear film, as well as consistently high tear meniscus index values.
In a comparative assessment of the effectiveness of various methods of permanent obturation of the lacrimal ducts (based on the results of long-term observation of patients for 2-4 years), differences were found only in connection with the “reliability” of their closure for tear outflow. Other parameters of the effectiveness of permanent obturation of the lacrimal ducts depended only on the pathogenesis and severity of the clinical course of corneal-conjunctival xerosis.
However, none of the methods she used turned out to be absolutely reliable. In particular, spontaneous restoration of the patency of obstructed tubules was observed in 28.2% of cases after closing the lacrimal openings with silicone occluders and in 25.0% of cases after covering the lacrimal papilla with a displaced conjunctival flap. Also, in 51.7% of cases, recanalization of the lacrimal ducts was noted after coagulation of the lacrimal openings and vertical sections of the lacrimal canaliculi, and in 60.0% - after covering the lacrimal papillae with a free flap of the bulbar conjunctiva.
At the same time, the restoration of the patency of the lacrimal ducts was naturally accompanied by a worsening of the clinical symptoms of xerosis of the epithelium of the ocular surface. In addition, as studies have shown, the full clinical effect of the procedure in question is observed only when both lacrimal canaliculi are obstructed. Recanalization of one of the two obstructed lacrimal canaliculi (including the upper one) is naturally accompanied by a worsening of the clinical course of corneal-conjunctival xerosis and a return of the functional indicators of the xerotic process to the original ones.
All 19 patients (31 eyes) with recanalization of the lacrimal ducts underwent repeated permanent obturation using one of the methods listed above, the results of which are presented in Table. 3.
Table 3. Comparative effectiveness of various methods of repeated permanent obturation of the lacrimal ducts in the complex treatment of 19 patients (31 eyes) with dry eye syndrome of various etiologies who underwent unsuccessful “permanent” intubation of the lacrimal ducts. It was established that repeated obturation of the lacrimal openings with silicone occluders was slightly more effective ( 44.4%) than the primary one, performed on the same eyes. The effectiveness of repeated conjunctival transplantation was 57.1% when using a free flap and 60.0% when using a displaced flap. Repeated diathermocoagulation of lacrimal openings (30.8%) turned out to be even less effective, especially in eyes after primary coagulation (28.6%). And only ligation of horizontal sections of the lacrimal canaliculi turned out to be the most reliable method of closing the lacrimal ducts in patients with dry eye syndrome.
The effectiveness of complex treatment of the examined patients with dry eye syndrome is summarized in Table. 4.
Table 4. Comparative effectiveness (in%) of the main methods of treating patients with various etiopathogenetic and clinical forms of dry eye syndrome Note. * - in the numerator - the number of eyes with a positive effect of the intervention, in the denominator - the total number of eyes; ** — the operation was performed only if the primary intervention was ineffective.
As can be seen from the data presented in it, as well as as clinical practice has shown, the most effective (but more traumatic) method of permanent closure of the lacrimal ducts was ligation of the lacrimal canaliculi (100.0%), and the most delicate was obturation of the lacrimal openings with silicone occluders. However, this method of permanent closure of the lacrimal ducts turned out to be the least reliable, mainly due to the occluder falling out at different times after the intervention.
Based on the results obtained, we have determined the sequence of repeated measures to obstruct the lacrimal ducts, implemented when the previous ones are ineffective.
Thus, if a silicone occluder of the lacrimal punctum is lost or dislocated, it is advisable to either repeat its implantation (effect 44.4%) or resort to conjunctival coating of the lacrimal papillae (50.0%). The operation of diathermocoagulation of the lacrimal opening and the vertical part of the lacrimal canaliculus, due to its relatively lower efficiency, does not deserve such widespread use as the interventions mentioned above.
The lack of effect of the conjunctival coating of the lacrimal papillae is a reason for ligation of the recanalized lacrimal canaliculus. Considering the complexity and traumatic nature of this operation, the indications for it can be limited by the ineffectiveness of the previously performed repeated obturation of the lacrimal openings with silicone occluders, as well as the conjunctival coating of the lacrimal papillae.
In general, obstruction of the lacrimal ducts in the complex of treatment measures carried out for patients with dry eye syndrome can significantly increase the effectiveness of conservative treatment of such patients and deserves wide clinical use.
