Antibiotics are a group of medicines aimed at combating pathogenic bacteria. Once in the body, they suppress the growth of pathogenic flora and help eliminate infectious and inflammatory diseases. It is difficult to imagine the life of a modern person without antibiotics - they are widely used for bacterial complications of respiratory viral infections and exacerbations of chronic inflammatory diseases of internal organs, and can be used for preventive purposes after surgical interventions.
Despite the benefits of these drugs, their use does not go without a trace, because the active substances destroy not only pathogenic flora, but also beneficial bacteria. Dysbacteriosis occurs - an imbalance of microorganisms, which can cause damage to the digestive system. Poisoning and discomfort in the stomach while taking antibiotics are associated with a decrease in the volume of beneficial microflora, as a result of which opportunistic bacteria are activated. Often this condition is accompanied by symptoms of intoxication, especially diarrhea.
Why does diarrhea occur after taking antibiotics?
The development of complications during antibacterial therapy in the form of diarrhea is associated with a decrease in beneficial microflora, which is involved in a complex of digestive processes:
- breakdown and absorption of nutrients from food;
- evacuation of the contents of the stomach and intestines;
- residual digestion of food;
- removal of toxins and metabolic products;
- secretion and absorption of water in the intestine;
- formation of feces, regulation of their excretion.
Even with standard antibacterial therapy, leading to a slight imbalance, side effects may occur in the form of disruption of intestinal function.
In addition, bacterial infections themselves can contribute to diarrhea, which is the basis for taking antibiotics. The waste products of pathogenic bacteria have a toxic effect, and stool liquefaction may be associated with an increase in body temperature. Antibiotics fight the underlying agent and root cause of the disease, and in many cases they are truly necessary. However, this group of medications can worsen the digestive system.
The mechanism of development of diarrhea after a course of antibiotics
Antibiotic-associated diarrhea (AAD) develops as a result of the death of both pathogenic bacteria and beneficial microorganisms. An imbalance of microflora is called dysbiosis. According to statistics, the source of such digestive disorders can be up to ⅕ of the types of antibiotics used in medical practice. Typically, this phenomenon occurs as a result of taking broad-spectrum drugs.
Typically, this type of diarrhea does not have other symptoms, unlike food poisoning. The main symptoms of antibiotic poisoning include watery or loose stools, and less commonly, cramping abdominal pain. Most often, the intestinal condition returns to normal after 2-3 days.
In very rare cases, antibacterial therapy can cause colonization of the mucous membranes by pathogenic microorganisms - Clostridium difficile and Salmonella. They cause severe infections with persistent diarrhea, which increases the risk of dehydration and can lead to serious health consequences.
Antibiotic-associated diarrhea can occur with long-term use of suitable doses of the drug, and not necessarily in tablet form - injections can also lead to this result. However, poisoning can also occur due to an overdose. Each antibiotic has a toxic effect on different organs, so the category of the drug is taken into account. Common symptoms of overdose include the following:
- high body temperature (up to 39–40 ˚C);
- diarrhea;
- vomit;
- muscle pain;
- pain in the right hypochondrium;
- changes in blood pressure;
- tachycardia or bradycardia;
- joint pain;
- dizziness, etc.
With toxic damage to the liver, the following symptoms may appear: yellowness of the skin and sclera, itching of the skin, bloating, etc. With kidney damage, the volume of urine decreases significantly, and a strong feeling of thirst occurs. Poisoning with aminoglycosides leads to the appearance of signs of toxic otitis: acute pain in the ears, decreased hearing acuity, a feeling of congestion, etc. All conditions associated with an overdose of antibiotics require immediate treatment of poisoning . It is important to call an ambulance as soon as possible.
Signs and symptoms of candidal stomatitis
Patients who develop fungal stomatitis or thrush in the mouth usually complain of pain and discomfort when eating or drinking liquid drinks, impaired taste, difficulty swallowing, and pain, discomfort, constant itching in the mouth, bad breath are also possible in state of rest. Swelling of the cervical lymph nodes is possible, and small children even refuse to drink. The oral mucosa and tongue are covered with a whitish coating, sometimes with a characteristic sign: bleeding appears when the plaque is removed. When thrush spreads to the corners of the mouth, difficulties appear in opening it (the so-called candidiasis).
