It often happens that we injure moles. Rip off completely or slightly tear off from the skin. It happens that the bleeding is quite strong, but it is still possible to stop it. Here the mole is covered with a band-aid and everything seems to be fine. Here we remember that in childhood our mother told us: “Don’t pick at a mole - you can die from it.” With an unpleasant feeling somewhere in the upper abdomen, we begin to search on the Internet for the eternal answer to the question “What to do?” After half an hour or an hour we understand that in a couple of days death from melanoma will occur and it’s time to look for a place in the cemetery...
Later in this article I will try to interrupt the endless stream of hysteria that has been copied from site to site for many years
Sign up for the webinar “Carcinogens in cosmetics: truth, lies and... marketing”
Is mole injury really dangerous?
In RuNet, the danger of traumatizing moles is given excessive, in my opinion, importance. Is there any justification for this point of view? Absolutely, but I think it's quite shaky.
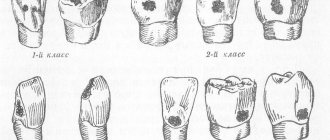
Indeed, there are several studies on this issue, mostly conducted in the 60s–80s of the last century. They show that 30–50% of patients in whom melanoma developed against the background of a nevus noted single or repeated trauma to the mole.
There are several arguments against these studies:
- Just because melanoma develops after trauma to a nevus does not necessarily mean that the two are related. Melanoma could develop both before trauma and much later for other reasons .
- A 2010 meta-analysis (summarizing data from 9 studies) showed that performing an incisional biopsy does not affect the prognosis of melanoma. In other words, if a piece is cut off from melanoma (for diagnostic purposes), this will not negatively affect the patient’s chances of living 5 years or more.
- The conclusions of the authors of several studies (55, 115, 147 and 498 patients) agree on one thing - incomplete removal of nevi, except for dysplastic ones with severe dysplasia, does not lead to the development of melanoma.
Here the corrosive reader will say: “Aha! Still, incomplete removal (you can read “trauma”) causes the development of melanoma!” No. A dysplastic nevus with severe dysplasia itself has a high chance of becoming melanoma in the future. The connection between incomplete removal and the development of melanoma from such nevi has not been proven .
- My experience. Almost every day people write to me who have injured a mole and are now preparing to “die” because they have read too much on the Internet. Almost any person who has a mole protruding above the skin has injured it in one way or another at least once in their life. If trauma to a mole were really a risk factor, in our country with a population of 146,000,000, the diagnosis of melanoma would be made much more often than 8,000 times a year.
Adverse reactions
A concentrated antiseptic solution provokes allergic reactions. Incorrect dosage calculation and abuse of a disinfectant leads to the following consequences:
- redness;
- dryness;
- skin stickiness;
- salivation;
- taste disturbances;
- skin rashes;
- contact dermatitis.
In 96% of cases, adverse reactions disappear after discontinuation of the drug.
Do not use a 20% antiseptic to disinfect open wounds. This is fraught with a chemical burn and worsening the condition of the burned skin.
Accidental ingestion of the medicine leads to poisoning and diarrhea.
What will happen to the mole next?
After trauma, as in any other place, the mole will hurt a little and turn slightly red - this is normal. Gradually, after 2-3 weeks, these phenomena should go away on their own. The only situation in which medical intervention may be required is the suppuration of a mole after a severe injury. This means that if after a few days a viscous white (not yellow) liquid begins to come out from the site of injury, you need to be examined by a surgeon. After 1-2 days, a crust will appear at the site of the injury, which will fall off on its own after 1-2 weeks.
