Inhalation anesthesia
This is the most commonly used type of anesthesia, which is characterized by ease of implementation, relatively easy control and short duration of action, which is important for minor surgical interventions. Inhalation anesthesia is the administration of drugs through a mask, which ensures their entry into the organs of the respiratory system. Most often, Narcotan, nitrous oxide, Trilene, Ftorotan and Etran are used for this type of anesthesia. There is a certain problem - to achieve the desired result, it is necessary that the effect of anesthesia be deep, and this is fraught with serious complications. Therefore, this type of anesthesia is most often used in pediatric surgery. Children under anesthesia administered by inhalation feel excellent, they do not experience respiratory dysfunction, and complications are extremely rare.
Not everyone can handle it
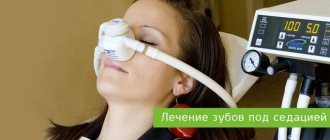
In recent years, it has become fashionable to treat teeth under anesthesia. A huge number of large and small medical centers have opened that actively advertise such treatment, but they are often completely unsuited to providing safe anesthesia. Meanwhile, dentistry is the only area where general anesthesia can often be associated with significant risks. Even in the USA and Europe, where the level of medicine is significantly higher than in Russia, doctors try to avoid anesthesia during dental procedures. The fact is that in this case, the anesthesiologist does not have access to the respiratory tract, is not able to control their protective reflexes, and cannot always prevent fluid (blood, pus) from flowing into the trachea - and such situations are life-threatening.
| Important | |
| If a patient suffers from bronchial asthma, he should definitely tell the doctor about it. The fact is that with this disease, additional funds may be required during anesthesia. | |
Unfortunately, in our country, the willingness to pay often becomes the main indication - so to speak, “any whim for your money.” Dental treatment under anesthesia is exactly the case when you shouldn’t be capricious without good reason; the price can be prohibitively high. And if there is a real need for this, you must definitely contact specialized centers that have an operating unit with the necessary equipment, it is possible to provide emergency care, and in an emergency, place the patient in intensive care or at least in a post-anesthesia observation ward.
In all other cases, there are no contraindications to general anesthesia. On the contrary, some medical procedures and examinations are much more convenient and safer to do under anesthesia. For example, colonoscopy (examination of the intestines) throughout the civilized world is a necessary procedure for medical examination in people over 50 years of age, and it is necessarily performed under anesthesia. And the point is not only that without anesthesia it can be painful and psychologically uncomfortable. Another point is that if a patient has a bad heart or hypertension, then enduring pain is quite dangerous for him, and this can more often lead to complications than properly administered anesthesia.
Of course, the higher the qualifications of the anesthesiologist, the lower the risk of side effects from the use of anesthesia. And there is only one way out: when preparing for an operation or examination under general anesthesia, you need to choose a medical institution as carefully as possible, go not to where it is “cheaper and closer to home,” but to those specialists who inspire trust. It is better to rely not on intrusive advertising, but on objective information, on the experience of relatives and friends. You should not at all strive to ensure that your anesthesiologist is a candidate or doctor of science; it is much more important that he has extensive experience and extensive practice.
Intravenous anesthesia
This type of anesthesia refers to non-inhalation types of anesthesia, which are characterized by a long-lasting effect and a greater depth of effect compared to inhalation anesthesia. Intravenous anesthesia can be performed using the following drugs:
- Thiopental, Recofol, Oxybutyrate and Propofol - classic pain relief
- Fentathyl with diphenhydramine - neuroleptanalgesia, which can be carried out on spontaneous breathing or combined with artificial ventilation
- Sibazon with Fentathyl is ataralgesia, which provides superficial, gentle anesthesia and can be carried out with other types of anesthesia.
This type of anesthesia is used to remove abscesses and phlegmons that occur with complications; it is also possible to treat small benign tumors if their removal under general anesthesia is not possible.
How long does dental anesthesia last?
This is another important point. It is important for the patient to know that it will not hurt and to understand how long the dental anesthesia lasts. The last factor can be decisive for planning work functions for the rest of the day. Insensitivity increases the risk of injury to the tongue and mucous membranes, which is why dentists recommend refraining from eating and active speech. In the case of conduction anesthesia, problems with diction and swallowing may occur.
find out how long dental anesthesia lasts in your particular case from your attending physician. He selects 1 drug or combination and selects the dosage. The effectiveness of pain relief will depend on the sum of these criteria.
How many hours does it take for the tooth to be anesthetized depends on the drug and dosage
- Drugs with a short duration of analgesia give an effect for 30-60 minutes. For example, novocaine “works” for up to 1 hour, but in combination with adrenaline, the duration of action is extended to 90 minutes.
