Hyperplastic gum growth is a fairly pressing problem in dentistry that requires timely professional treatment. This condition not only spoils the appearance of the teeth, but also causes discomfort and can become complicated. gum hypertrophy develops, it is recommended to immediately consult a dentist. The Nurimed clinic in St. Petersburg offers its services for the diagnosis and treatment of overgrown periodontal tissue.
Dental hypoplasia
It affects the enamel of the teeth and, as a result, underdevelopment of the tooth or its tissues. It is a fairly common dental disease and is observed in approximately 30% of patients. A weak degree of enamel underdevelopment is manifested by a change in color in the form of pronounced pigmentation of white or yellow shades without any unpleasant sensations. Small single spots may not be treated, but if the spots are visible to the naked eye, for example during communication, treatment is mandatory!, and as soon as possible, since inaction can cause the most irreversible consequences. Such as:
- Increased tooth wear
- Destruction of tooth tissue
- Complete loss of affected teeth
- Development of malocclusions
A popular and effective treatment method is dental restoration, and in case of serious changes, orthopedic treatment is indicated. In some cases, tooth enamel may be prepared to smooth the surface of the teeth.
Manifestations of the disease
The following clinical symptoms allow you to recognize gum fibromatosis:
- In the initial stages, swelling or enlargement of tissue of a tumor nature.
- On the mucous membrane you can see thickenings that gradually increase.
- Increased gum volume without signs of swelling.
- Filling interdental spaces with soft tissue.
- Overlapping of the teeth with the edges of the gums.
- Injury to overgrown areas during cleaning (this can cause bleeding and inflammation).
- Increasing intensity of tissue color (the gums become bright pink).
If you notice any signs of fibromatosis, you should immediately contact your dentist. If you ignore the problem, unpleasant complications may develop:
- decreased quality of daily hygiene with an increased risk of developing infections;
- pain when eating;
- redistribution of chewing load;
- development of periodontal diseases.
Dental hyperplasia
Manifests itself in the form of excessive formations of hard dental tissues. In 70% of cases the disease is acquired, in the rest it is hereditary. An example of dentin and enamel hyperplasia are oval-shaped formations, measuring from 0.5 to 3.5 mm diagonally, consisting of either enamel or dentin covered with enamel. There are cases in which the cavities of such formations were filled with pulp. They can be located almost anywhere on the tooth. This dental disease occurs in 2-3% of the population. Identifying this disease and 3-5 visits to the dentist will allow you to get rid of it for life, .. or for a long period of time, if after treatment you stop visiting the dentist again.
Treatment of hyperplasia
Therapeutic treatment, in which grinding of enamel drops and filling of pinpoint manifestations of the disease are prescribed. In children, treatment of hyperplasia is carried out using a restorative method.
To restore teeth, photopolymers are used, which completely restore the structure and color of the enamel.
Veneers are installed or artificial crowns are made. Of all types of hyperplasia, only pearl drops on the neck of the tooth can be cured, which over time can cause inflammation of the gums. During the treatment process, excess enamel is removed from the tooth using diamond grinding, and a course of phosphorus-containing medications is prescribed.
Dental fluorosis
Dental disease that occurs when drinking water and food with a high fluoride content, and in large cities and during the usual inhalation of combustion products (exhaust gases from cars, factories, etc.). It is one of the most common non-carious diseases affecting tooth enamel. One of the reasons for the appearance is the entry of fluoride elements into the blood and manifests itself in the form of stains on the tooth, of different sizes, shapes and colors. The disease usually destroys the incisors. When treating the disease, professional whitening is used, or restoration of the damaged part of the tooth with a composite material or an onlay (orthopedic design).
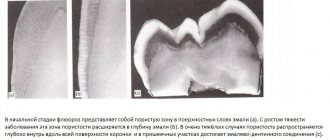
Fluorosis
A non-carious lesion that develops as a result of large doses of fluoride compounds entering the body. As a rule, we are talking about a cumulative effect - a microelement enters the body over a long time before causing pathological changes in hard tissues, not only tooth enamel and dentin, but also bones. Even slightly exceeding the level of fluoride in drinking water can be fatal for people with calcium deficiency, especially for children during the formation of the skeleton and molars (baby teeth are rarely affected by fluorosis). There are several forms of the disease, differing in the shape of the spots and the degree of tooth decay. Thus, streaked, spotted and chalky-speckled forms are characterized by the appearance of white stripes, yellowish, brown and dark brown spots on the enamel, and erosive and destructive forms are accompanied by deep lesions of hard tissues, leading to tooth destruction.