Indications and contraindications for dental root canal filling
Indications
- Pulpitis that cannot be cured with conservative methods;
- The need for re-treatment of the canal after previously performed procedures;
- Preparatory measures for prosthetics using stump inlays or a pin;
- Preparation for installation of a crown or bridge, provided that extensive grinding of hard tooth tissues is required;
- Treatment of a fractured tooth, provided that its pulp has been injured and died.
Contraindications
- Serious damage to periodontal tissues, which does not allow saving the tooth;
- Identification of a cystic formation that cannot be cured;
- Identification of any neoplasms in the area of the tooth root;
- Longitudinal root fracture;
- Too branched and curved dental canals;
- Their obstruction due to the lack of lumen or filling material that cannot be removed;
- Perforation of the root canal wall.
The last 4 points are relative contraindications. Treatment can be carried out by an experienced specialist using a dental microscope.
Preparation
The preparatory process is carried out taking into account the chosen method of sealing the root canal. The use of specialized equipment requires the selection of the appropriate tool.
For example, when installing an apical pin, you should select the appropriate size and trim its tip by 0.5-1 mm. Appropriate pluggers and equipment are also prepared.
Preparation for obturation:
- The use of specialized equipment requires the selection of the appropriate tool
cleaning all tissues affected by caries and installing fillings on the holes (except for the endodontic entrance);
- therapeutic procedures to eliminate periodontal problems;
- restoration work with the walls and surfaces of the tooth;
- if there is excessive salivation, the patient is offered the drug atropine (the solution is used to rinse the mouth half an hour before the onset of obturation).
Next, the dentist moves on to the next stage, which directly concerns the endodontic entrance:
- use of anesthesia (infiltration/conduction);
- opening access to the root canal (includes preparation of a cavity affected by caries, removal of the arch of the dental pocket where the nerves are located);
- extraction of tooth connective tissue and necrotic formations;
- determination of the parameters of the root canal opening (X-ray);
- treatment of the canal opening with medications and instruments;
- relieving inflammation (if any).
Experts do not recommend endodontic treatment to be carried out in one visit. In difficult cases, the period may drag on for several weeks.
Materials used for filling tooth root canals
There are special requirements for materials used for obturation of root canals; in particular:
- Compatibility with body tissues, minimizing the risk of rejection;
- Minimizing the risk of developing an allergic reaction;
- The presence of antiseptic and anti-inflammatory properties;
- Ease of insertion into and removal from the root canal;
- Elimination of shrinkage after hardening inside the channel;
- The ability to initiate regeneration processes in periodontal tissues.
- The ability to fully fill even small voids;
- X-ray detectability.
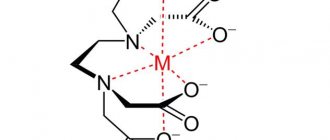
Obturators are usually divided into two groups:
- Fillers – pins made of metals, gutta-percha and fiberglass;
- Sealers are dental pastes and cements for fixing fillers.
Guttarpeche fillers are considered the most effective today, which give especially good results when combined with sealers. The latter are known for good adhesion to the walls of root canals and are able to provide reliable sealing if all conditions are met. In order for root canal filling to be carried out correctly, CELT dentists select materials for it on an individual basis, taking into account:
- The canal of which tooth (baby or permanent) requires obturation;
- Its branching, diameter, cross-country ability;
- The degree of destruction of the crown, the need to strengthen it;
- The patient's budget for the procedure.
Symptoms of urinary tract obstruction
Obstructions most often cause disturbances in the outflow of urine (even cessation) through the urinary tract, which is the cause of acute or chronic renal failure. Also, symptoms of a patency defect include pain, the intensity of which depends on the degree of development of obstruction. As the pathology progresses and homeostasis is disrupted, the pain becomes pronounced, with the manifestation of renal colic, and requires immediate medical intervention. If the obstruction develops slowly, renal function defects show little effect, pain may also be absent or quite mild or moderate and not cause much concern. At the same time, this condition also requires urgent assistance from doctors, since with chronic disruption of the outflow of urine, irreversible changes occur in the kidneys.
A favorable prognosis for obstruction of the urinary tract is possible only with its timely elimination and treatment of the diseases that caused it.
Complications that may develop after root canal obturation
Provided the procedure is carried out correctly, modern equipment and high-quality instruments are used, the risk of complications is minimized. Otherwise, the following complications are possible:
- Breaking off parts of the endodontic instrument and getting them stuck in the canal and, as a result, the presence of voids around them;
- Development of inflammatory processes and swelling in the cheek area on the side of the affected tooth;
- Perforation of the root canal wall;
- Allergic reaction to filling materials.