- The average duration of anesthesia for infiltration injection with lidocaine is 1.5-2 hours.
- Ultracaine - gives a high effect, lasts up to 5 hours, and Bupivacaine can freeze the injection area for up to 8 hours.
to predict exactly how long anesthesia will last for dental treatment for a particular patient only by taking into account all individual factors. Your doctor can guess the average exposure time, but it may vary.
Local anesthesia
Treatment under anesthesia is the only option for providing surgical care to a patient or performing complex manipulations. Often, a doctor will numb a specific area, which is achieved by injecting it with an anesthetic solution and is called local anesthesia. This type of anesthesia is used for opening ulcers, treating teeth, and excising a hernia. Local anesthesia is the injection of an anesthetic into the skin and other anatomical structures of the place where surgery is expected to be performed.
The anesthetic injections are superficial; only in exceptional cases can the doctor administer the drug more deeply. Local anesthesia is performed by injecting the drug through a very thin needle, so the actual anesthesia procedure is minimally painful. Often, the administration of an anesthetic is combined with sedation - sedatives are introduced into the patient’s body, which normalize the person’s psychological state, reducing feelings of anxiety and restlessness.
Despite the fact that local anesthesia is used very widely in medicine, the consequences of anesthesia can be quite serious. For example, local anesthetics can have a negative effect on the heart and brain, leading to heart rhythm disturbances, seizures and loss of consciousness. At the same time, doctors claim that local anesthesia, compared to general anesthesia, is safer for the patient’s health.
How anesthesia and anesthesia work: myths, fears, side effects
An alternative to spinal anesthesia can be epidural, when a local anesthetic is injected into the epidural space located in the spine through a special catheter. Depending on the type of operation (chest, abdominal cavity), the anesthesiologist determines the place of its introduction. In this case, the doctor can inject not only a local anesthetic into the epidural space, but also opioid painkillers that enhance the effect. Sometimes the epidural catheter may be left in place temporarily to provide pain relief as required by the patient (called an extended epidural).
More complex and serious interventions are always associated with lengthy preparation on the part of the anesthesiologist - installation of a central venous catheter, administration of infusion therapy, correction of blood coagulation parameters and other important parameters. It is also important to consider whether the operation is an emergency or a planned one.
Can you tell me more about the difference between spinal and epidural pain relief?
During spinal anesthesia, the drug is injected at the lumbar level into the subarachnoid space (into the cavity between the pia mater and the arachnoid mater of the spinal cord, filled with cerebrospinal fluid). Usually everything is limited to a couple of injections. In this way, the soft tissues above the injection site are anesthetized and the drug is directly administered under the dura mater. This anesthesia lasts from two to six hours and is technically easier to administer.
During epidural anesthesia, the drug is injected into the space between the dura mater of the spinal cord and the periosteum of the vertebrae, which contains connective tissue and venous plexuses. It is located closer to the skin compared to the spinal one. Anesthesia is given at any level of the spinal column. It is considered a technically more complex manipulation.
I've read that epidurals can cause paralysis.
This is a common fear, but anesthesiologists say that today it is practically impossible. Such a complication could arise after surgery due to improper care of the catheter, as a result of which the patient developed purulent epiduritis, which caused neurological symptoms with loss of function of the lower extremities. Or due to incorrect actions of the anesthesiologist, when puncture of the epidural space occurs at high levels (there is a risk of unintentional damage to the spinal cord). But in most cases, epidural anesthesia does not threaten anything other than a headache for several days after surgery.
Can everyone have anesthesia?
In life-threatening situations when a person needs surgery, doctors almost always use anesthesia. For example, if there is a victim of an accident on the couch who urgently needs surgery, the risk of having it performed with anesthesia for any health condition will be less than the risk of refusing it.
If a patient comes for a planned operation, then the anesthesiologist is obliged, after collecting an anamnesis, to select the appropriate type of anesthesia taking into account the patient’s health. Doctors are guided by the rule: the volume and risk of anesthesia should not exceed the risks on the part of the surgeon. The patient's age cannot be a contraindication. Specialists take into account all severe chronic diseases that complicate the state of health, and allergic reactions to anesthesia components.
Is there a difference between old and new drugs?
Yes there is: in their consumption, efficiency and safety of use. However, it is invisible to patients; To appreciate the difference, you have to be an anesthesiologist.
How to prepare for anesthesia and how to survive recovery from it?
Preparation depends directly on the type of anesthesia and surgical intervention. The doctor will tell you what and how best to do before the operation. Just build a trusting relationship with your treating doctors, it will be much calmer.
