We have repeatedly written that “sick teeth mean a sick body.” Many diseases have a close connection with dental health (see “Two scientific experiments that will make you go to the dentist”) and dental health is an indicator of the health of the body! Ignoring even simple hygiene rules and timely visits to the dentist is fraught with the possibility of the appearance of one or another disease.
In this article we want to talk about such an unpleasant disease as osteoporosis and, it would seem, what does the dentist have to do with it?
Osteoporosis (lat. osteoporosis) is a chronically progressive systemic disease of the skeleton or a clinical syndrome manifested in other diseases, characterized by a decrease in bone density, a violation of their microarchitecture and increased fragility due to impaired metabolism of bone tissue with a predominance of catabolism over the processes of bone formation, a decrease in bone strength and an increase risk of fractures. Wikipedia .
Medical observations show that a toothbrush can serve not only to prevent caries, but also that osteoporosis can be accidentally discovered with its help. Scientists have developed a unique program that can recognize decreasing bone density on an X-ray. Dental imaging may become a method for diagnosing osteoporosis in the future.
Research shows that plain radiographs are a simple and inexpensive method that can help identify patients with incipient osteoporosis. Such a place is the patient’s lower jaw – thinning of the bone can already be detected on an X-ray of the jaw.
What is periodontitis
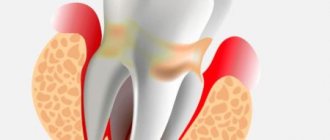
Periodontitis is an inflammatory process of the peri-root tissues of the tooth. Pathology develops regardless of a person’s age and gender. The disease is characterized by disruption of the periodontal ligament, destruction of osteocytes, formation of cysts, and loosening of the segment.
The periodontium is a layer of tissue penetrated by blood, lymphatic vessels, and nerve endings. It consists of the gum, alveolar bed and ligament. Due to this complex, each unit is held in its own hole.
The pathogenesis is based on the body's immune response to the inflammatory process. It manifests itself as a vegetative-vascular reaction. Blood flow to the affected area increases, stasis occurs in small vessels, and edema develops. The dentogingival connection is weakened, and under the influence of inflammatory mediators the bone begins to melt. This leads to expansion of the periodontal fissure.
Depending on the provoking factor that caused periodontitis, the following types are distinguished:
| Classification by cause of disease | Notes |
| Infectious | The most common. Periodontal infections are caused by plaque microorganisms. Under their influence, enamel and dentin are destroyed and caries develops. In the absence of medical intervention, microorganisms involve the pulp in inflammation, and pulpitis occurs. Further, along the root canal, the infection descends to the opening in the apex and enters the periapical tissue. In addition, an extra-dental route of infection entering the periodontium from surrounding tissues or hematogenously (periodontitis, osteomyelitis, tonsillitis, etc.) is possible. |
| Drug | Drug-induced periodontitis occurs when the dosage or exposure time of potent drugs during endodontic treatment is not observed. Medicinal substances exit through the root canal into the surrounding tissues, where they have a toxic effect. |
| Traumatic | It is provoked by mechanical impact on periodontal tissue (bruise, blow, improper root filling, etc.). |
The development of the disease is provoked by poor oral hygiene, diabetes, infections of the ENT organs, and metabolic disorders. There is an increased risk of inflammation in smokers and alcohol abusers.
Periodontitis can have a different course:
- acute form. Characterized by a vivid clinical picture. Based on the nature of the exudate, serous and purulent types of the disease are distinguished;
- Chronic periodontitis is a sluggish pathology with erased symptoms. There are fibrous, granulating and granulomatous periodontitis.
Chronic inflammation recurs from time to time. During exacerbation, the clinical picture corresponds to the acute form.
Depending on the location of the lesion, 2 types of dental periodontitis are classified:
- apical (near the root apex);
- marginal (the source of inflammation is located near the edge of the gum).
Implantation methods
Depending on the clinical picture, implants can be implanted using two-stage or one-stage treatment protocols. The latter are preferable because the screws can be installed at an angle, which provides greater coverage of the bone tissue, which means the system will be better stabilized.
With the classical method, an implant is first installed, and prosthetics are performed on average six months later. The operation is performed with dissection of the gums and suturing, that is, it is highly traumatic. Bone augmentation is almost always carried out. Bone grafting also requires a recovery period.