In all cases, the filling material will have to be removed, which is associated with a number of difficulties and the risk of complete tooth loss. After removing the fragments of endodontic instruments from the canal and cleaning it, the procedure will have to be repeated.
You just have to want it
For specialists in this case, the field of activity remains endodontic treatment in particularly complex root canal anatomy, as well as in particularly complex clinical situations, and for “particularly gifted” specialists - perhaps complex cases of root canal revision.
There is enough work for everyone. In any case, this would benefit “general-profile” therapeutic dentistry.
The article was provided by the magazine of the official publication of the Association of Dentists of Lower Saxony (Germany) NZB - Niedersächsisches Zahnärzteblatt (No. 6, 2011, pp. 31-34).
Translation by Inna Bichegkueva.
What is three-dimensional obturation? Its features and advantages
Gutta-percha obturation, also called three-dimensional, is considered the most effective method of filling root canals today. It ensures sealing of the entire root canal system, even if it is seriously branched. As a result, a reliable barrier appears between the dental cavity and periodontal tissues. The procedure solves several problems at once:
- Reliable sealing of the lumens of the dentinal tubules that extend into the lumen of the canal;
- Eliminating the risk of recurrent infection;
- Eliminating the risk of material resorption in the canal;
- Overlapping of the lumens of not only the main, but also the lateral and acesor canals;
- Creation of favorable biological conditions for tissue healing.
The advantages of this approach are obvious:
- Even more effective treatment of complicated caries;
- Painlessness, elimination of discomfort for the patient;
- Possibility of using a tab or pin;
- Guarantee that the canal will not become inflamed again.
It is worth noting that gutta-percha filling has been used in dentistry for several years now... But only today, thanks to a number of systems (“Gutta Core”, “ThermoFill”, others), it has become so effective, perfect and at the same time quite simple. As a rule, in the process of filling root canals, the endodontist faces a number of difficulties: from the individual characteristics of their anatomical structure to the development of inflammation of the tissues around the root.
Materials used for three-dimensional obturation
It is a special cross-linked thermosetting gutta-percha elastomer. It is made of gutta-percha in two different forms and combines its advantages. Its use makes the preparation stage for the pin as simple as possible, as well as removing the filling material from the canals, if the need arises. This material itself is quite strong, but under the influence of a certain temperature it becomes very plastic, which makes it easy to fill not only the central channel, but also its branches. Its composition is such that it will not dissolve under the influence of dentinal fluid. This also makes it quick and easy to remove.
Three-dimensional obturation algorithm
3D root canal filling systems include everything you need and do not require the use of special tools. At the same time, the endodontist who works with them must know their features well and follow technological processes. Procedure steps:
- Instrumental processing of the canal and its expansion to a value determined by the technology of working with a particular system (as a rule, the taper should be at least 6% for effective irrigation and obturation);
- Control of root canal measurements and selection of obturator size taking into account the taper involved in the process of instrument preparation. For control, the original verifier from the system with the appropriate size and taper is used;
- Introducing the sealer into the mouth or middle segment of the root canal, its uniform distribution during the process of introducing the obturator. It is important to avoid excess material as it may become trapped in the periapical tissues;
- Selection of an obturator, determination of its working length in accordance with the length of the root canal and heating in a special oven. Its slow introduction into the root canal and filling of all branches due to condensation at the mouth;
- Removing the media and handle and cutting the media directly above the mouth;
- Monitoring of the treatment performed by radiographic examination;
- Restoration of the crown part of the tooth by placing a filling or prosthesis.
Material and methods
The study material consisted of the results of examination and treatment of 85 patients (143 eyes) with dry eye syndrome of various etiologies and severity levels aged from 7 to 75 years. According to the etiopathogenesis of corneal-conjunctival xerosis, they were divided into 2 groups.
Group 1 included 23 patients (23 eyes) with dry eye syndrome due to a primary disorder of tear production: 15 people (15 eyes) with impaired innervation of the lacrimal glands and 8 (8 eyes) with the absence of the lacrimal gland after its extirpation.
