Tooth extraction is a common, but complex operation that is fraught with the development of complications, even with the capabilities of modern dentistry. After it is carried out, acute alveolitis develops more often than other complications. Alveolitis refers to inflammation of the walls of the socket that appears after tooth extraction. The risk of this disease can be reduced by strictly observing sterility during surgery to remove a diseased tooth. Much in this case depends on the professionalism of the doctor who performs the operation.
What factors contribute to the development of alveolitis
Most often, this disease is caused by injuries to the walls of the socket, which themselves are very thin. An inexperienced doctor during tooth extraction can cause varying degrees of damage to the hole or even break the wall. In addition, if the doctor lacks experience, the remains of bone tissue remaining after tooth extraction can get into the wound and cause the development of infection in it. The greatest risk of developing alveolitis is when a wisdom tooth is removed.
Another common cause of the development of alveolitis is considered to be insufficient sterility during surgery. Modern dentistry is equipped with very good antiseptics, but even they do not ensure 100% sterility of soft tissues during tooth extraction surgery. Especially if the tooth could not be saved due to the development of purulent inflammation.
In some cases, alveolitis develops as a result of weak immunity, which cannot cope with pathogens even during a course of treatment with antibiotics, which may be prescribed after tooth extraction. Therefore, if a person has an aggravated chronic disease or has developed an acute respiratory disease, it is strictly not recommended to remove his tooth. If a person with a weakened immune system had to have a tooth removed, then after the operation he should avoid contact for some time with people who have diseases that are transmitted by airborne droplets (such as influenza and sore throat). Elderly people, as well as those suffering from cancer, diabetes mellitus or immunodeficiency, are required to be prescribed antibiotics after tooth extraction.
Also, the development of alveolitis can be caused by the absence of a blood clot, which should appear in the socket after tooth extraction. Such a clot provides reliable protection of the hole from the ingress of pieces of food into it, which harbor pathogenic bacteria. That is why an experienced specialist, before removing a tooth from a patient, checks how well his blood clots and asks whether he is taking warfarin, aspirin and coagulants. Even a simple failure to follow the dentist’s recommendations after tooth extraction can cause the development of alveolitis. If the patient touches the place where the tooth used to be with his fingers, does not rinse the mouth with the means prescribed by the dentist, and does not maintain sufficient oral hygiene, then inflammation of the walls of the socket will certainly develop.
Preventive measures for alveolitis
Any patient who has had a tooth removed can minimize the risk of developing the disease. To do this, he needs to strictly follow all the surgeon’s recommendations, namely:
- stop the bleeding in the first two hours after the procedure by placing a sterile tampon on the hole (you need to bite it firmly and hold it for at least half an hour);
- if a wisdom tooth has been removed and the bleeding lasts longer, take a hemostatic drug;
- Do not under any circumstances remove a blood clot that has formed in the socket;
- carry out hygienic brushing of teeth, being careful to avoid damage to the wound and displacement or destruction of the clot;
- Avoid consuming cold/hot, spicy/salty foods during the recovery period;
- refuse to take hot baths and visit baths and saunas;
- use anti-inflammatory drugs such as Metrogyl Denta.
You can eliminate the risk of developing alveolitis due to the doctor’s fault by making an appointment with CELT surgeons for removal... Well, if you are faced with this disease, get it treated with us by making an appointment online or contacting our information line operators: +7 (495) 788-33 -88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Symptoms of alveolitis
In the first few days of the development of this disease, it is asymptomatic. But as the source of infection grows (usually on the 2nd or 3rd day after tooth extraction surgery), the following symptoms appear:
- weak aching pain that appears when eating (with the development of inflammation, the pain becomes shooting, and the source of its origin from the hole spreads to the entire jaw, in addition, it can radiate to the temple and ear);
- very unpleasant sensations that occur every time you open your mouth;
- a rise in body temperature up to 39 degrees is possible, but often this disease resolves against the background of normal body temperature;
- apathy, aching joints and muscles, chronic fatigue, headache and other symptoms of intoxication;
- swelling of the gums, severe redness (with advanced alveolitis, the gums may become bluish, which may indicate tissue necrosis);
- absence of a blood clot in the socket.