Causes of fluorosis:
- consumption of water containing fluoride more than 1.5 mg (6.0 mg is a critical indicator leading to pathological changes) The optimal concentration of fluoride, which has a pronounced preventive effect on teeth: 0.6 - 1.5 mg/l.;
- work in production in conditions of excess fluoride in the air;
- lack of calcium with excess fluoride.
Symptoms of fluorosis
Teeth become brittle, their enamel wears off, and dark brown (brown) stains appear, which over time turn into erosions. The non-carious nature of the disease is confirmed by the fact that other hard tissues of the body also suffer from it, as evidenced by bone pain and decreased joint mobility. The development of fluorosis is often indicated by muscle weakness, as well as disturbances in the functioning of the liver and autonomic nervous system.
Treatment of dental fluorosis
First of all, you need to eliminate the source of excess fluoride intake - change the water and working conditions, and then begin to put your teeth in order. Treatment is determined by the form of fluorosis - sometimes, in order to return the teeth to an aesthetic appearance (in some cases after grinding off the enamel), it is enough to carry out bleaching and remineralization with preparations enriched with phosphorus and calcium, and if the process has gone deep, the teeth are restored with crowns or veneers. By the way, residents of Russia more often suffer from a lack of fluoride in water than from its excess. But it is better to find out exactly the microelement content in the water you drink, and not to use fluoride-containing toothpastes and mouth rinses if there is enough fluoride in it.
In tap water in St. Petersburg, the fluorine content is 0.15 - 0.20 mg/l of water, which is significantly lower than the optimal level.
Pathological abrasion of teeth
Characterized by severe loss of hard tissue on all teeth. Traditionally, three types of abrasion are distinguished: horizontal, vertical (extremely rare) and mixed. In this case, tissue loss occurs either in the horizontal plane, then the cutting edges of the teeth, cusps and chewing ones are erased. There are several subtypes of increased abrasion and they depend on the depth of the tissues involved in the process and the diminishing tissues. Often this disease is promoted by: traumatic occlusion, bruxism and frequent chewing of very hard foods. Minor abrasion of two or more teeth is a consequence of increased, systematic load on the teeth. If you have teeth worn down by time? If yes, then you definitely need two dentists, an orthopedist and an orthodontist, since it is impossible to get rid of tooth wear without a dentist. I would like to note that solving this disease is not the cheapest pleasure, which means installing braces at a young age will allow you to maintain healthy teeth and a very significant budget.
How to diagnose and how to treat gum hyperplasia?
The diagnostic algorithm is focused on not confusing the disease with other pathologies. Therefore, the examination should be trusted only to a qualified dentist. The Nurimed Clinic offers a modern algorithm for confirming hypertrophy:
- examination of the oral cavity (allows the doctor to suspect a problem);
- X-ray examination to exclude similar pathologies;
- histological analysis of tissues taken for biopsy (a conclusion on the benign quality of the process and cellular composition is required).
After confirmation of the diagnosis, which is impossible without histology, treatment of gingival hyperplasia is carried out. Modern dentistry offers safe, painless surgical removal of overgrown gum tissue. The dentist peels off and removes excess tissue, after which the mucous membrane is sutured. This procedure is considered minimally invasive and does not require special recovery. In some cases, the dentist prescribes a number of medications to prevent complications.
An additional stage of treatment is sanitation of the oral cavity. Manipulation allows you to eliminate infectious processes that could cause hyperplasia. Also, professional cleansing can reduce the risk of inflammation and relapse of hypertrophy.
In the case of drug-induced fibromatosis, it is recommended to consult with your doctor and, if possible, change medications. To prevent re-growth, the cause of hypertrophy must be eliminated: the bite is corrected, tartar is removed, inflammation is treated, the balance of hormones is controlled, and so on.
Wedge-shaped tooth defect
Non-carious lesion of the hard tissues of teeth, manifested in the form of a formation in the area of the neck of the tooth. Non-carious lesion of teeth, observed in the form of a wedge-shaped defect. The diagnosis is observed in the front teeth (smile area). Outwardly it appears in the shape of a “ladder” (hence the “wedge-shaped defect”). Symptoms of the disease manifest themselves in the form of a medium defect in the enamel and up to the complete chipping of part of the tooth. The painful anomaly most often appears in people aged 35 to 65 years. Treatment of this pathology is possible, but it is necessary to identify the nature of the disease accompanying the appearance of such a lesion.