The 2nd group included 62 patients (120 eyes) with dry eye syndrome due to a combined disturbance in the production of tear fluid with increased evaporation of the tear film: 37 people (70 eyes1) with Sjögren's syndrome, 13 (26 eyes) with the reaction " graft versus host" after red bone marrow transplantation and 12 (24 eyes) with ocular cicatricial pemphigoid.
All patients were examined using traditional methods. The severity of each subjective sign of xerosis was determined according to our proposed 4-point scale [16] and summarized into an indicator of subjective discomfort. This scale, in contrast to numerous foreign analogues (OSDI, etc.), significantly simplifies the assessment of the severity of subjective signs of dry eye syndrome and is successfully used in our studies [2].
The severity and objective symptoms of xerosis were determined similarly. All patients scheduled for obturation of the lacrimal ducts also underwent functional tests to assess the function of active lacrimal drainage.
The algorithm for functional examination of patients included sequential performance of diagnostic tests, starting with minimally invasive tests and ending with more invasive tests. The examination began with an assessment of the tear meniscus index. Tear film stability was then assessed using the Norn test. Next, taking advantage of the presence of sodium fluorescein in the conjunctival cavity, the condition of the corneal epithelium was examined, and then the bulbar conjunctiva was examined using 1% rose bengal staining.
Corneal staining with sodium fluorescein solution was assessed using the Oxford scale in our modification, which provides for determining the degree of corneal staining (staining of the conjunctiva was not taken into account) on a 6-point scale. The pattern of staining of the cornea, temporal and nasal parts of the bulbar conjunctiva with a 1% solution of rose bengal was assessed using a 4-point van Bijsterveld scale.
The examination was completed by determining the total and then, after anesthesia with a 0.4% solution of oxybuprocaine (inocaine, Sentiss, India), the main tear production. Based on the difference in their values, the amount of reflex secretion of tear fluid was calculated.
The criterion for verifying the diagnosis of dry eye syndrome was a decrease in the stability of the tear film (its breakup time according to Norn is below 10 s) in combination with one or more pathognomonic signs of xerosis of the ocular surface [2, 16].
The treatment measures performed by all patients with dry eye syndrome at the first stage of the study included instillation of artificial tears and symptomatic medications. The choice of the optimal “artificial tear” drug for each patient (based on subjective sensations) was made based on the results of trial instillations of various such drugs for 2-3 days. In this case, patients with mild and extremely severe xerosis were prescribed low-viscosity drugs, and those with moderate and severe xerosis were prescribed ophthalmic gels. In the presence of systemic diseases, treatment was supplemented with appropriate therapeutic measures prescribed by a rheumatologist (endocrinologist, gynecologist or other specialist).
The effectiveness of therapy was assessed based on positive dynamics according to at least one of the following criteria: a decrease in the severity of clinical (subjective or objective) signs of xerosis by 2 points or more, or a decrease in the degree of staining of the surface of the eyeball according to the Oxford scale in our modification or according to the van Bijsterveld scale by 2 points or more.
Obturation of the lacrimal ducts was performed in two stages: at the first stage it was temporary, and if it was effective, it was permanent. The indication for obturation, along with the insufficient effectiveness of drug therapy, was a decrease in all components of tear production with a positive result of the color nasolacrimal test. All patients continued to receive conservative therapy due to obstruction of the lacrimal ducts.
Temporary obturation of the lacrimal ducts was carried out using an absorbable collagen (or catgut) thread with a diameter of 2/0-4/0, which was inserted into 2 pieces of 3-4 mm in length first into the lower and then into the upper lacrimal canaliculi (Fig. 1).
Rice. 1. Stage of temporary obturation of the lower lacrimal canaliculus with collagen thread.
Permanent obstruction of the lacrimal canaliculi was performed using one of the following methods:
— silicone punctal occluder plugs (Punctal plugs®, FCI, France, Fig. 2);
Rice. 2. Sequence of obturation of the lower lacrimal opening with a silicone plug from FCI (France). a — introduction of an obturator into the lower lacrimal punctum; b — correct position of the obturator in the lumen of the lower lacrimal punctum.
— covering the lacrimal papillae with a free flap of the bulbar conjunctiva according to J. Murube et al. [12] (Fig. 3);
Rice. 3. The main stages of the operation of conjunctival covering of the inferior lacrimal punctum (according to J. Murube et al. [12]). a — the first stage of the intervention: excision of a square-shaped flap of tissue above the lacrimal punctum (1), the lower eyelid is pulled back using a stay suture (2); b — the second stage of the same operation: a graft (3) is excised from the conjunctiva of the eyeball to replace the tissue defect above the lacrimal punctum; c — the third stage of the same operation: the graft (3) is transferred to the prepared “bed” and sutured to its edges with four sutures, the entrance to the vertical part of the lacrimal canaliculus (4) is closed.