One-stage treatment protocols allow you to restore teeth in one stage, without blood and stitches, since micro-punctures are made in the gums to introduce an artificial root. A minimally invasive procedure is more comfortable for the patient, and the recovery period is easier.
One-stage implantation methods:
- installation of an implant immediately after tooth extraction - one-step;
- restoration of a tooth segment or a complete row - basal;
- treatment of complete edentia - All-on-4 or All-on-6 protocols.
The doctor decides which method to choose after diagnosis.
Symptoms of periodontitis
A clear clinical picture is characteristic of the acute stage and periods of exacerbation in the chronic form:
- The pain in the initial stages is aching and intensifies when chewing food or pressing on the crown. As inflammation progresses, the intensity of the pain attack increases sharply. The sensations become unbearable, pulsating.
- A feeling of a tooth protruding from the gums. The causal segment becomes higher than other units in the series.
- Presence of deep caries.
- Previous treatment of pulpitis on the causative tooth.
- Swelling of the gums.
- The appearance of an inflammatory tubercle in the projection of the root apex on the gum.
- Formation of a fistula near the diseased segment, discharge of serous or purulent exudate from it.
- Loosening of the unit.
Chronic periodontitis during remission is asymptomatic or has mild symptoms.
Rehabilitation period
You should strictly follow your doctor's instructions. If antibiotics are prescribed, then you need to complete the recommended course. Pain can be relieved with analgesics, swelling can be relieved with a cold compress.
In the first two weeks, careful oral hygiene is important. It is necessary to carefully remove plaque with a soft toothbrush, use dental floss, and rinses. In order not to disturb the injured tissues, it is necessary to eat soft food at a comfortable temperature. It is not recommended to visit the sauna, take a hot bath, or sunbathe on the beach.
Smoking should be stopped for the entire recovery period until the osseointegration process is completed, approximately 4 to 6 months.
What does periodontitis look like?
Osteoporosis
Hypogonadism
Thyrotoxicosis
Diabetes
6370 11 November
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Osteoporosis: causes, symptoms, diagnosis and treatment methods.
Definition
Osteoporosis is a metabolic bone disease characterized by a decrease in bone density as a result of a decrease in the amount of bone substance or insufficient calcification.
“Holes” appear in the bone, making it brittle and prone to damage even with minor mechanical stress
Osteoporosis is a very common disease. In Russia, about 14 million people suffer from it, and osteoporosis is more common in women than in men. The danger of osteoporosis is that the disease does not have characteristic symptoms that would indicate the onset of the process, but knowing certain risk factors and following preventive measures, you can prevent it or alleviate its course.
Causes of osteoporosis
Two opposing processes constantly occur in the bones - the formation and destruction (bone resorption) of bone tissue.
For the effective formation of new bone tissue, building material is required, in the synthesis of which many organs and systems of the body take part: proteins, carbohydrates, fats (the main building material and source of energy), minerals such as calcium and phosphorus, which gives bones density. The endocrine system is involved in the regulation of metabolism and the intensity of the processes of formation and destruction of bone tissue. The kidneys produce active vitamins that help build bones. Thanks to muscles, bone growth accelerates.
If the functioning of at least one link of this complex system is disrupted, the balance of bone tissue formation and destruction occurs.
Many diseases can lead to the development of osteoporosis.
All risk factors for the development of osteoporosis are usually divided into modifiable (those that can be controlled) and non-modifiable (those that cannot be influenced).
Modifiable risk factors include:
- smoking;
- insufficient calcium intake;
- vitamin D deficiency;
- alcohol abuse;
- taking glucocorticosteroids for more than three months;
- low physical activity;
- long-term immobilization (immobility).
Non-modifiable risk factors for osteoporosis include:
- age over 65 years;
- female;
- Caucasian race;
- previous fractures;
- low bone mineral density;
- tendency to fall (due to vision problems, sleep problems, frailty, physical inactivity, or taking medications that cause dizziness);
- heredity (family history of osteoporosis);
- hypogonadism in men and women (decreased production of sex hormones);
- decreased kidney function;
- insufficient body weight.
For patients who have one or more risk factors for osteoporosis, specially designed screening is carried out, thanks to which the disease can be diagnosed at an early stage.