After wisdom tooth removal, a symptom of alveolitis is bleeding or the so-called “dry socket,” when a blood clot disintegrates for some reason, resulting in exposed bone. Also a sign of the development of alveolitis is paresthesia, which appears as a consequence of damage to the facial nerve.
Anatomy of teeth
|
Each tooth has three parts: the crown of the tooth, the neck of the tooth and the root of the tooth. The crown of the tooth rises above the gum. It is covered with a very durable fabric - enamel, which contains 96-97% inorganic substances and only 3-4% organic.
- The inorganic substance of tooth enamel is represented mainly by hydroxyapatite, containing trace elements (magnesium, zinc, strontium, copper, iron, fluorine, etc.).
- The organic substances of tooth enamel are represented by proteins, lipids, and carbohydrates. Their content varies between 1.2-1.5%.
Tooth enamel also contains 3.5-3.8% liquid, which is of great importance for the physiological processes occurring in the enamel.
After teething, the process of enamel maturation occurs for 3-5 years, during which calcium compounds, phosphates, microelements and other substances enter the tooth enamel, contributing to the physiological process of its mineralization and increasing its strength.
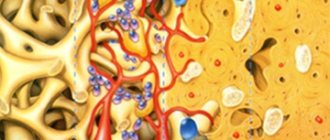
The bulk of the tooth crown and tooth root consists of dentin - a bone substance impregnated with calcium salts. Dentin contains 70% inorganic substances and is penetrated by tiny tubules containing feeding fibers and nerve endings. In 1 sq. mm of dentin there are up to 75,000 such tubules.
The root of the tooth is located in the cell of the jaw bone and consists of dentin, which, in turn, is covered on the outside with softer tissue - cement (46% inorganic compounds). Between the root and the alveolus (socket) there is a narrow, slit-like space filled with connective tissue. This is the periodontium of the tooth. Periodontal fibers are woven with their ends into cement and bone tissue of the cell and, thus, strengthen the tooth in the alveolar process of the jaws. From the walls of the alveoli, blood vessels penetrate into the periodontium, feeding the dental tissues, and nerve fibers pass through.
In the middle of each tooth there is a cavity that turns into a narrow canal ending in an opening at the apex of the root. In this cavity of the tooth crown there is pulp - dental pulp , which nourishes the tooth tissue. The dental pulp is connected to the rest of the tissues of the jaw by a neurovascular bundle, which passes through an opening in the apex of the tooth root.
Between the root and the crown of the tooth there is a neck of the tooth , covered with cement, and covered with a gingival edge on top. The following teeth are distinguished on each jaw: incisors (central and lateral), canines, small molars and large molars.
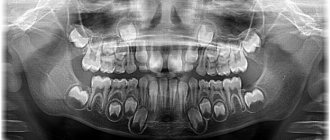
Humans erupt teeth twice. First, the so-called milk or temporary teeth appear.
- The timing of their eruption varies depending on the development and general health of the child.
- Usually teeth appear at 6-8 months of life. First, the incisors erupt, then the canines and molars.
- By the age of 2-2.5 years, all 20 temporary teeth should erupt.
- Permanent teeth begin to emerge at 5.5-6 years of age.
- By this time, temporary teeth begin to loosen and fall out.
- The first to appear are the large molars, then the incisors, small molars, canines, and the second large molars.
- By the age of 14, temporary teeth are usually completely replaced by permanent teeth.
- Somewhat later, the third large molars appear, or, as they are also called, “wisdom teeth.”
- Approximately 25-30% of people are missing some or all of their wisdom teeth.
- Thus, an adult human should have between 28 and 32 teeth (depending on whether the third molars have erupted).