Urethral lavage during self-medication
Washing the urethra at home is possible no further than its anterior segment. Therefore, doing instillations for medicinal purposes on your own is not only pointless, but also dangerous. No amount of rinsing the urethra with potassium permanganate or even miramistin can cope with the inflammatory process in the posterior parts of the canal. No matter how proven the solution may be, washing the urethra on your own is unlikely to be able to push it beyond the first six to seven centimeters. This means that the posterior segment of the urethra will be infected. And then bacterial, viral, protozoal agents can easily begin to travel through the genitals and blood, causing prostatitis, vesiculitis, orchiepididymitis or visceral lesions. It is also worth remembering that the same chlorhexidine or miramistin are absolutely indifferent to such STI pathogens as chlamydia. The latter are quite resistant to instillations and can tolerate unfavorable conditions, forming foci of chronic infection. It makes no sense to try to independently administer potassium permanganate or furatsilin in order to treat urethritis. This only creates the illusion of activity in the patient, threatening to transfer him to the category of traumatic patients with burns or canal injuries.
How to properly monitor a mole after an injury?
To objectively track changes in a mole, after the inflammation has subsided, you can take a photograph of it against the background of a ruler and compare the original image with subsequent ones. In order for the photo to be of high quality and comparison possible, the following rules must be observed:
- The photo must be taken with a camera, not a phone.
- The photo should not be a “selfie”. In such photographs, the mole is usually out of focus.
- A light source or camera flash should be directed at the mole.
Is it possible to treat a burn with Chlorhexidine?
When using Chlorhexidine for burns, you should pay attention to the concentration of the active ingredient in it - chlorhexidine bigluconate. For local and external use, 0.05%, 0.2% and 0.5% antiseptics are suitable. More concentrated products are intended for disinfection of medical instruments or undamaged skin.
This effective antiseptic destroys up to 80% of pathogenic fungi and bacteria. It is used in the form:
- applications;
- rinsing;
- irrigation;
- rinsing.
The drug prevents wound infection and purulent inflammation of wound surfaces.
Briefly about the main thing:
In my opinion, there is currently no convincing evidence that trauma to a mole can lead to the development of melanoma. Besides me, oncology associations such as NCCN and ESMO also think the same. However, I don’t know if everything was fine with your mole BEFORE the injury. That is why, after the inflammation has subsided, I recommend contacting an oncologist, especially if this specialist has not looked at all of your moles before. If pain, redness, and swelling do not go away within a month, you need to see an oncologist as quickly as possible.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My Online consultation (from anywhere in the world)
In what cases is the use of antiseptics prohibited?
Chlorhexidine is not used in case of hypersensitivity to the active or auxiliary components. Contraindications to its use are:
- exacerbation of dermatitis;
- tendency to allergies;
- parallel intake of iodine preparations;
- 3rd and 4th degree burns;
- relapses of herpes zoster.
Use the medicine with caution to treat burns in patients under 16 years of age. Children's skin is prone to allergic reactions, so treating wound surfaces with 0.5% antiseptic is fraught with nettle fever.
Preparations for lavage of the urethra
Microorganisms such as chlamydia exhibit the properties of a virus and bacteria at the same time, being an intracellular parasite. Therefore, after chlamydia has been introduced into the endothelium of the urogenital tract, it is not so easy to get them out of there. And they are not susceptible to antibiotics of many classes. This is where rinsing the urethra with collargol comes to the aid of the urologist. A 2% solution containing silver and protective protein is administered by the doctor during the appointment. For this purpose, a 40-cm Nelaton catheter is used. It is sterile and disposable, made of plastic that does not cause allergies and irritation of the mucous membrane. A 150 mm disposable syringe is also used, into which the solution is drawn and which creates the necessary pressure for its administration. Other drug options for the procedure may be: protargol, combinations of dioxidine and protargol, dimexide and dioxidine. The drugs have a local antiseptic effect plus have an exfoliating effect. Helping to get rid of cells affected by intracellular pathogens or bacterial film. Washing with protargol or collargol is effective for trichomoniasis, gonorrhea, mycoplasmosis. Washing the urethra with Uro-Hyal is more often used for combined pathologies of the urinary tract. Persistent interstitial cystitis in combination with urethral lesions may require such a drug. With this development of events, both the urethra and the bladder are washed.
