Causes Danger of fistula Diagnostics Treatment Prevention
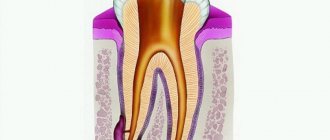
A fistula on the gum is a pathological condition, the result of purulent inflammation near the root of the tooth with perforation of the gum tissue. This is a channel in the thickness of the gums through which pus comes out from the source of inflammation.
The disease is diagnosed and treated by dentists: a therapist, a surgeon, and sometimes a maxillofacial surgeon.
What is a fistula, what does it look like, symptoms
Externally, the fistula is a convex formation with a noticeable white spot on it. This means that the pathological process is accompanied by the formation of pus in large quantities.
There are two types of fistula:
- External, when the gum fistula comes to the surface;
- Internal, when the process remains hidden inside the gum, due to the fact that the fistula channel does not reach its surface. The inflammatory process can only be detected by x-ray examination.
Symptoms of a dental fistula are detected primarily by visual examination. There is a noticeable bulge on the gum, from where pus comes to the surface. There are other signs:
- The pain is cutting, stabbing, spasmodic. Becomes stronger with impact (for example, when chewing), weakens slightly after some of the purulent contents come to the surface;
- Putrid odor;
- Foreign tastes in the mouth;
- Tooth mobility with pathology;
- Swelling of the gums in the area of inflammation;
- Discharge of mucus with pus;
- Increased temperature, symptoms of intoxication of the body;
- Inflammation of the lymph nodes.
Causes of a fistula on the gums in an adult
A fistula is formed due to an infectious purulent process in the dental canal. Pathology can occur for the following reasons:
- Deep caries and untimely treatment;
- Newly emerging periodontitis and periostitis with the formation of pus;
- Chronic periodontitis, damage to the walls of the tooth root;
- Cystic formations;
- Oncology;
- Pulpitis, damage to the tooth root;
- Granuloma.
Fistula also occurs after tooth extraction. This is a common pathology that occurs as a result of infection in the wound.
A fistula after dental treatment can form, for example, due to infection as a result of errors in the treatment of caries. Improper filling of a tooth can also lead to the development of pathology. In this case, a tooth root fistula is formed when pus, having passed through the dental canal, breaks into the surrounding tissue. The most common fistula of the upper and front teeth occurs.
Alcohol, smoking, stress, exacerbations of chronic diseases, abuse of carbohydrates, lack of nutrition, chronic diseases - all these factors increase the root causes of the disease.
What to do if the gums near the crown become inflamed
Inflammation of the gums near the tooth under the crown is treated based on the original cause that caused it. So, if swelling of the soft tissues appears as a result of trauma to the gums with a brush or due to the chemical components included in the rinses, it is enough to replace oral hygiene products with more suitable ones, and treat the gums themselves with antiseptics.
If swelling of the gums is caused by the development of dental pathology - gingivitis, periodontitis, etc., complex treatment is necessary - professional cleaning, curettage of periodontal pockets, application of anti-inflammatory and wound-healing ointments, injection of vitamins and sometimes antibiotics into the gums.
When flux forms, it is opened and the wound is drained.
If the flux has opened on its own and a fistulous tract has formed, endodontic treatment is carried out (if a crown covers a living tooth or not all root canals are filled) or resection of the apex of the root on which inflammation has formed. If it is presented late, it is not always possible to save the tooth under the crown and then it is removed. To the list of posts
How dangerous is a fistula? Consequences
The fistula itself does not pose a danger, since through it the pus is removed from the source of infection, and accordingly, the degree of tissue damage is reduced. But the presence of a fistula indicates that the process is serious, and various types of complications may arise, such as:
- Loss of teeth in the affected area;
- Attachment of a secondary infection - inflammation of the lymph nodes, ears;
- Sinusitis;
- Sinusitis;
- Damage to bone tissue;
- Sepsis as a result of infection entering the general circulatory system;
- The appearance of cystic formations at the roots of the tooth;
- Heart complications, bacterial endocarditis.
Sometimes it happens that the pus drains almost completely, the fistula heals, and the patient thinks that everything is gone. But in fact, the source of inflammation has not been eliminated, so relapse of the disease is inevitable. Repeated abscesses and fistulas are more difficult to treat.
Why did an abscess appear on the gum?
The main, main cause of abscesses is the penetration of infection into the gum tissue. In this case, a reaction of the body’s defenses occurs: leukocytes that destroy hostile cells die, and a large amount of pus accumulates at the site of infection. As a result, a pus-filled sac forms in the gum tissue, which can gradually increase in size and eventually rupture. Infection can enter the gum tissue in a variety of ways. In addition, the formation is promoted by the presence of diseases of the gastrointestinal tract, immune system, permanent plaque on the teeth and tongue, and smoking.
There are many factors that increase the risk of developing abscesses inside the oral cavity, but ultimately all the reasons come down to two main ones:
- Periodontitis
Periodontitis is a disease in which a focus of infection forms at the very root of the tooth (usually at the apex). The development of periodontitis is caused by untreated caries and advanced pulpitis (inflammation of the soft tissues of the tooth). Often, the infection penetrates into the tissue surrounding the tooth root during dental procedures and manipulations - for example, when the dental canals are not completely cleaned during the treatment of pulpitis or when the filling is not dense enough. The development of periodontitis is also facilitated by the presence of chronic infectious diseases that cause a steady decrease in the activity of the body's defenses, stress and overwork, and the presence of bad habits. Infectious foci often arise under crowns when they are installed poorly.
