With the development of implantation technology, more and more patients prefer this method of restoring lost teeth, as the most reliable, aesthetic and convenient. Set it and forget it! This is exactly what happens in most cases, unless the plans of the doctor and his patient are disrupted by the most formidable complication, due to which the implant can be lost - peri-implantitis. This is what visitors to numerous dental forums scare each other with, so much so that some give up the idea of installing an implant altogether. In this article, let's figure out what peri-implantitis is, how to avoid it, and, if necessary, treat it.
What is peri-implantitis?
Peri-implantitis is an inflammation of the tissues and bone surrounding the implant, which ultimately, without timely intensive treatment, leads to bone loss and loss of the implant.
Peri-implantitis is much easier to prevent than to stop a process that has already begun. The main cause of the disease is a bacterial infection, which can occur either at the moment of implantation, and then the symptoms of the disease appear a few days after the operation, or after some time - from several months to several years.
Mucositis – the best of the worst
Mucositis after implantation is also a common problem, although not as serious as peri-implantitis. This is the initial stage of implant rejection, when only soft tissues become inflamed and the bone is not affected.
How does mucositis manifest:
- erythema - redness;
- thinning of the mucosa at the site of inflammation;
- hyperplasia - swelling of the gums;
- ulcers on the inside of the cheeks and gums;
- white spots on the mucous membrane are a symptom of the death of soft tissue.
Painful sensations while eating, increased body temperature, malaise, dry mouth, and weight loss also accompany dental mucositis. The disease rarely leads to the loss of an implant, but the danger is different: with advanced mucositis, the mucous membrane in the mouth is so inflamed that the patient cannot even swallow, nutrition is only possible through a tube.
Why does peri-implantitis occur?
According to statistics, during implantation, more than 95% of implants are successfully installed and take root. 5% of failures are associated with various reasons, but in approximately 1% of cases, peri-implantitis is “to blame” for the loss of the implant, i.e. inflammation affects approximately 1 artificial tooth root out of 100. You need to understand that complications are possible with any surgical intervention. It depends on the patient's health and immune system. If the patient has disorders or may have a decrease in immunity under the influence of unfavorable external factors, this must be taken into account. That is why implantation requires preliminary thorough diagnosis by the surgeon.
Other causes of implant infection and the development of peri-implantitis can be:
- Incorrect behavior of the patient himself after implantation:
- poor hygiene,
- violation of the treating dentist’s recommendations for the care of implants,
- increased chewing load, careless attitude towards your artificial teeth, gum injuries near the implant,
- smoking,
- ignoring routine examinations to monitor the condition of the implant roots.
- Mistakes made by specialists during implantation:
- an inappropriate prosthetic technique was chosen,
- the implant is placed in the wrong place,
- the implant is installed in a hole with a larger diameter than required,
- the load on the implant was incorrectly calculated,
- a complete diagnosis was not carried out and/or the patient’s health status was incorrectly assessed before implantation,
- During the operation, asepsis was violated.
- A low-quality implant was installed. This can happen due to the fault of the dentist or at the insistence of the patient himself.
- There was a source of infection in the patient's mouth - caries, periodontal disease, dental plaque and calculus. In order for implantation to proceed without complications, all sources of possible infection in the oral cavity must be eliminated at the preparation stage.
Possible risks and complications
The negative consequences that arise against the background of long-term progression of the pathology include:
- From the local group - periostitis, inflammation and necrosis of bone tissue, the formation of cysts and granulomas, rejection of the artificial pin;
- From the systemic category - pericarditis, infections of the maxillary sinuses and vital organs, sepsis.
Systemic complications usually occur with a long-term closed fistula, when purulent masses with infection, instead of coming out, penetrate into the surrounding tissues and organs. Of these, the greatest danger is blood poisoning, which poses a threat to human life.