On the upper and lower jaws, the teeth are arranged in the form of dental arches, forming the upper and lower dentition, respectively. With the correct relationship of the dentition during closure, the front teeth overlap the lower ones by 1/3 of the tooth crown, and each tooth of the upper and lower dental arches comes into contact with two teeth of the opposite jaw. A certain relationship between the dentitions is called occlusion .
Prepared by: dentist-therapist V.V. Plesovskikh.
Forms of alveolitis
After tooth extraction, the following forms of alveolitis may develop:
- Serous, which is manifested by aching pain that intensifies while eating. With serous alveolitis, the patient's condition is satisfactory, and his body temperature remains normal. With this form of alveolitis, there is almost or complete absence of a blood clot in the socket, as a result of which food debris accumulates in it. Serous alveolitis develops within three days after tooth extraction. If adequate treatment is not carried out within a week after the development of this disease, complications are highly likely.
- Purulent, which is manifested by very severe pain, bad breath, and a rise in body temperature to 38 degrees. A person with a purulent form of alveolitis experiences severe lethargy, his skin becomes pale, and every meal causes increased pain. The face of such a patient swells and the lymph nodes become enlarged. When examining a patient with purulent alveolitis, the dentist discovers hyperemia and a grayish coating.
- Chronic purulent, the symptoms of which sometimes increase and decrease. During diagnostics, the dentist discovers that the patient has overgrown soft tissue in the area of the socket, and a gap appears between the bone wall and the tissues. In this case, pus is found in the hole, swelling of the mucous membrane is observed, which may have a bluish tint.
Alveolitis of the tooth: treatment
The treatment of alveolitis after tooth extraction must be taken seriously, since the disease will not go away on its own, and its consequences can be very serious:
- blood poisoning
- abscess
- osteomyelitis
- phlegmon
- periostitis
Only an experienced dental surgeon will create an effective treatment plan. It is better to start it when the first signs of the disease appear. The treatment process may include:
- numbing the affected area using anesthesia
- washing the hole with warm antiseptic solutions
- removing particles of tissue decay that remain after washing using a sharp surgical spoon
- treatment with a sterile cotton swab
- applying a gauze bandage with iodoform impregnation or an anesthetic and antiseptic bandage
- impregnation of soft tissues at the site of inflammation with anesthetic and lidocaine
- application of antiseptic tampons, hemostatic sponge with kanamycin
- removal of dead tissue
- microwave therapy, fluctuarization, infrared laser beams, ultraviolet irradiation
- prescribing vitamins, analgesics and sulfa drugs
- antibiotic therapy
With proper treatment of serous alveolitis, the inflammatory process subsides after 3–4 days.
A week after the pain disappears, the walls of the socket begin to heal and become covered with new mucous tissue. After 14 days, the swelling subsides and the mucous membrane takes on a normal pink color. After treatment of purulent alveolitis, the wound heals within 1–2 months, and tissue restoration takes about six months.
Diagnosis of alveolitis
To diagnose alviolitis, no tests or complex manipulations are required. If a person, a few days after tooth extraction, begins to feel pain in the socket area, if the soft tissues in the area of the operation swell, if he feels weak or his body temperature rises, then he should consult a doctor as soon as possible.
Any experienced doctor can diagnose alveolitis by visual examination. Sometimes a blood test may be ordered to clarify the diagnosis.
Restoration of dental-alveolar defects: a multidisciplinary approach
Correction of alveolar ridge defects is a complex clinical task from a functional and aesthetic point of view, which dentists have to solve at the stage of preparation for the dental implantation procedure. The bone crest of the jaw performs two important functions for a dental implant: biological - by essentially providing a “shelter” for intraosseous support, and aesthetic - by supporting the architecture of the peri-implant soft tissues.
Furhauser et al developed a special pink aesthetics score that measures the success of the aesthetic component of treatment using single intraosseous supports. High rates of pink aesthetics are achieved due to the complete immersion of the implant into the structure of the bone ridge, while maintaining (or restoring) the proper contours of the gingival papillae and the entire gingival profile. Gingival parameters that have been recorded around completely intact teeth are used as initial criteria during the development of the pink esthetics parameter. With an adequate approach to the restoration of residual ridge defects, the doctor is also able to provide a more natural contour of the soft tissues in the peri-implant area, thus maximizing the overall success rate of the treatment.