- Is there a risk of tooth fracture?
- Is there a risk of developing pulpitis?
- Is the patient embarrassed by his appearance?
- Is there sensitivity?
- Is the patient concerned about further progression of the lesion?
Only by collecting all the answers to the questions can the orthopedic dentist make a final diagnosis and offer several methods of dental treatment. But in any case, you need dental intervention. Inaction with such a tooth defect can lead not only to its loss, but also to a number of symptoms not related to teeth, for example, insomnia.
Types of gum hyperplasia
In dentistry, the following types of fibromatosis are distinguished:
- Localized hyperplasia (tissue near one tooth or group of teeth is affected).
- Generalized (the entire dentition of one or both jaws overlaps).
- Papillary (growth is concentrated only in the area of the papillary papilla).
- Marginal (not only the papilla is affected, but also the gingival margin).
- Diffuse (increase in all layers and areas of tissue).
In some cases, hypertrophy appears as a bump or growth when the growth affects a limited area.
Increased tooth sensitivity
In dental language - Hyperesthesia. If you feel a sharp pain lasting 5-20 seconds, then be sure that this diagnosis has reached your teeth. The disease manifests itself in the form of sensitivity of one or more teeth, or is generalized, affecting almost all teeth.) There are several types of hypersensitivity
- reaction to hot and cold.
- reaction to sugar, salt and acids.
- reaction to everything, including tactile stimulation.
Hyperesthesia almost always leads to many other dental diseases. Sensitivity between teeth is a symptom of the development of dental caries. There are many reasons for sensitivity, but the main ones are:
- Carious process
- Tooth wear
- Enamel chipping
- Wedge-shaped defect
- Hypoplasia
- Erosion of tooth enamel
Note that this disease is a direct consequence of loss of tooth integrity. Treatment of the disease depends on the causes of its occurrence (caries - filling; chipping of enamel - tooth restoration, etc.)
Non-carious lesions of teeth
In addition to caries, the most common dental disease, there is another diverse pathology of hard tissues - non-carious lesions of teeth.
Non-carious lesions of dental tissue occur without tissue softening and without the participation of microorganisms. These processes are based on a violation of the mineralization of hard dental tissues under the influence of external or internal factors. These pathologies occur in approximately 15% of patients, but no more than 5% seek dental care for them, since non-carious dental lesions, as a rule, do not cause pain or other subjective sensations, and often only worsen the appearance. However, if left untreated, a number of complications may occur, in particular early tooth loss.
Hypoplasia of teeth and enamel is most often the underdevelopment of enamel or tooth tissue in the tooth buds under the influence of disturbances in mineral and protein metabolism in the body of the fetus in the womb or in the body of a child. The enamel immediately after eruption has a chalky tint, and then becomes loose and is quickly lost. Hypoplasia is irreversible. Hypoplasia of permanent teeth occurs during the period of their mineralization under the influence of certain diseases (acute infectious diseases, measles, scarlet fever, rickets, diseases of the gastrointestinal tract, dystrophy, brain disorders) at the age of 6 months to 1.5 years. Hypoplasia can appear in the following forms: discoloration (white or yellowish spots on the teeth with a shiny surface and painless upon probing), wavy enamel, absence of enamel in a certain area. Spots with hypoplasia have pronounced symmetry and are characterized by stability (they do not change their shape and color). When the child’s body weakens, caries may occur at the site of the defects. Treatment of dental hypoplasia consists of filling the affected areas of the teeth with composite materials, using sodium fluoride paste, and coating the teeth with fluoride-containing varnish. It is also necessary to normalize general metabolism.
Enamel hyperplasia – “enamel drops” (pearls). These drops are usually located in the cervical area of the crowns of both permanent and baby teeth and have a diameter of 2-5 mm.