Treatment procedure
Before starting a treatment course aimed at eliminating a fistula formed after implantation, an X-ray examination is required to identify the source of inflammation, as well as the volume of affected bone tissue. The dentist’s task comes down to opening, cleaning and antiseptic treatment of the cavity, followed by suturing and conducting a therapeutic course. If the source of inflammation is located in the middle or apical area of the implant, it is necessary to provide access to it by cutting out the bone in the projection of the site of inflammation.
Symptoms of peri-implantitis:
- The disease begins with redness, discomfort and swelling of the gums in the area of the installed implant.
- There is bleeding of the gums in the problem area.
- At the site of inflammation, connective tissue begins to grow.
- The gum moves away from the implant, as in periodontal diseases, and a periodontal pocket forms around the titanium rod.
- Serous fluid and pus may be released from the pocket, and a fistula may form.
- The X-ray image reveals a noticeable loss of bone tissue around the implant.
- The implant becomes loose, the patient feels its mobility, this provokes further destruction of the bone around the titanium rod.
- Ultimately, if the inflammatory process is not stopped, implant rejection occurs.
What is the danger of a fistula near an implant?
The fistula tract itself is not dangerous; to some extent, it even helps to temporarily stop the growth of the cavity with pus, since excess accumulated exudate comes out through it. However, its appearance indicates extensive purulent inflammation. It cannot be limited to a local cavity for a long time and will spread further. This can lead, in addition to damage to soft tissues, to destruction of the jaw bone. In the future, a fistula during tooth implantation can lead to serious complications:
- extensive inflammation of the periosteum,
- mobility of living units and installed implants,
- complete loss of teeth and loss of artificial structures,
- growth of the inflammation focus into nearby structures: inner ear, sinuses,
- the appearance of multiple cysts in the jaw,
- sepsis - infection of the blood and lymph,
- multiple organ failure: damage to internal organs due to sepsis.
Read more about the most dangerous complication after implantation in the material “Dental implant rejection.”
How is peri-implantitis treated?
The success of treatment for peri-implantitis depends on what stage of the disease it is started at: the earlier, the better the prognosis.
Treatment is aimed primarily at relieving inflammation in the area and restoring bone volume once it has begun to be lost. Therefore, there are 2 main stages in treatment - sanitation of the inflamed area and surgical bone augmentation.
- Before starting treatment, the doctor conducts a diagnosis. The main stage of such a diagnosis will be a 3D CT scan to accurately determine the affected area and the condition of the bone tissue.
- Then professional hygiene of the implant and adjacent areas is carried out - removal of soft dental deposits and tartar from the dental crown and from the subgingival space using ultrasound.
- Next, surgical sanitation of the area of inflammation is carried out - the abscesses are opened. Cleaning of periodontal pockets is carried out in the same way as for periodontal diseases - using special curettes or the Vector device. It is advisable that the problematic implant is not loaded.
- At the same time, bone grafting can be performed using the method of directed bone regeneration using bone chips and regenerating membranes.
- In parallel, the patient is given local and general antibacterial therapy and antibiotics are prescribed.
- When treating peri-implantitis, it is very important to maintain daily hygiene using antiseptic drugs.
The result of treatment is necessarily monitored by repeated x-ray diagnostics.
It must be remembered that peri-implantitis is prone to frequent relapses, therefore, after treatment, monitoring the condition of the implants and increased attention to proper hygiene are MANDATORY.
Diagnostics
Determining the presence of the fistula itself is not difficult. To assess its depth and diameter, it is possible to use a special probe inserted into the resulting oroantral tract. To assess the extent of inflammation and the presence of additional passages, it is possible to use radiography of the upper jaw with the introduction of a contrast agent.
Evaluation of the presence of a foreign body or apex of the tooth root is carried out during radiography or directly during the operation to close the fistula. If there is no effect from antibacterial therapy, it is possible to culture the microflora to determine its resistance to antibiotics of various types of action.