Defects in the area of the bone structure of the jaws arise either due to the inability of bone tissue to regenerate normally, or as a result of progressive destruction. The inability to adequately form the bone structure is associated with two main factors: the congenital absence of teeth in a certain area of the alveolar ridge, which limits the conditions for the growth of alveolar bone tissue in principle, and the phenomenon of tooth ankylosis, which, in turn, stops the possibility of further growth of bone tissue. Destruction of the alveolar bone can develop due to infection of the intervention site, trauma or tooth loss. Infection of bone tissue can be caused by a tooth root fracture, errors during endodontic treatment, or pathologies of periodontitis or peri-implantitis.
If the size of the bone defect reaches critical values, such lesions are not amenable to spontaneous regeneration and require additional interventions. In such cases, they speak about the limited potential of ridge regeneration, and the need to implement hard tissue augmentation approaches. The problem is that the doctor, with large ridge defects, has to restore the contour of the ridge almost anew, taking into account all the necessary vertical and horizontal parameters. The predictability of bone augmentation procedures depends on the fact that a number of biological principles are implemented: wound closure under primary intention, ensuring sufficient blood supply, maintaining the required volume of space, and the stability of the regeneration process. A sufficient level of blood supply to the intervention area ensures the supply of necessary cells, growth factors and other agents that induce a cascade of osteogenic biomineralization. Osteocytes enter the wound area, differentiating from bone marrow stromal cells, as well as from progenitor cells that circulate in the blood. During angiogenesis, a new blood network of capillaries begins to form in the structure of the bone defect, which grow directly from the walls of the defect. The bone graft used during manipulation allows one to retain the required amount of space, initiates the process of tissue resorption during remodeling, and is a chemical attractant for angiogenesis. The success of bone augmentation depends on ensuring a closed state of the space under which tissue regeneration takes place, and the level of tissue vascularization in the area of intervention.
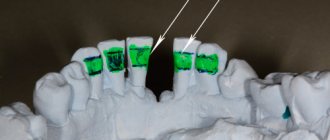
Restoration of horizontal bone defects is more predictable, since in such cases there are walls that limit the defect, from the structure of which capillary ingrowth will occur. When reconstructing vertical defects in the bone tissue of the jaws, the situation is somewhat different: the longer the distance over which the capillaries need to migrate, the more difficult it is to achieve complete vascularization of the bone defect (photo 1).
Photo 1. In the blood and bone marrow there are so-called differentiation clusters - CD34+ stem cells, which are capable of differentiating into osteoblasts and endothelial cells. These cells migrate to the affected area and initiate the process of its restoration by triggering a cascade process of formation of new bone tissue and blood vessels. In addition, CD34+ cells release vascular endothelial growth factor (VEGF).
Distraction osteogenesis is a modification of the guided bone regeneration (GBR) procedure and has demonstrated successful results in the restoration of complex bone crest defects. In fact, the movement of teeth during orthodontic treatment is also a variant of distraction osteogenesis. This procedure is also used during periodontal-orthodontic rehabilitation of patients in order to reduce the size of intraosseous defects around problem teeth. The use of distraction osteogenesis allows the clinician to reduce the initial size of the bone tissue defect, which subsequently simplifies the bone augmentation procedure. After all, the rule is the same for everyone: the smaller the bone defect, the easier it is to restore it. In the clinical case described below, we illustrate the concept of using orthodontic techniques during targeted correction of the area of future implantation.