Dental fluorosis (endemic fluorosis) is a disease observed in individuals (mainly children) who live for a long time in areas with high fluoride content in water and soil (more than 1 mg/l). Fluorosis is a peculiar form of hypoplasia. Depending on the concentration of fluoride ions, stains that appear on the surface of teeth during fluorosis can have different colors - from white to brown and even black. The more fluoride in drinking water, the more often fluorosis occurs and the less often caries occurs. A predisposing factor to the development of fluorosis is a decrease in the body's reactivity (infectious diseases, endocrine disorders). Fluorosis spots are stationary, dense, with a shiny surface, painless and smooth upon probing. With fluorosis (as opposed to hypoplasia), caries almost never occurs, due to the fact that fluorapatite is deposited in the spots (hence their high microhardness and resistance to acids). Treatment of fluorosis. In the early stages (change in enamel color), bleaching is recommended, followed by remineralizing therapy; calcium and phosphorus supplements are prescribed. It is necessary to increase children's intake of proteins, milk, fruits, vegetables, and limit the consumption of fatty foods. In winter, fish oil, multivitamins, and ultraviolet irradiation are prescribed. It is important to maintain the correct daily routine and conduct general hardening of the body. For complex forms of fluorosis, methods of cosmetic dental restoration or covering teeth with artificial crowns are effective.
Marble disease is a congenital familial osteosclerosis (an abnormal increase in bone density). In this case, the bones of the entire skeleton are affected. After teething, teeth have a chalky tint, and then the enamel becomes loose and is quickly lost. The process can develop into a malignant form.
Wedge-shaped defects are a type of damage to dental tissues located near the walls of the teeth, on the cheek and labial surfaces. The defect has the shape of a wedge with the base towards the neck of the tooth and the apex towards the cutting edge or chewing surface. A wedge-shaped defect, as a rule, does not bother the patient much: pain occurs rarely (only briefly from thermal and chemical irritants), the tooth cavity is not affected and is not opened, the defects slowly deepen, and softening is not determined (this distinguishes the defect from caries). The causes of the wedge-shaped defect have not been fully established. There is a point of view that it occurs under the influence of mechanical factors (for example, a toothbrush). It is sometimes believed that since a wedge-shaped defect begins after exposure of the tooth wall, it is one of the manifestations of periodontal disease. There is evidence of the role of endocrine disorders, diseases of the central nervous system and gastrointestinal tract in the occurrence of a wedge-shaped defect. Treatment of a wedge-shaped defect is aimed at strengthening the hard tissues of teeth through the use of remineralizing therapy (applications of calcium, phosphorus, fluorine, use of fluoride varnish, fluorine gel, etc.). In advanced cases, filling with composite materials or orthopedic treatment (artificial crowns) is recommended.
Increased abrasion of dental tissues . The wear of tooth enamel is a completely natural process that occurs in all people by the age of 45-50. However, in a certain group of people, pathological abrasion occurs already at a young age. Not only the enamel is erased, but also almost completely the crowns of the teeth (most often the front teeth). The causes of the disease are: the habit of grinding teeth during sleep, disorders of the parathyroid glands, almost complete loss of chewing teeth (which increases the load on the front teeth). Treatment – orthopedic or orthodontic (in order to properly distribute the load on the teeth).
Erosion of hard dental tissues is the progressive loss of enamel and dentin on the vestibular surface of tooth crowns. Areas of erosion have an irregular rounded shape. The causes of tooth erosion are considered to be the mechanical effects of toothbrushes, endocrine disorders (in particular, increased function of the thyroid gland - thyrotoxicosis). It occurs mainly in middle-aged people and lasts 10-15 years. There are different degrees and stages of the process. Treatment is aimed at additional mineralization of hard dental tissues. Erosion is filled with composite materials and artificial crowns are made. Calcium and phosphorus preparations, multivitamins with microelements are prescribed internally.
Necrosis of hard dental tissues initially manifests itself in the loss of enamel shine, then chalky spots appear, gradually turning into dark brown. Softening appears in the center of the spots, the enamel becomes brittle and easily chips. Necrosis differs from erosion by softening in the center of the spot. Teeth are extremely sensitive to any irritants. The causes of necrosis are endocrine pathologies (hyperthyroidism, dysfunction of the gonads), pregnancy, diseases of the central nervous system, chronic intoxication of the body, hereditary factors. Treatment is aimed at eliminating tooth sensitivity, remineralization, and normalizing endocrine disorders.
Dental injuries. Acute dental injuries occur when a tooth is exposed to traumatic factors - impact, increased load during chewing, constant pressure from improperly made orthopedic structures. Injuries are more common on children's baby teeth (luxation, tooth fracture, crown fracture). Acute dental injuries include: tooth bruise, tooth dislocation (complete and incomplete), fracture of part or the entire crown, combined injury, tooth germ injury. If a tooth is bruised, it is necessary to rest it, eliminate contact with opposing teeth by grinding off the cutting edge, and exclude solid foods from the diet. It is necessary to monitor the condition of the pulp, and in case of irreversible changes, remove it and fill the canal. Tooth dislocation with healthy gum tissue rarely occurs. However, if there is periodontal pathology, in particular, bone tissue resorption, tooth dislocation can easily occur even when chewing hard food. In case of incomplete dislocation of a tooth, it is necessary to create rest for which the tooth is splinted. If the pulp ruptures, it is removed and the canal is filled. If part of the crown breaks off, it is restored using composite materials. Sometimes special pins are used.