- Collargol - a 2% solution of silver on glycerin - is used for a wide range of infections. It inhibits the growth of bacterial agents, viruses, and protozoa. Highly efficient;
- Silver proteinate or colloidal silver is known as protargol. The aqueous solution is characterized by antiseptic, astringent and anti-inflammatory properties. The effect is based on the binding of silver ions to the genetic material of pathogens. Rinsing the urethra with protargol allows you to create a protective film instead of exfoliated endothelium (due to the precipitation of proteins by silver). These two drugs are the main antiseptics, which are extremely safe and widely active;
- dimexide or dimethyl sulfoxide exhibits anti-inflammatory and analgesic effects. Penetrates biological membranes and improves the penetration of other substances into endothelial cells. Therefore, they use it in combination with silver preparations (collargol and protargol). It is used more rarely on its own;
- dioxidine - hydroxymethyl quinoxaline. Its solutions exhibit broad bactericidal activity. One of the advantages is the absence of irritation of mucous membranes and skin. More often a one percent solution is used. Suitable for joint use with dimexide.
The answer to this question is quite expected. This is only part of a set of measures to get rid of inflammation of the urethra due to sexually transmitted infections. There is no point in using it every day. 2-3 procedures per week are enough. This will make the instillations as beneficial as possible and will avoid side effects and complications. This frequency of procedures allows the urethra to fully recover.
- inexpensive;
- does not require the use of reusable instruments;
- allows you to overcome antibiotic resistance of bacterial films;
- allows you to shorten the time and cost of treatment;
- makes it possible to treat chronic, persistently recurrent inflammatory changes;
- combines the advantages of preventive and therapeutic methods;
- allows you to avoid multiple courses of antibiotics and prevents the development of bacteria with multiple resistance to antimicrobial drugs.
Is it painful to wash the urethra?
An experienced urologist performs such procedures not only correctly, but quickly and painlessly. After all, he has skills in his hands that have been developed over the years. The instillation regimen must be chosen correctly, and the patient is not allergic to the selected solution. A slight burning sensation after washing the urethra, caused more by damage to the mucous membrane by the main inflammatory process, is all that he can feel. This is a clear advantage of a catheter in the hands of a professional. Even after using all the tools and materials, a person without experience can not only scratch, but even more roughly violate the integrity of the urethra. Causing not only pain, but also bleeding. It is better for the patient to urinate before the procedure. After all, after administering the medicine, it is recommended to delay urination for half an hour to an hour. Before inserting the catheter, the doctor treats the head and external opening of the urethra with an antiseptic. After this, a sterile catheter is inserted into the urethra. Its free end is attached to a disposable syringe containing medication, which is slowly injected into the urethra. Next, the catheter is removed. No pain relief is required during or after the procedure. It should be remembered that you should immediately report any painful reactions or allergic manifestations during procedures or medications to your doctor. Also, you should not conceal episodes of allergies or other drug intolerances that have been noted previously. This will allow the patient to achieve maximum safety, and the doctor to choose the most gentle and correct treatment regimen. If discomfort or allergies appear after independent home manipulations, it makes sense to immediately seek advice from a urologist. The same recommendations apply to canal injuries. Thus, if you need to wash the urethra for therapeutic purposes, it is advisable to contact a venereologist or urologist. It is better to do this in a clinic equipped with a laboratory, so as not to delay either competent diagnosis or effective treatment.
Consequences of self-washing the urethra
Complications of washing the urethra at home on your own can be very diverse:
- burns of the mucous membrane up to the formation of strictures (narrowings) of the urethra, complicating urination;
- the spread of infectious agents up to the generalization of the infection; the formation of carriers of the infection;
- erectile dysfunction;
- infertility;
- urethral injuries and bleeding from it.
The consequences of a thoughtless attitude to the use of medications are subsequently much more expensive than high-quality treatment from a competent specialist.