Prevention of peri-implantitis
From all of the above, it follows that peri-implantitis is much easier to prevent than to treat later. In order to protect yourself as much as possible from such a complication, both immediately after implantation and during subsequent life with an implant, you must:
- Carefully monitor oral hygiene, use not only a toothbrush and toothpaste to care for teeth and implants, but also special products - a monotuft brush, a dental brush, special dental floss and an irrigator. Visit a hygienist regularly for professional oral hygiene.
- Do not violate the recommendations of your doctor immediately after the implantation procedure.
- Pay attention to your health, strengthen your immune system, and don’t smoke.
- Regularly undergo scheduled examinations with your attending physician with RG diagnostics at least once a year to monitor whether there is bone atrophy.
- Carefully choose the clinic and doctor where you get implants.
- Place implants of brands that have already proven themselves among doctors and patients - in this case, the savings turn against the patient, because If the implant fails, you will have to undergo quite expensive treatment and pay for the implantation again.
After dental implant surgery
After installing a dental implant, to ensure the normal course of the healing process, you must follow the dentist’s recommendations. Their implementation will allow the body to ensure that the results of the intervention are recorded and make it easier to bear stress.
Doctors' advice for the first week after the intervention
In the first time after surgery, experts recommend:
- Avoid the possibility of nerve hypothermia when applying a cold compress to the cheek.
- Do not eat before the end of the action of the painkiller, which takes about 2 hours to be completely absorbed.
- Avoid eating spicy, fatty and acidic foods during the first 7 days after the procedure.
- Avoid taking cold and hot food and liquids, giving preference to foods and drinks heated to a warm temperature.
- Ensure that you stay in a position during the day in which your head is located above chest level.
Note! In the first few weeks after implant installation, doctors advise sitting more often, using high pillows for sleeping, and not leaning back while sitting in a chair.
- To avoid impact on the area undergoing surgery, rupture and divergence of sutures, it is recommended to sleep on your side, on the side opposite to the one on which the manipulations were performed.
- Clean hard-to-reach areas of the oral cavity from food debris using dental floss.
- Avoid work associated with moving heavy objects and heavy physical activity, during which pressure is created due to the automatic compression of teeth, which can negatively affect the process of implant healing.
In addition to the recommendations listed, safe and rapid healing can be ensured by the use of painkillers (Ketonal, Nise), Curasept disinfectant rinse, and topical wound healing ointment Solcoseryl.
Recommendations from dentists for the second and subsequent weeks after the procedure
Despite the fact that with normal care, after the first 7 days after surgery, partial healing of the affected structures and bone tissue around the implanted element is observed, dentists recommend that patients follow the instructions. After the first week, if healing is successful, based on the results of a routine examination, the dentist may allow the sutures to be removed; in more severe cases, it will take about 3 weeks for them to be removed. Recommendations from specialists at this stage of restoring the integrity of dentition elements may include advice regarding:
- The need to ensure proper oral care, avoiding the use of products with a powdery consistency when brushing your teeth.
Important! Qualified dentists recommend refraining from brushing your teeth with toothpaste; they recommend giving preference to a gel, which will ensure the safety of the gums while completely eliminating pathogenic microflora.
- Quitting smoking, since nicotine entering the body leads to the destruction of bone structures, weakening of the gums, which provokes the development of inflammatory processes and necessitates the need for additional therapy.
- The need to avoid touching the area where the implant is located using the tongue, fingers or mechanical devices.
Note! To speed up the process of tissue regeneration in the damaged area of the oral cavity, it is recommended to rinse with a saline solution diluted in the proportion of 1 teaspoon of salt per 200 ml of warm water.
- When choosing the right toothbrush, it is recommended to choose one with soft bristles or purchase a children's brush.
- Adjusting the diet to increase the amount of foods high in calcium (dairy products, white cabbage).
- The need to avoid air travel, climbing to heights, and visiting saunas and steam baths.