Bibliography:
- Lutskaya I.K., Nichiporovich G.S. Frequency of enamel and dentin cracks in permanent teeth. Dental Journal 2006, number 2. Page. 87-91.
- Nichiporovich G.S. Modern ideas about the increased sensitivity of hard dental tissues. Dental Journal, 2006, number 2. Page. 92-95.
- Leus P.A. Non-carious diseases of hard dental tissues. Educational and methodological manual. Minsk, BSMU-2008, 56 pages.
- Borovsky E.V., Leus P.A. Erosion of hard dental tissues. Dentistry 1971. T. 50 No. 3.p. 1-5.
- Fedorov Yu.F. Clinic and treatment of hyperesthesia of hard dental tissues. - M 1970, 140 pp.
- Leus P.A., Kozel O.A. Disturbances in the development of tooth enamel. Educational and methodological manual. Minsk, BSMU-2004-29 pages.
Author: Shulyak Alesya Vadimovna
Tooth injury
Enamel damage
.
Enamel is the only tissue of ectodermal origin with an acellular structure, without blood vessels and nerves. According to modern concepts, tooth enamel is the strongest tooth tissue. Although the proportions of the enamel are quite small. According to research, the volume of enamel in chewing teeth is 2.3–3.5 mm, and in baby teeth – no more than 1 mm. There are several types of tooth enamel structure. Type 1
is defined as having a uniform coating that is an organic coating of enamel.
The organic matter has a dense structure with poorly defined enamel prisms; this structure corresponds to areas of non-crystalline enamel. Type 2
is characterized by zones in which the organic coating only partially covers the underlying inorganic component, resulting in the formation of scalloped tissue.
The contours of the enameled prism can be observed on the surface. Type 3
is characterized by the absence of an organic coating on the enamel surface and clearly defined contours of the enamel prism.
Type 4
is characterized by a homogeneous organic coating on the enamel surface with faintly defined contours of the enamel prism, which give the design a wave shape.
Different types of enamel structure determine the unequal resistance of the surface layer of enamel to various external factors, leading your teeth to injury, including the development of dental caries. Enamel decay
is extremely common.
Most cracks are not very noticeable and can easily be missed during a routine dental examination. Most cracks are vertical, with the exception of the mandibular incisors. Such changes in the enamel structure are the basis for subsequent tooth destruction. Dental intervention is necessary in order to subsequently avoid problems with dental health, otherwise the development of caries is guaranteed. Dentin destruction.
Dentin is one of the strongest biological materials in the human body.
In humans, teeth come into contact almost 5,000 times a day during normal use. Despite the fact that we use force while chewing, healthy teeth do not break, since the structure of the teeth is quite rigid because the base is dentin. Dentin
is a component of a special component in the bone, which consists of mineral particles, collagen and water. Despite the fact that enamel and dentin are composed of the same mineral (carbonated hydroxyapatite), dentin is a complex microcomposite material. When the integrity of dentin is violated, many clinical situations arise that can destroy your tooth. -Tooth fracture A tooth fracture is a rupture or crack in the dentin of a tooth. The outer shell of the tooth protects the pulp, which contains nerves and blood vessels. A fracture is a break in the chewing surface of a tooth. Typically, the tooth cracks from the chewing surface downwards and in some cases reaches the root of the tooth. A vertical fracture also occurs, when cracks begin at the root and move toward the chewing surface. The main cause is chewing hard food or accidentally biting off a hard object. But the occurrence of injury associated with external threats, including a car accident or sporting event, is no exception. Tooth fractures are more common in older people because teeth wear down over time. Teeth with dental caries or decay are especially susceptible to fracture. We would like to note that not all tooth fractures cause painful symptoms; often the fracture causes irritation or infection in the pulp, which is not accompanied by toothache. Main symptoms of a tooth fracture:
- Pain when chewing food.
- Chew food on one side only to avoid discomfort.