The initial diagnosis of candidiasis, fungal stomatitis is especially difficult in young children, since at the primary stage only redness is detected, and there is no characteristic plaque. But then whitish small grains appear (resembling semolina grains), which, after increasing in size, take the form of a film or curdled residue. In the absence of treatment for candidal stomatitis, it can progress, plaque covers the entire surface of the oral cavity, the internal layers of the mucous membrane are also affected (acute thrush in the mouth), and with certain predisposing factors, chronic candidal stomatitis .
Treatment of antibiotic-associated diarrhea
Diarrhea that develops while taking antibiotics requires adjustment of the treatment regimen. You should not stop taking medications on your own; you should consult your doctor. Typically, the course of antibacterial therapy is interrupted or the drug is replaced with an antibiotic of a different group.
Normalization of digestive processes, intestinal motility and stool consistency are tasks that require an integrated approach. There are three general principles that are important for all people suffering from diarrhea after taking antibiotics:
- Nutrition correction: it is important to follow a diet. The diet should include crackers and rice water. It is important to reduce the amount of carbohydrates consumed as much as possible, and also give up milk, dairy products, baked goods, fresh vegetables, berries and fruits; legumes, pasta.
- Compliance with the drinking regime: it is necessary to drink at least 2 liters of water per day to replenish fluid loss during watery stools.
- Symptomatic therapy: the pathological process can be stopped with the help of medications.
Due to the fact that many sources of natural probiotics and prebiotics are prohibited for diarrhea, one of the key principles of treatment is the prescription of medications containing these components. Strict dietary restrictions require the use of probiotics and prebiotics for antibiotic-associated diarrhea: it is important to restore normal intestinal microflora to prevent the proliferation of opportunistic microorganisms.
In most cases, medication correction is indispensable. Remember that only a doctor can prescribe medications.
There are several groups of drugs that can be recommended for antibiotic-associated diarrhea.
Sorbents
Infectious and inflammatory diseases are accompanied by intoxication of the body, and in the process of antibacterial therapy, decay products of pathogenic microflora accumulate. Therefore, the doctor may prescribe enterosorbents - products that literally absorb toxins and harmful substances and remove them from the body.
Probiotics and prebiotics
It is important to address the root cause of diarrhea and restore normal intestinal microflora after taking antibiotics. For this, probiotics are used - bifidobacteria, lactobacilli, as well as prebiotics - a nutrient substrate to stimulate the growth of one's own beneficial microflora. Synbiotics include both probiotics and prebiotics and are widely used in gastroenterological practice.
If there is a pronounced shift in the microbial balance, the doctor may recommend intestinal antiseptics or bacteriophages - they are designed to prevent the growth of opportunistic microflora and help restore the number of beneficial microorganisms.
Enzymes
Enzyme replacement therapy is not the mainstay of treatment for antibiotic poisoning. However, preparations based on digestive (pancreatic, gastric, intestinal) enzymes stimulate the digestion of food, normalize intestinal motility and peristalsis and participate in the restoration of normal microflora of the large intestine.
Symptomatic therapy
Diarrhea is often accompanied by painful symptoms: flatulence, nausea, cramping and abdominal pain. You can quickly alleviate the condition with the help of medications. They are unable to cope with the main problem, but will bring temporary relief. Report your symptoms to your doctor, and he will select one or more remedies to improve your well-being:
- for increased gas formation - defoamers (drugs based on simethicone) or herbal carminatives;
- analgesics or antispasmodics for pain;
- Oral rehydration solutions are products designed to replenish normal fluid volume and prevent dehydration.
If diarrhea is accompanied by elevated body temperature, the doctor will select an antipyretic drug.
General strengthening agents
Weakened by an infectious or inflammatory disease, as well as subsequent use of antibiotics, the body may require complex recovery. A specialist can prescribe immunomodulators, vitamin-mineral complexes and restorative drugs.
Restrictions in food during diarrhea can also cause hypovitaminosis and lack of minerals. During long-term antibiotic therapy, it is necessary to discuss preventive measures with your doctor in advance.