Sometimes periodontitis can affect two teeth at the same time. Most often, when this disease occurs, patients complain of severe pressing, aching, acute pain and swelling, but in some cases these symptoms may be absent. Over time, pus accumulates inside the gums, and the cavity containing it expands to the boundaries of the outer mucous membrane of the gums. As a result, an “abscess” or fistula (a small hole through which pus comes out) may form on its surface.
A common result of periodontitis is the appearance of cysts or granulomas - benign formations associated with changes in the structure of the tissues of the oral cavity. To diagnose such conditions, X-ray examination is used, which often makes it possible to detect the disease in the early stages of development and prevent the formation of an abscess. However, due to the latent course of the disease in the initial stages, diagnosis is sometimes difficult: often the presence of infection in the root apex is discovered by chance, when examining other teeth.
The release of pus to the surface of the gum and the formation of an abscess on the gum in the mouth is most often accompanied by acute pain. However, if inflammation on the gums does not hurt, this does not mean that the disease is progressing favorably and you can postpone a visit to the dentist. The absence of pain is usually due to the fact that when a fistula or abscess forms, the pressure of pus on the root and nerve of the tooth decreases. But the main cause of the disease, the focus of chronic infection, still persists. In addition, ulcers without pain often turn out to be formations of other types - for example, wen or benign tumors.
If a white abscess forms on the gum, this usually indicates the presence of a focus of inflammation deep in the gum, at the root of the tooth. Due to the deep location of the infectious focus, characteristic signs of inflammation are often absent.
- Periodontitis
Periodontitis is a disease in which “pockets”, areas of sagging gum tissue, form between the lower edge of the teeth and the gums. As a result, cavities are formed in which food debris and bacterial mass accumulate. All this creates the most favorable conditions for the emergence of a focus of infection, which subsequently leads to inflammation.
As a result of the constant presence of pathogenic microorganisms, the part of the gum adjacent to the tooth becomes inflamed, becomes red and swollen, and may bleed when brushing or applying pressure. The deepening of the gum pocket against the background of the constant presence of a source of infection leads to the accumulation of pus in it, as a result of which an abscess is formed.
Unlike periodontitis, with periodontitis the source of inflammation is not deep in the gums, but on the surface. Therefore, even with a simple examination, you can detect characteristic signs of inflammation: swelling and redness. Since periodontitis pockets often form on several or even all teeth of the jaw, the abscesses caused by this disease can also be multiple.
Diagnostics
First of all, this is a visual inspection. An external fistula is visible to the naked eye. If the fistula in the jaw is hidden, an x-ray is taken. With the help of X-ray examination, the focus of inflammation and the depth of the pathological process of damage to the periosteum are accurately identified. It is important to distinguish a fistula from gum tissue, purulent tissue inflammation and other pathologies.
Self-medication of such a disease at home and self-diagnosis are unacceptable. Treatment is carried out under the supervision of a doctor, which he prescribes based on the diagnostic results.
Treatment of fistula on the gum
There are several ways to treat a dental fistula: surgery (the most common) and methods for treating a dental fistula without tooth extraction. When surgically removing a fistula on the gum, the inflammatory cavity is opened, cleared of pus, and then drainage is installed to ensure the outflow of purulent contents. Surgical treatment is clearly indicated for a large area of damage, when a fistula occurs over a tooth covered with a crown, or when there is damage to the periosteum.
In the medical treatment of gum fistula, conservative methods are used.
It could be:
- Endodontic therapy (teeth preparation; cleaning of canals, elimination of inflammation, filling);
- Drug therapy (used at all stages of work to eliminate pathology) involves taking antibiotics, NSAIDs, antihistamines;
- Physiotherapy. It is never prescribed separately, only in combination. Increases the effectiveness of any treatment methods.
Why does the gums around the crown become inflamed?
In addition to mechanical damage, the gums can react with swelling due to the irritating effect on it of chemicals contained in oral hygiene products - toothpaste, rinses.
However, swelling of the gums near the tooth under the crown can be caused by more serious reasons. For example, swelling may be a sign of:
- Gingivitis or periodontitis. It usually appears due to poor oral hygiene, the presence of dental plaque, malocclusion, poorly fitting crowns, as well as hypovitaminosis and endocrine disruptions. At first, the gums swell and bleed, darkening of the gums around the tooth at the crown may be observed, and later suppuration and tooth mobility occur.
- Flux, or periostitis. This disease affects the hard periodontal tissues and, in particular, the periosteum of the jaw. Very often, tooth flux under the crown is a consequence of asymptomatic pulpitis or periodontitis. If the flux is not treated, there are two possible options for the development of the disease - involution of the flux and its spontaneous opening. In the second case, a fistula forms on the gum (tooth under the crown), through which purulent contents flow. In this case, the pain subsides, but the inflammatory process itself continues and without appropriate treatment, osteomyelitis of the jaw can form.
- Alveolar process abscess is another complication of pulpitis, periodontitis or caries occurring in the tooth under the crown. With this disease, the patient will complain not only of swollen gums above the crown of the tooth, but also of severe pain in the jaw, aggravated by exposure to heat, facial asymmetry, and unilateral enlargement of the submandibular and cervical lymph nodes.
- Overloading a denture with irrational prosthetics can lead to the tooth crown moving away from the gum and food starting to get clogged under it. As a result, mobility of the supporting teeth appears, and the soft tissues of the oral cavity become inflamed (gingivitis).