- Acute pain when biting into dense food. -Pain when interacting with cold or hot food and air.
- Occasional pain lasting 3 to 10 seconds (even when swallowing saliva).
Vertical root fractures
may not be noticed until the infection affects the bone or gum.
If the tooth itself is visually intact, the fracture may not be visible to the naked eye. That’s why modern dental clinics are equipped with a special dental microscope. Although this is not the only way to detect a fracture, other options include staining (a solution is applied to the tooth to help see the crack), transillumination (passing light through the tooth), periodontal probing (using special instruments to determine the extent of the crack), bite testing (you will be asked to bite down on a special object to find the specific tooth causing the problem), x-ray (to look for certain defects, as not all fractures can be seen on x-ray. Early diagnosis can help save the tooth before the fracture progresses). Teeth do not heal on their own.
The goal of treatment is to protect the tooth and the inside of the pulp. Talk to your dentist and choose a treatment plan that suits your cost and treatment time. Treatment of the tooth will depend on the severity of the damage. Tooth restoration options may include:
- A crown is a dental covering. However, a temporary crown will be installed first to make sure that it solves the problem. A permanent crown is installed only after wearing a temporary onlay for a short time (this allows not only to properly restore the tooth, but also to avoid problems with its further use).
- A veneer or Lumineer is a thin covering that is placed over a tooth if there is a small chip on the surface; in some cases, dentists resort to restoration with a composite material. However, if the fracture has affected the root of the tooth, you cannot do without root canal treatment. Root canal infection is a common clinical situation in cases of severe pulp damage. The root canal is depulped and filled with filling material. Tooth extraction is used as a last resort only in emergency and very difficult situations when saving the tooth is not possible.
Pigmentation of teeth
A non-carious pathological condition in which teeth become brown, yellow, gray, pink, black, red or another unusual color or shade. In most cases, pigmentation develops against the background of demineralization of the enamel, accompanied by hypoplasia and hyperesthesia. Pigmentation occurs under the influence of general (diseases, medications) and local (smoking, food colorings) factors and occurs in 85% of people, more often in men than in women. Treatment of this non-carious dental disease involves regular professional cleaning and whitening, but often the only way to restore the aesthetics of the dentition is prosthetics.
Causes of tooth pigmentation:
- demineralization of enamel;
- chips and other injuries to hard dental tissues;
- poor oral hygiene;
- treatment using iodoform and resorcinol-formalin, as well as “silvering” of teeth;
- rupture of the neurovascular bundle (pulp);
- smoking;
- taking certain medications and foods with added food coloring;
- hemolytic disease;
- uroporphyria;
- Excessive production of pigment in the body.
Pigmentation, like many other non-carious lesions, develops not only after, but also before teething. Thus, pigmentation in a child is often a consequence of the mother taking tetracycline antibiotics during pregnancy, which, penetrating the placenta, are deposited in the bones and tooth buds. Since the composition of dentin and enamel remains virtually unchanged over time, one cannot expect that yellow-brown pigmentation will disappear with age.
Symptoms of tooth pigmentation
The natural color of enamel is milky white, all other options indicate pathological pigmentation. The color of teeth affected by non-carious diseases varies. Thus, with a hemolytic disease accompanied by bilirubin deposition, the teeth are painted in various shades of gray, blue, green and brown, while “tetracycline” pigmentation is yellow-gray. Red staining is characteristic of uroporphyria, and gray staining is characteristic of pulp necrosis. In cases of exogenous pigmentation (associated with external factors), enamel and dentin are colored dark brown by nicotine, and pink by resorcinol-formaldehyde paste (not currently used in dentistry).
Treatment of tooth pigmentation
If, based on the patient’s complaints, clinical examination data and the results of additional studies (radiography and thermography), pathological pigmentation of the teeth is diagnosed, then treatment begins immediately. The therapy consists of sanitation of the oral cavity, including thorough removal of dental plaque (professional cleaning with ultrasound and using the Air Flow air-abrasive system). In case of deep pigmentation, intracanal and external bleaching is carried out using special preparations. However, not all types of pigmentation are eliminated by bleaching. Thus, the procedure will not eliminate tetracycline discoloration and color changes that appear as a result of oxidation of metal pins installed in the channels and silver amalgams. In these cases, pigmented teeth are covered with crowns and veneers (if their condition allows this). When treating non-carious pigmentation in children, consultations with a pediatrician and a genetic specialist are often required.
What is tooth sensitivity?