Antidiarrheal drugs
If you cannot cope with diarrhea, your doctor may prescribe drugs from the following groups:
- eubiotics - live bacteria that are designed to restore the balance of intestinal microflora and restore normal digestive function;
- synthetic drugs based on loperamide: bind to opioid receptors of the intestinal wall and inhibit the release of mediators that stimulate intestinal motility;
- herbal preparations based on tannins.
Sorbents also have an antidiarrheal effect. They are natural and synthetic. Enterosorbents, entering the intestines, absorb toxins and harmful substances, contribute to the formation of stools and their reduction. It is important to remember that at least two hours should pass between taking sorbents and other drugs.
For severe antibiotic-associated diarrhea, antibacterial agents targeting Clostridium difficile or another infectious agent may be appropriate.
The drug “Fitomucil Sorbent Forte” can be used as an adjunct to relieve diarrhea syndrome. It contains inulin, a prebiotic that promotes the growth of normal microflora, as well as 5 types of probiotic bacteria. In addition, the drug contains psyllium, a natural component that helps reduce diarrhea and relieve intoxication, since it turns into a gel and absorbs toxins. The triple effect (enterosorbing, detoxifying and restorative) distinguishes Fitomucil Sorbent Forte from other sorbents prescribed for AAD. Live bacteria populate the intestines and not only help relieve diarrhea, but also improve the condition of the microflora that has been damaged by taking antibiotics.
However, to restore microflora it is not enough to take one drug.
Only a doctor prescribes specific therapy. It is necessary to stop taking uncontrolled medications and agree with a specialist on medications for symptomatic therapy.
What it is
In the process of studying the contents of stomatitis ulcers, scientists have repeatedly discovered the presence of pathogenic bacteria in the liquid. Based on this, a version emerged about the possible formation of stomatitis as a result of bacteria entering microscopic wounds and cracks in the oral cavity. The most common “guests” that affect the mucous membrane are the ubiquitous streptococci and staphylococci. These bacteria are present everywhere, and even a newborn baby in the maternity hospital can pick them up. That is why bacterial stomatitis is recognized as one of the main types of stomatitis in children.
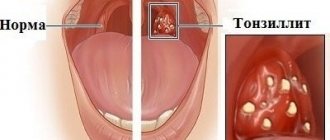
This type of bacteria constantly lives in a weakened body, especially with chronic diseases of the teeth (deep caries, gingivitis, periodontitis), tonsils (tonsillitis) or nasopharynx (laryngitis, pharyngitis, rhinitis). If the integrity of the mucous membranes is not compromised, there is no reason to fear stomatitis, however, the slightest injury inevitably leads to bacteria entering the damaged area.
However, bacteria often enter the wound from outside. The inflammatory process can begin on the skin of the face or in the corners of the lips and smoothly flow into the oral cavity if left untreated. The infection can also be acquired during dental treatment, by eating unwashed foods, and even by kissing a sick person. In such cases, only streptococci are most often present in the lesions at the initial stage, and staphylococci also appear later.
The list is not limited to these two bacteria, since diplococci, spirochetes, spindle-shaped bacteria, gonococci, clostridia and other dangerous types of bacteria can cause no less harm to the oral cavity.
Depending on the general condition and immune response of the body, bacterial stomatitis can be short-term, or it can drag on for a long time, turning into a severe necrotic form. With this scenario, a pronounced dark swelling is detected at the site of damage, and subsequently bubbles appear. This course of the disease in weakened people is accompanied by fever, general malaise, headaches, intoxication of the body and even the development of a severe form of sepsis. Often, with bacterial stomatitis, there is pronounced bleeding of the gums.
Prevention of diarrhea during antibiotic therapy
To prevent diarrhea while taking antibiotics, it is important to follow several recommendations:
- strictly adhere to the dosage and treatment regimen prescribed by the doctor;
- use probiotics recommended by a specialist;
- follow a diet to prevent gastrointestinal disorders;
- maintain optimal drinking regime;
- take medications that protect the lining of the stomach and the entire digestive tract. If you have chronic ailments, you must inform your doctor about them so that he can select an individual scheme for protecting the digestive system from the effects of antibiotics.
If it is necessary to take antibiotics, it is important to take into account the body's previous reactions to antibacterial therapy. Thus, in some patients, antibiotic-associated diarrhea develops in response to exposure to a particular group of drugs or a specific agent.