- Avoiding alcohol (for at least 1 month), the use of which dulls the sense of pain and reflexes. As a result, if the area where the intervention is located is damaged, the patient will feel pain after a certain period of time, which increases the risk of complications due to delayed medical care.
- The need to avoid eating sticky and hard foods, such as nuts, carrots, crackers, seeds and stretchy sweets until bone and soft tissues have completely healed.
Important! In most clinical cases, pain symptoms disappear after 7 days, but if you experience discomfort after the specified time period, you should consult your dentist. Most likely, he recommends taking Ibuprofen over the next few weeks, emphasizing the need to respect the timing and dosage of taking this potent drug.
The frequency of visits to a specialist decreases as rehabilitation progresses from once every 1.5 weeks during the first 2 months after the procedure to one visit every 6 months after complete restoration of the damaged structures with an implanted element.
Treatment methods
Treatment is carried out in stages. First, the inflammatory process is eliminated using therapeutic methods, then surgical sanitation is performed. At the first, conservative stage, the oral cavity is sanitized, plaque and tartar are removed. Peri-implant pockets are irrigated with special solutions. At home, the patient should rinse his mouth and make applications with medications.
Then the surgical stage begins. To access the bone and surface of the implant, an incision is made in the gum and a periodontal flap is created. Through the formed hole, the doctor removes granulation tissue, cleans the surface of the implant with a curette and rinses the pocket. The wound is sutured and covered with a bandage. During the postoperative period, it is important to exclude the development of an infectious process, therefore a course of antibiotics and rinsing the mouth with antiseptics are prescribed.
If the pathological process is started and accompanied by relapses, the only solution is to remove the implant. After this, thorough treatment is carried out, and after complete recovery, reimplantation is carried out.
Treatment of peri-implantitis is complex and takes a long time, so it is very important to choose the right clinic where implantation will be performed. Installation of implants by an experienced surgeon will minimize the risk of medical error, and subsequent implementation of all his recommendations will prevent the development of inflammation in the postoperative period.
Implantologists at the 32 Dent clinic have extensive experience in successful operations. We work with certified materials and install high-quality implants from well-known brands. Implantation in our clinic is a safe procedure.
Establishing diagnosis
The success of treatment largely depends on when the patient consults a doctor. Therefore, we recommend visiting a dentist as soon as the first signs of peri-implantitis appear - swelling and bleeding of the gums. The doctor will conduct an examination and prescribe additional research to clarify the diagnosis:
- Dentistry.
- X-ray examination.
- Computed tomography.
These methods allow not only to clarify the diagnosis, but also to assess the degree of bone tissue loss. Additionally, laboratory tests may be prescribed.
What can happen during surgery
No matter how expensive and high-quality implants are, complications during surgery depend on the qualifications of the implantologist. This is why choosing a doctor is so important. Experienced doctors practically never have misfires in the form of:
- Bleeding
due to vessel damage
Bleeding may be associated with increased blood pressure and poor blood clotting. However, in the vast majority of cases, vessel rupture occurs due to surgeon error.
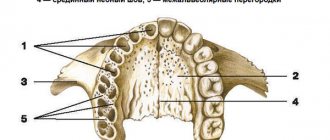
- Perforation of the maxillary sinus
In the upper jaw there is little bone for installation; it often has to be replanted (sinus lift). When implanting upper teeth, it is easy for the doctor to make a mistake and drill a hole that is too deep. 3D modeling and surgical guides, coupled with the surgeon's experience, significantly reduce such cases.
- Nerve injury
When working on the lower jaw, there is a possibility of touching the alveolar, mental or lingual nerve. This leads to numbness. This is why implantologists insist on performing a CT scan before surgery, this helps to make accurate measurements in the area where the pin is being implanted.
Alveolar wall
The result of an incorrectly selected implant size.
Modern technologies: 3D modeling, surgical templates, CT and orthopantomogram virtually eliminate operational errors.