In other words, dentin hypersensitivity. If cold, heat, sugar, salty, sour or just cool air have a painful reaction on your teeth, then you have all the symptoms of tooth sensitivity. The symptoms are very common and it is estimated that a large proportion of the population experiences this sensation. Why does tooth sensitivity (dentin hypersensitivity) occur? Tooth sensitivity is usually caused by dentin in areas of the roots exposed due to gum extraction or periodontal disease. Receding gums are very common, and by age 65, four-fifths of people will have gum recession.
Causes
Hyperplasia can occur for a variety of reasons. The most common cause of gum tissue overgrowth is the use of certain medications that block calcium channels. The following drugs should be avoided:
- phenytoin;
- cyclosporine;
- nifedipine;
- felodipine;
- diltiazem.
If taking a medication caused gum overgrowth, the doctor should select another drug that does not cause such consequences. Causes:
- pregnancy;
- blood diseases;
- puberty in adolescents;
- malocclusion;
- the presence of tartar and other dental deposits in large quantities.
Gum hyperplasia often occurs with leukemia, as a result of taking a large number of different medications.
Why does tooth sensitivity (dentin hypersensitivity) occur?
When the root of a tooth becomes exposed, it does not have a layer of enamel like the crowns of your teeth. The roots have a very vulnerable coating - cementum, which, after the loss of the top layer, leaves the dentin exposed. Excessive brushing with highly abrasive dental paste causes abrasion of the surface of the tooth enamel and exposes dentin. A very acidic diet with lots of acidic fruits and pickles can also cause tooth decay and dissolve the surface of the tooth, exposing dentin. It is important to visit your Doctor periodically if you have any symptoms of sensitivity so that he can examine your mouth and identify any symptoms associated with dentin sensitivity and suggest you the best treatment plan. When teeth react painfully, brushing them can be painful, and if you don't brush your teeth because of pain, it can lead to the destruction of enamel and gum disease. Reactions to heat, cold, sugar, sour and salty foods and drinks are also a clear sign of tooth decay, or a sign of a broken tooth, in which case your dentist will treat you comprehensively. Some of the most common causes of sensitivity are:
- Gum recession due to age or improper brushing of teeth
- Acidic drinks (such as soda), which cause enamel erosion and dentin attack
- Brushing with very low quality toothpaste, improper brushing, and brushing more than three times a day will result in loss of enamel.
- Gum disease that can lead to gum recession
- A broken or fractured tooth can expose dentin
Additionally, some dental procedures may cause sensitivity. Procedures such as teeth whitening, professional teeth cleaning, braces or fillings are known to cause sensitivity during or after the procedure.
Structure of tooth enamel
Tooth enamel is the main protector of teeth and completely covers their crown part. The average thickness of the tissue is about two millimeters: in the chewing area the layer is slightly thinner, and on the sides of the teeth, on the contrary, it is thicker. The color of tooth enamel depends on its density and the quality of dentin, as well as on some individual characteristics of the body, but this type of tissue is essentially transparent.
The composition of tooth enamel includes, for the most part, inorganic substances (more than 95%). The percentage of water content is very small (approximately 3%): this is partly why such high strength is achieved. Inorganic materials primarily refer to hydroxyapatite crystals (a mineral containing fluorine, magnesium, carbon and other elements). The presence of hydroxyapatite crystals also explains the fact that the enamel is vulnerable to the effects of an acidic environment, i.e. The consumption of foods that increase the acidity of saliva is contraindicated. This is especially true for calcium ions, on which the integrity and density of the enamel largely depends.
Can you prevent tooth sensitivity on your own?
Of course, yes, if you keep your mouth clean, observing all oral hygiene standards, which will help stop gum loss and, as a result, periodontal disease. Thorough flossing and flossing as recommended by our dentist can help reduce the chance of avoiding this disease. A diet without consuming acidic foods also helps stop the development of this symptom. Ignoring the disease can lead to other health problems, leaving you vulnerable to tooth decay and gum disease.
What to do if you have sensitive teeth?
See your dentist first. The doctor will offer you all treatment options. It is also important to tell your Doctor if the cause is not dentin (root) hypersensitivity, the tooth may be reacting due to a more serious problem. To treat increased reactivity to stimuli, your Doctor will definitely recommend using a low abrasion dental paste designed for such clinical cases - desensitizing toothpaste. These toothpastes make your teeth less sensitive if you brush them twice a day, and also contain fluoride to protect your teeth from decay. In addition, your dentist may prescribe a fluoride gel, fluoride rinse, or a high-consistency fluoride toothpaste that is specially formulated to make your teeth less sensitive and provides additional protection against tooth decay. These procedures are carried out at home and are inexpensive. Other procedures for sensitive teeth that your dentist or hygienist may suggest in your dental office.
