Disturbance = inflammation
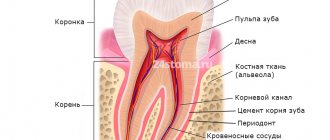
Any disruption of the periodontal ligament and restoration is likely to cause inflammation. Any inflammation in this area can negatively affect the result of the entire work. Understanding the function and location of the ligament increases the likelihood of successful restoration. In particular, factors such as
- position of the gum edge,
- marginal fit,
- contact areas,
- prosthesis shape,
- Iatrogenic damage.
Gum augmentation and plastic surgery
The gums play a very important role. The gum protects the neck of the teeth from harmful or traumatic factors, fixes the tooth itself, and gives the smile a beautiful shape.
Gum augmentation is a procedure during which its shape is changed in order to cover an exposed area of a tooth or correct it around an implant.
The shape of the gums can change after dental interventions, injuries, inflammatory processes (gingivitis, periodontitis) or due to congenital structural features of the jaw, its developmental anomalies, which can be corrected using gingivoplasty. Gum plastic can prevent or eliminate an aesthetic defect and give the gum the desired appearance.
When is gum surgery necessary: indications
- Gum plastic surgery when the root is exposed (recession). One of the most important and common indications for this intervention. Closing gum recession is necessary to prevent tooth decay, reduce its sensitivity, and reduce the risk of developing infectious and inflammatory complications;
- Correction of a gummy smile. Exposing mostly the gums, rather than the teeth, while smiling can be embarrassing for both those around you and the person himself. In such cases, gum plastic will do an excellent job of eliminating the defect, and additional production of veneers will be able to correct any non-standard situation;
- Gum augmentation with implantation or bone grafting. It is produced to cover the bone tissue being built up, fix the implant, and eliminate aesthetic defects.
All types of gingival margin reconstruction directly depend on the gum biotype. The thicker the gingival contour, the cheaper and simpler the treatment. If the gums are of the ultra-thin biotype, any surgical treatment will be a challenge for the patient and the doctor.
Methods for gum extension
There are two ways to perform gingivoplasty: using your own flap of the oral mucosa or using a special collagen matrix or barrier membranes.
Flap plastic flap of the mucous membrane. This technique uses only the patient's own tissue:
- An incorrectly located area of the gum is excised, unable to return to its original position;
- If there is a lack of tissue available at the excision site, a tissue flap is formed from adjacent areas of the mucosa (adjacent gum, palate, inner surface of the cheek);
- The flap or gum edges are sutured under tension in close contact with the tooth surface using surgical knots.
The use of a collagen matrix is somewhat different. The material is simply tightly sewn to the existing defect, which ensures the subsequent formation of its own tissues on the existing collagen mesh.
Gingivoplasty for a gummy smile
With this type of smile, several millimeters of gum, most often the upper one, are exposed. This gives the face an unusual expression when smiling.
Correction of a gummy smile is carried out by excision and modification of excess soft tissue. Thanks to this, the smile and gum contour are given an aesthetically correct shape.
Gingivectomy is also used for the eruption of wisdom teeth or after their removal, for excess gum tissue after installation of a dental implant, for bite correction, and tooth extraction.
Progress of the operation
Gingivoplasty is conventionally divided into several stages:
- Preparing for the intervention. The oral cavity is disinfected using antiseptics or other disinfection methods. If necessary, the surgical field is delimited from other areas of the mucous membrane;
- Anesthesia. Most often, local infiltration anesthesia is used using any modern painkillers or other anesthetics approved by an allergist;
- Tissue dissection. Necessary incisions and excision of excess soft tissue are made;
- Directly plastic. It is possible to directly stitch the incision after removing excess gum, form a flap, or use a collagen matrix with their fixation to the surrounding tissues;
- End of operation. The surgical wound is sutured with surgical sutures.
Postoperative recovery
After gum surgery, it is important to follow certain rules to prevent complications and promote the healing process. This process can take from 5 to 20 days, depending on the extent of the operation performed and the individual speed of regeneration.
- Until healing is complete, you must strictly adhere to the rules of oral hygiene: brush your teeth at least twice a day (do not touch the surgical site with a brush), use special solutions with antiseptics;
- In the first 7-10 days, you may need to constantly wear a special protective mouthguard;
- For the first 5-10 hours after surgery, smoking and eating are prohibited. You can drink after 2 - 3 hours; you can only drink soft boiled or mineral water without gas at room temperature or slightly warm;
- During the entire healing period, it is forbidden to eat hard, spicy, sweet foods. The ban also applies to hot and cold dishes;
- During the entire rehabilitation period, physical activity, flying, diving, off-road driving, sauna, bathhouse are prohibited.
The swelling should completely disappear within 3-5 days after gingivoplasty. If this does not happen or any complications develop (bleeding, enlargement of the operated gum, pain, fever), then you should immediately contact your doctor.
The article used materials from the site: https://doctorlevin.ru/
Impaired passive eruption
When planning restorations, if the volume/height of the gingival tissue is large, it is necessary to remember the phenomenon of altered passive eruption. Such a violation leads to changes in the connection of the periodontium and restoration, which should be taken into account.
Passive eruption involves displacement of the gingival margin in the apical direction, gradual exposure of the crown and securing the edge in the area of the tooth neck. Violation of this process leads to an expansion of the zone of fixation of the gingival margin, that is, it can “stop” away from the CEJ. According to a study by Garber and Salama (1996), impaired passive eruption occurs in 7-14% of the population, predominantly in patients with thick and flat gingival tissue biotypes.