Clinical case
A 28-year-old patient sought dental care with a complaint about implant mobility in the area of the 22nd tooth (photo 2-3). In the area of the 23rd tooth, the patient had congenital adentia. The 22nd tooth erupted in place 23, leaving free space in the area of the natural position 22, where the procedure for installing a dental implant was previously carried out. The implantation took place in December 2002. In February 2005, the patient went to the dentist with signs of implant mobility and symptoms of peri-implantitis. X-ray diagnostic data confirmed the destruction of the residual ridge area around the installed intraosseous support. During the treatment, the problematic implant was removed, and careful curettage was performed in the area of the formed defect (photo 4-5). During the healing process of the problem area, a defect in the jaw bone tissue was formed with loss of the level of clinical attachment in the projection of the distal surface of the 22nd tooth and the medial surface of the 21st tooth (photo 6-7). Thus, the bone loss in this clinical case was caused by both congenital adentia and the inflammatory effect of peri-implantitis. Considering the amount of bone loss in the area of teeth 21 and 22 adjacent to the defect, it was proposed to remove them and ensure adequate formation of the bone contour for the subsequent implantation procedure. This intervention required a massive guided bone regeneration procedure, for which bone graft could be harvested from the chin area. After 6 months, the edentulous area could be restored with a bridge or single crowns on implants.
Photo 2. Front view of the affected implant in the area of the 22nd tooth.
Photo 3. X-ray of the affected implant in the area of the 22nd tooth before treatment.
Photo 4. Vertical defect of the bone tissue of the ridge in the area of the 22nd tooth.
Photo 5. Horizontal defect of the bone tissue of the ridge in the area of the 22nd tooth.
Photo 6. View of the bone and soft tissue defect after removal of the implant.
Photo 7. X-ray of the defect area in the area of the 22nd tooth.
However, at the same time, such an approach is characterized by the risk of developing significant biological and aesthetic complications. To restore adequate gum contour, it was necessary to raise the level of the underlying bone tissue, only in this way would it be possible to achieve the proper height of the interdental papillae. This was the main problem, because the predictability of vertical augmentation surgery is less than that of horizontal reconstruction of the bone crest. In the process of vertical augmentation of the jaw bone, an autogenous graft in the form of blocks is successfully used, but the level of its effectiveness is determined by a number of factors, including ensuring primary wound closure, minimizing the risk of secondary infection, creating conditions for stabilizing the graft, and leveling the possibility of developing paresthesia after surgery. From an aesthetic point of view, the removal of two teeth and the placement of three implants means that it is quite difficult to achieve the proper height of the interdental papilla in the area between the three intraosseous structures. When using two implants, it is much easier to restore the proper papilla, however, in the area of the cantilever part of the prosthesis, it will be necessary to carry out certain periodontal intervention to correct the relationship of the prosthetic structure with the surrounding tissues. Thus, taking all of the above into account, the approach of natural tooth extraction and placement of three implants was categorized as excessively risky in terms of the potential for potential biological, aesthetic, biomechanical and occlusal complications.
Another possible treatment approach involved minimizing the length of the defect through orthodontic tooth movement. First we had to move the 22nd tooth into its proper position. In this way, it would be possible to limit the ridge defect to the volume of one tooth. After this, it was planned to carry out extrusion of 21 teeth (with further extraction), which would make it possible to “pull out” the level of the bone crest from the distal side of the defect. After this, 22 would need to be moved distally to the place of tooth 21, then forced orthodontic extrusion and subsequent extraction would also be carried out. Thus, it would be possible to reduce the size of the bone defect and form appropriate bone walls around it, from the area of which the process of angiogenesis would subsequently be ensured. The area of the defect at the site of tooth 21 could be restored using a mineralized lyophilized bone allograft and membrane. Orthodontic tooth movement, which, in essence, is a subtype of distraction osteogenesis, would allow the restoration of the proper vertical parameters of the height of the bone crest, eliminating the need for autogenous bone replacement material. In addition, correct positioning of the premolar during the orthodontic phase of treatment would allow the creation of a more harmonious occlusal scheme, ensuring the formation of an occlusal relationship protected by the premolars. Such a scheme ensures the normalization of the loads applied to the implant strictly along the axis of the intraosseous support.