Each patient experiences recovery from anesthesia individually; not everyone feels bad, but many feel nausea and drowsiness, and muscle tremors. It all depends on the characteristics of the body and the drugs that were administered during the operation. After waking up, it is important to listen to your body and report any deviations to your doctors.
Endotracheal anesthesia
One of the most commonly used methods of anesthesia when performing complex surgical interventions is endotracheal anesthesia, which involves immersing the body in a state of deep narcotic (medicinal) sleep. At the same time, the muscles completely relax, and the patient does not breathe independently. To achieve the desired state, doctors carry out a set of measures for the patient:
- Tracheal intubation is the insertion of an endotracheal tube into the lumen of the trachea, which is needed to provide artificial ventilation of the lungs.
- Intravenous administration of narcotic anesthetics, sedatives and tranquilizers.
- Administration of muscle relaxants – they block neuromuscular transmission.
- Artificial ventilation.
The quality of endotracheal anesthesia depends not only on the experience of the anesthesiologist, but also on how correctly the patient’s condition is monitored. It is imperative to monitor blood pressure, pulse, and oxygen saturation.
After general anesthesia
Even after a good general anesthesia, in the first hours there is short-term confusion, disorientation in space and time, drowsiness, nausea, and dizziness. As the anesthetic drugs wear off, pain appears in the postoperative wound, but it is successfully relieved by the administration of strong anesthetics.
After general anesthesia with an endotracheal tube, patients complain of pain and sore throat caused by irritation of the mucous membrane of the upper respiratory tract, but this symptom, like nausea, passes very quickly. As a rule, patients feel well 3-4 hours after surgery, and on the second day they leave the clinic and return home.
What foods can you eat?
You need to switch to a special diet at least 3 days before the examination. It is better if this period is 5-6 days. The following products are allowed to be consumed:
- Low-fat cheeses, kefir.
- Eggs.
- Buckwheat porridge.
- Boiled lean meat.
- Boiled fish of low-fat varieties.
- Honey, sugar, jelly.
- Mashed potatoes (small quantities).
If you are having a colonoscopy, you need to pay maximum attention to preparing for the procedure at home. Diet violations should not be allowed; this can lead to the accumulation of gases and feces in the intestines, which will greatly complicate the examination.
What preparation is needed?
Before general anesthesia, a special examination is required:
- General blood analysis
- Coagulogram
- General urine analysis
- Biochemical blood test (sugar, bilirubin, urea, creatinine, total protein)
- Antibodies to hepatitis B, C, HIV, Microreaction not older than three months
- EGC not older than a month
- Fluorography of the chest organs over the past year
- Blood for blood type and Rh factor
When the necessary tests have been collected, the anesthesiologist must examine the patient along with the examination results, ask the patient about important aspects of his health, and comment on the upcoming procedure. Given the fact that muscles relax during medicated sleep, the risk of stomach contents flowing into the respiratory tract increases. That is why planned interventions are carried out on an empty stomach.
Rule two. Follow the anesthesiologist's recommendations
The anesthesiologist must talk to you the day before if you are undergoing elective surgery. Tell us in detail about all the problems that bother you and how you endured anesthesia before.
Take seriously the regimen that you will be advised to follow before the operation - do not smoke, do not drink liquids. It is prescribed to prevent complications and extreme situations.
Article on the topic
Advice from an anesthesiologist: Which anesthesia is safer?
If you are prescribed any medications the night before or the morning before surgery, do not ignore this order. As a rule, strong sleeping pills are prescribed before surgery, which already represent the first stage of anesthesia. They will ensure that you get a deep, relaxing sleep before surgery and that other painkillers work properly.
How does the drug affect the body?
The mechanism of action of Propofol has not yet been fully studied. Its main effect is associated with the fact that it enhances and prolongs the action of GABA (gamma-aminobutyric acid), an amino acid that plays the role of an inhibitory neurotransmitter in the central nervous system, responsible for calm, relaxation and sleep.
When administered, Propofol begins to act almost immediately - it instantly penetrates the brain and causes rapid onset of sleep. Next, a maintenance dose of the drug is administered through an intravenous catheter. An anesthesiologist, using special equipment, controls the depth of sleep, the dosage of incoming medication, the patient's breathing, blood oxygen saturation, blood pressure and heart rate. After completing the treatment procedures, the supply of Propofol is stopped, and the patient wakes up after 5-10 minutes as if from a normal sleep.
How is the period after?
In the first minutes after waking up, the patient may experience some discomfort, however, the unpleasant sensations quickly fade away and after an hour and a half, patients are in their usual state of mind. Sometimes, after waking up, patients may experience nausea and vomiting. That is why it is recommended to take a short pause between waking up and the first intake of water and food. Fortunately, if the above-described discomforts occur, they are quite fleeting.
Post Views: 1,199