Sensitivity due to gum disease, what is it?
Gum disease
is an inflammation of the gums that can progress to affect the bone that surrounds and supports your teeth, which also causes sensitivity, which we often confuse with tooth sensitivity. It is caused by bacteria in plaque, which always forms on tooth enamel. If plaque is not removed by daily brushing and flossing, thick plaque will form and bacteria will then infect the entire mouth. This can lead to weakening of the gums and, as a result, teeth falling out or being removed by the dentist.
Stages of gum disease:
- Gingivitis: This is the earliest stage of gum disease and is caused by the formation of plaque on the gums. If daily brushing is not carried out promptly or does not meet all hygiene standards, plaque produces toxins (poisons) that can irritate the gum tissue, causing gingivitis. You may notice some bleeding during dental hygiene. If gum problems are detected early, the damage may be localized because the bone and connective tissue that holds the teeth in place are not yet affected.
- Periodontitis: At this stage, the bone and fibers are irreversibly damaged. Your gums may begin to form a pocket under the gum that traps food and plaque. Proper dental treatment and improved home care usually help prevent the disease from developing. Advanced periodontitis: In this final stage of gum disease, the fibers and bone that support the teeth are destroyed, which can cause the teeth to shift or become loose. This can affect your bite, and if aggressive treatment cannot save them, your teeth may need to be removed.
What it is
Hyperplasia is a random rapid increase in gum tissue cells. Hyperplasia is not a tumor; it is benign changes in cell tissues, in which the cells themselves continue to perform their functions without changes. With hyperplasia, unlike oncological diseases, cells do not grow into surrounding tissues and do not metastasize. Many doctors are inclined to believe that it is not always a pathology, but only an experienced doctor can decide on a treatment method.
Gingival hyperplasia is manifested by excessive growth of tissue that can partially or completely cover the entire crown of the tooth. With this disease, only the gum tissue grows; the cheek and tongue tissues are not affected by changes. Hyperplasia is not an inflammatory process, so there is no drug treatment for it. In addition, it is necessary to correctly carry out differential diagnosis of the disease, being able to distinguish it from cysts and other tumor neoplasms. And only an experienced dentist can do this. Therefore, if you find that your gums are growing by leaps and bounds, consult a doctor immediately.
Gum hyperplasia is also accompanied by increased blood supply to the gums, so when brushing your teeth, the gums often bleed. Often patients mistake this disease for gingivitis or periodontitis and self-medicate, which does not bring any effect. In order not to waste time and not to advance the disease to such a stage when the tooth is completely under the gum, you must immediately consult a doctor.
How do you know if you have gum disease?
Gum disease is most common in adults. If detected in the early stages, the problem can be corrected with minimal consequences, please contact your dentist if you notice any of the following symptoms:
- Gums that are red, swollen, or swollen or tender
- Gums that bleed when brushing or flossing
- Teeth that look longer because your gums have receded
- Gums that have separated or pulled away from your teeth, creating a pocket
- Changes in the way your teeth fit together when you cleave them together
- Pus between teeth and gums
- Constant bad breath
- How is gum disease treated?
When you detect the first symptoms of gum disease and proper oral hygiene, you will rid your teeth of plaque and avoid the development of the disease. Professional cleaning with a Doctor is the only way to remove plaque that has accumulated and turned into tartar. Your Doctor will clean your teeth and remove tartar from above and below the gum line.
Causes of gum overgrowth
Establishing factors that contribute to an increase in periodontal volume makes it possible to reduce the risk of recurrence of an unpleasant situation and draw up a competent treatment plan.
The main causes of gum hyperplasia:
- inflammatory process in the gingival area;
- mechanical damage to soft tissues;
- taking certain medications (immunosuppressants, anticonvulsants, antihypertensive drugs - calcium channel blockers);
- the presence of certain systemic pathologies (hormonal imbalances, metabolic disorders, systemic connective tissue diseases, leukemia);
- oncological processes in the body;
- accumulation of tartar in the cervical part of the tooth crown;
- increased spaces between teeth or teeth growing at an angle;
- complication of gingivitis, periodontitis.