After discussion, the second rehabilitation approach described above was chosen. Before the start of the orthodontic phase, soft tissue augmentation was performed in the area of teeth 21 and 22 to correct the mucogingival defect. For this purpose, a free gingival graft was used, which allowed the formation of the required thickness of attached and keratinized gums. Thus, we minimized the risk of developing loss of gingival coverage in the area of 21 and 22 teeth during their orthodontic movement (photo 8). The orthodontic phase of treatment was aimed at creating such a state of the bone ridge in the area of the 23rd tooth, which would be most suitable for the dental implantation procedure (photos 9-11). In addition, orthodontic correction made it possible to balance the patient's existing occlusal pattern. At the same time, in the area of individual teeth, their shape was corrected using composite restorations (photos 12-13).
Photo 8. View of sufficient volume of keratinized and attached tissue after soft tissue augmentation.
Photo 9. Orthodontic distraction osteogenesis to form a site for implantation in the area of the 23rd tooth.
Photo 10. Radiograph during orthodontic distraction osteogenesis.
Photo 11. X-ray after forming the area for implantation in the area of the 23rd tooth.
Photo 12. View of the formed occlusal relationship and canine route of insertion.
Photo 13. Bonding on teeth 7-9 after the orthodontic stage of treatment.
Photo 14. Registration of the presence of bone tissue in the interproximal areas of the 21st and 22nd teeth after orthodontic treatment.
After moving the 22nd tooth to its proper position, periodontal status was monitored. At this point, the decision was made to discontinue continuous extrusion of teeth 21 and 22 because there was a distinct difference in the levels of clinical mucosal attachment around these teeth (Figure 14). Thanks to the use of computed tomography and wax modeling capabilities, it was possible to establish the most prosthetically favorable position of the future implant. The results of the CT scan confirmed that the level of bone tissue was sufficient for the installation of an intraosseous support (photo 15-16). To correct residual signs of the bone defect, it was necessary to perform only a minimal procedure of directed bone regeneration. The implant was installed after complete separation of the flap (photo 17). During the operation, dehiscence was noted in the area of the roots of teeth 21, 22, 24 and 25, as well as signs of bone dehiscence in the area of the natural position of tooth 23 (photo 18). After installation of the implant, the cortical plate was perforated to induce the process of angiogenesis (photo 18).
Photo 15. Planning of implant installation in the area of the 23rd tooth according to CT scan data. Bone dehiscence in the area of the 23rd tooth was restored.
Photo 16. Cross-sectional view of the area of the 23rd tooth prepared for the installation of a dental implant after orthodontic correction.
Figure 17. SurgiGuide surgical template (Materialize Dental, Leuven, Belgium) supported on teeth.
Photo 18. Installation of a dental implant. Perforation of the cortical plate to stimulate angiogenesis.
To cover the area of dehiscence, a mineralized lyophilized bone allograft treated with platelet-derived growth factor was used, which was placed into the structure of the defect and covered with a membrane (Figure 19). The flap was repositioned more coronally to ensure complete primary wound healing (Figures 20-21). 4 months after implantation, provisional structures were fixed to the implants and the soft tissue area was augmented using a connective tissue graft. To complete the orthodontic correction of the teeth position, implant structures were used as additional support. The goal of orthodontic treatment at this stage was to achieve the required position of individual teeth, normalize their occlusal relationship and form an optimal distance between their roots. At the final stage of treatment, zirconium abutments (photo 22) and all-ceramic structures (photos 23-25) were fixed to the implants.
Figure 19: Mineralized freeze-dried bone allograft hydrated with platelet-derived growth factor was used to cover the area of dehiscence.
Photo 20. Closure of the wound area by primary intention.
Photo 21. X-ray of the implant in the area of the 23rd tooth immediately after installation.
Photo 22. Fixation of the zirconium abutment on the implant.
Photo 23. X-ray after fixation of the zirconium abutment.
Photo 24. Final restoration in the area of the 23rd tooth.
Photo 25. View of the final restorations in the area of teeth 7-9 and 23.