— covering the lacrimal papillae with a displaced flap of the tarsal conjunctiva according to the method we developed (together with E.E. Somov) [13] (Fig. 4);
Rice. 4. The main stages of covering the inferior lacrimal punctum with the tarsal conjunctiva. a — the conjunctiva is separated and pulled up to the previously skinned lacrimal papilla; b — the conjunctival flap is fixed with sutures [13].
— diathermocoagulation of the vertical part of the lacrimal canaliculi (Fig. 5);
Rice. 5. Diathermocoagulation of the vertical section of the lower lacrimal canaliculus.
— ligation of the horizontal part of the lacrimal canaliculi (Fig. 6)
Rice. 6. Stage of the operation of ligation of the horizontal part of the lacrimal canaliculus. The tubule is isolated, tied with two ligatures (Vicryl, 8/0) at a distance of 3-4 mm and crossed between the ligatures. - in the absence of effect from previous interventions.
Material requirements
Tooth obturation must be carried out with high-quality materials that meet certain requirements:
- moisture resistance,
- hypoallergenic and good biocompatibility,
- no shrinkage for many years,
- antibacterial effect,
- high adhesion to dentin,
- lack of interaction with tissue fluids,
- easy removal if necessary,
- good radiopacity,
- fast curing period.
List of instruments used for obturation
An endodontist (endodontist) performing such a technically complex procedure must have a high level of professionalism. He also needs to have in his arsenal a set of specialized tools: a spreader for distributing and compacting gutta-percha, a canal filler, a gutta-condenser for filling canals and softening filling materials, pluggers for condensing gutta-percha, “GuttaEst” for heating and cooling gutta-percha.
Clinical cases in which obturation is required
Tooth obturation is a procedure that is performed only on units that are subject to depulpation, that is, removal of the nerve. It is also impossible to do without it if the patient is preparing for prosthetics with crowns or bridges - the teeth that will act as a support for the dentures are exposed to it.
It is necessary to carry out sealing even when the crown of the tooth is destroyed by more than half. Endodontic treatment will help prevent the infection from spreading deeper, strengthen the roots and protect the internal cavities from the destructive process.
Indications
Root hole obturation is recommended for the following dental problems:
- periodontitis (in any manifestation);
- chronic pulpitis;
- acute pulpitis.
When is there a need for filling?
Root filling is indicated for the treatment of a number of dental pathologies and for smile restoration by an orthopedic dentist:
- for pulpitis in adult patients: in children the rudiments of the permanent row are located very close, therefore endodontic treatment of the primary occlusion is not carried out (passing the canals with an instrument can be dangerous),
- in the treatment of periodontitis, cysts and granulomas: inflammatory processes or space-occupying formations under the apices of the roots can be treated surgically - osteotomy, for example. But this option may not be justified from the point of view of severe traumatism with a small pathological focus,
- when preparing a “support” for a prosthesis: artificial crowns, bridges or clasp appliances are attached to previously pulpless teeth in order to eliminate the risk of pulpitis or periodontitis while wearing the prosthesis,
- if the crown is destroyed by 50%: here a standard filling will not provide the necessary strength to the top of the tooth, so it is necessary to install a ceramic inlay, or strengthen the root part with a metal pin and install a crown on top. Endodontic treatment is also carried out to prevent the spread of infection.
Diagram of the difference between pulpitis and periodontitis
Design characteristics
Pins for the structure are made of various materials - silver, absorbent pastes, etc. Gutta-percha together with sealants is very popular.
The pins themselves can be of any shape - cone-like, thermoplastic mass, etc. The doctor selects them individually for each patient.
To accurately secure the pin, sealants made from calcium hydroxide, zinc oxide-eugenol, resin or glass ionomer materials are used.
This design is often used in the treatment of advanced forms of carious lesions (periodontitis, pulpitis, etc.). A pin can only be installed in a tooth that does not cause discomfort to the patient, otherwise additional treatment will be required.
For temporary obturation of primary teeth, pins made of chlorophenol-camphor-menthol composition are used. They are not particularly durable and are ideal for temporary fillings.