In 1977, Coslet et al proposed the following classification of passive eruption disorders:
- type 1A – wider band of keratinized tissue, normal bone ridge level;
- type 1B – a wider band of keratinized tissue, a bone ridge at the level of the CEJ;
- type 2A – less wide band of keratinized tissue, normal bone crest level;
- type 2B – a less wide band of keratinized tissue, a bone ridge at the level of the CEJ.
Treatment options depend on the type of passive eruption disorder:
- type 1A – gingivectomy, displacement of the flap in the apical direction;
- type 1B – gingivectomy, bone grafting, flap displacement in the apical direction;
- type 2A – displacement of the flap in the direction of the apex;
- type 2B – bone grafting, displacement of the flap in the apical direction.
If passive eruption disorder remains undiagnosed and is not taken into account when drawing up a treatment plan, the complications mentioned above are possible, that is, periodontal inflammation around the restoration (thick biotype) or gingival recession (thin biotype).
CONTENT
- 1 Biomechanical considerations 1.1 Biological width
- 1.2 Tip effect
- 1.3 Crown to root relationship
- 1.4 Treatment planning
- 2.1 Apically repositioned flap with bone recontouring (resection) [13] 2.1.1 Indications
- 2.2.1 Indications
Coronal lengthening
Lengthening the coronal part is a procedure that can minimize the risk of violation of the biological width. When considering the applicability of this procedure to a specific case, one should calculate the feasibility of its implementation in general. Preparation for surgery should include determining the biotype of gingival tissue, assessing its condition, and high-quality x-rays. In some cases, such as severe abrasion/wear of teeth, a sensitivity test should also be performed. A wax up, a wax-up model, is often helpful in discussing the treatment plan with the patient.
Biological width and periodontal complex
In the implant field, biological width is also defined as the distance from the most prominent coronal projection of the connective epithelium to the alveolar bone, including the epithelium (approximately 1 mm) and the connective tissue attachment (approximately 1 mm). By analogy with a tooth, the dentogingival complex additionally contains a section of the implant-gingival sulcus (approximately 1 mm). If this distance is less, resorption of the bone ridge surrounding the implant should be expected (Clin Oral Implants Res. 1991 Apr-Jun; 2(2):81-90 “The soft tissue barrier at implants and teeth” Berglundh T., Lindhe J., Ericsson I., Marinello C.P., Liljenberg B., Thomsen P.).
Biotype of gingival tissue
When lengthening the coronal part, it is important to take into account the biotype of the gum. According to research results, the gingival margin can “grow” along the crown from the level determined during the procedure. This growth is more often observed in patients with a thick biotype of gingival tissue, but there are also individual characteristics. In addition, it is likely that the amount of gingival retraction depends on the position of the flap relative to the alveolar ridge at suturing, as described by Deas (2004). Therefore, if the patient has gum tissue of a thick biotype, it is possible to compensate in advance for the mentioned reverse movement of the edge during the formation of the gum during the operation. A temporary crown should be placed 6-8 weeks after surgery to ensure proper gum formation before the permanent crown is placed.
The Heterburg Study of the Swedish Population
This study (Journal on Dental Researelu 2015 Effectiveness of Implant Therapy analyzed in a Swedish population) is by far the largest on implant survival. Of the 25,000 patients with implants installed in 2003, 4,716 patients were selected. Early implant loss was 4.4% (121 patients) on the patient side and 1.4% (154 implants) on the implant side. Nine years after implant treatment, 596 patients with 2367 implants were evaluated. Late loss was 4.2% on the patient side (25 patients), and 2% on the implant side (47 implants). Overall loss: patients 7.6%, implants 3%.
When assessing the prevalence of caries or periodontitis, the number of patients with these diseases is considered, and not the number of affected teeth, so implantation failure should be assessed in terms of the number of patients, not implants. Thus, the survival rate of implants over 10 years is 93%, and not 97%, these data allow a more realistic assessment of the result and improve clinical work.
Gum enlargement after orthodontics
After orthodontic treatment aimed at lengthening the coronal part, enlargement of the gums is often observed, i.e. its edge rises above the desired level. In such cases, you should not immediately take up a scalpel and surgically remodel the gum. The gums will return to the desired shape on their own within 3-6 months after treatment. At these marks it is already possible to assess its condition and decide on the need for surgical correction of the edge.
In the “Orthopedics” department of the Stommarket.ru online store you will find a variety of materials necessary for successful restorations of various levels of complexity:
https://stommarket.ru/catalog/ortopediya/
Nice prices and excellent delivery conditions!
Presence of root caries in teeth and severe dentoalveolar deformations
Before
Stages
After
Specialists:
Kyalov Grigory Georgievich
Description:
The patient came to the clinic on a recommendation from friends who had undergone successful implantological treatment at the NK Clinic.
After an initial consultation, X-ray examination and functional planning, it was proposed to remove teeth 38, 37, 47, 48 and 26. The reason is the presence of root caries in each tooth and severe dentoalveolar deformations, in the presence of which it is impossible to create an effective and correct chewing function. We removed the corresponding teeth and performed simultaneous dental implantation. Three months later, we produced separate ceramic crowns on individual zirconium abutments, supported by dental implants. Thus, we were able to completely restore chewing function.