This clinical case illustrates an example of the correction of a dentoalveolar defect resulting from bone crest destruction through the application of the principles of orthodontic, periodontal and restorative dental treatment. This approach made it possible to normalize the patient’s occlusal scheme, as well as to achieve proper restoration of the defect area with minimal consumption of bone replacement materials. Thus, it was also possible to simulate the necessary contour of the soft tissues, ensuring their natural aesthetics. The restoration of the coronal part was carried out using all-ceramic single restorations on zirconium abutments.
Authors: Brian S. Vence, DDS George A. Mandelaris, DDS, MS David P. Forbes, DDS, PhD
Methods for treating alveolitis
Treatment for this disease should begin immediately after diagnosis. In most cases, a conservative treatment method is used, which includes taking antibiotics and non-steroidal anti-inflammatory drugs, as well as the use of antiseptics.
The antibiotic is selected so that its active substance penetrates the bones and soft tissues as quickly as possible. Only a doctor should select and prescribe such a drug, who can take into account the general condition of the patient and the presence of contraindications to the use of certain medications.
Nonsteroidal anti-inflammatory drugs are prescribed to relieve pain. Your doctor may prescribe ibuprofen, diclofenac, or another strong medication. Local anesthetics such as lidocaine and novocaine are often used to relieve pain.
Antiseptic agents are prescribed for rinsing the mouth to cleanse it, as well as rinse the hole. Antiseptics such as stomatidine, chlorhexidine, furatsilin and hexoral are suitable for these purposes.
In the conservative treatment of alveolitis that has developed after the extraction of a tooth, including a wisdom tooth, the hole is thoroughly washed and treated with antiseptics, and the source of infection is eliminated with the help of antibiotics. Surgical treatment of alveolitis is carried out in advanced cases. With this treatment, the infected area is cleared of pus and pieces of food, and layers of dead tissue are removed. The doctor also prescribes physiotherapeutic procedures, such as microwave therapy, the use of infrared laser or UV radiation.
It is impossible to treat alveolitis on your own. Due to the presence of pus in the socket, which the patient cannot efficiently eliminate at home, self-prescribing and taking antibiotics will only lead to a decrease in immunity. Rinsing with antiseptics can somewhat improve the overall situation, but they will not sufficiently clean the hole from pus and food debris. Traditional methods of treating alveolitis, which consist of using herbal infusions and decoctions, will not cause any harm to this disease, but they will not provide any benefit either.
The duration of treatment for alveolitis depends on the form of the disease and its neglect. It may take from 2 days to 2 weeks to stabilize the patient’s condition, stop the spread of infection and cleanse the hole.
Treatment of alveolar sockets
Treatment is carried out strictly by a dentist. Remember that when treating alveolitis yourself with rinsing and antibiotics, you will not get rid of it, all these measures are useless! The main treatment procedure can only be performed by a dentist. Treatment at the dentist goes something like this:
- Removal of the blood clot under anesthesia, removal of food debris and necrosis from the socket (if all this is not removed, any treatment will be null);
- The hole is disinfected and washed with an antiseptic; antiseptics are placed in it, which are changed from time to time by the dentist at separate appointments;
- The dentist will prescribe antiseptic baths and an antibiotic, and painkillers for pain;
Moscow metro station Zvezdnaya, Danube Avenue, 23
Prevention of alveolitis
In order to prevent alveolitis, it is recommended to follow these simple rules after tooth extraction surgery:
- no smoking;
- Do not rinse your mouth during the first day after surgery;
- do not eat foods that require some effort when chewing, and do not eat spicy or hot foods;
- do not touch the hole remaining after tooth extraction with your tongue or fingers;
- do not visit the sauna for some time and avoid increased physical activity.
If you experience any discomfort in the socket area after tooth extraction, you should consult a doctor as soon as possible. In the early stages, alveolitis can be treated quickly, and the treatment itself is inexpensive.
The Denta-Professional dental clinic employs experienced doctors who qualitatively treat alveolitis using modern medicines and procedures. They carry out their job duties professionally, so the success of treatment is guaranteed even in the most difficult cases.