Classification of osteoporosis
There are many classifications of osteoporosis. Currently, a classification is used based on the cause of osteoporosis.
There is a group of primary osteoporosis, which is divided into:
- Postmenopausal osteoporosis (type I).
- Senile (senile) osteoporosis (type II).
- Juvenile osteoporosis (occurs in children).
- Idiopathic osteoporosis (the cause of which cannot be determined).
Secondary osteoporosis develops against the background of one of the diseases:
- endocrine system - Itsenko-Cushing's disease or syndrome (increased production of adrenal hormones), thyrotoxicosis (hyperfunction of the thyroid gland), hypogonadism, hyperparathyroidism (increased production of parathyroid hormones), insulin-dependent diabetes mellitus, polyglandular (when several endocrine glands are involved in the process) endocrine failure;
- rheumatic – systemic lupus erythematosus, rheumatoid arthritis, ankylosing spondylitis;
- organs of the gastrointestinal tract - chronic diseases of the liver and pancreas, malabsorption syndrome (decreased absorption capacity in the intestine), condition after resection (removal of part) of the stomach and intestines;
- kidney – chronic renal failure, renal tubular acidosis;
- blood - leukemia and lymphoma, myeloma (diseases in which the number of certain blood cells increases, including malignant blood tumors), hemophilia (hereditary pathology characterized by a disruption of the blood coagulation system), systemic mastocytosis (increase in the number of mast cells - one type of white blood cell);
- genetic disorders (Marfan syndrome, osteogenesis imperfecta);
- secondary osteoporosis, which developed against the background of other conditions, for example, alcoholism, malnutrition, prolonged immobilization, chronic obstructive pulmonary diseases, organ transplantation, oophorectomy (removal of the ovaries);
- secondary osteoporosis that developed while taking medications.
Symptoms of osteoporosis
Osteoporosis is not characterized by obvious clinical manifestations until the moment of injury.
Thus, we can say that osteoporosis is manifested by its complication, that is, bone fracture in response to even a minor external influence.
After a fracture, typical symptoms appear: pain, swelling, redness and dysfunction of the part of the body where the fracture occurred.
In some cases, fractures can occur unnoticed by a person - for example, compression fractures of the vertebrae, which occur under the influence of the weight of one’s own body, when the vertebrae affected by osteoporosis cannot cope with the load and “flatten”.
Compression fracture of the spine
You can suspect a vertebral fracture due to osteoporosis if:
- acute pain, radiating like radicular pain into the chest, abdominal cavity or thigh, sharply limiting movements, intensifying with minimal movements;
- back pain appeared after falling from your own height or after lifting heavy objects, which does not go away after taking non-steroidal anti-inflammatory drugs;
- height decreased;
- feeling of fatigue in the back after being forced to stay in one position or walking;
- “feeling of heaviness” between the shoulder blades.
Diagnosis of osteoporosis
Physical examination includes:
- measuring the patient's height (a decrease in height by 2 cm or more over 1-3 years or by 4 cm or more compared to the age of 25 years reflects a decrease in vertebral height due to compression);
- measuring the distance between the back of the head and the wall when measuring height (if this distance is more than 5 cm, then we can talk about thoracic kyphosis);
- measuring the distance between the lower ribs and the wing of the ilium (if this distance is the width of 2 fingers or less, then we can talk about shortening of the spinal column due to compression of the vertebrae).
Diagnosis of osteoporosis involves calculating body mass index.
During laboratory and instrumental diagnostics, the cause of osteoporosis is examined: whether the disease is primary in nature or caused by metabolic disorders.
In addition, complications of osteoporosis are being looked for. The doctor prescribes a set of studies, which may include:
- clinical blood test (determining the level of hemoglobin, red blood cells, platelets, leukocytes with calculation of the leukocyte formula);
How to diagnose periodontitis
To determine periodontitis, you need to see a dentist. The doctor will collect anamnesis, conduct an examination using dental instruments, and prescribe additional diagnostics:
- Insertion of the probe into the cavity does not cause pain.
- There is no reaction to the thermal test.
- Percussion causes sharp pain.
- Electroodontodiagnostics. With periodontitis, teeth react to a current of 150 to 200 µA.
- Orthopantomography. In acute serous periodontitis, no radiological changes are observed. Later, the expansion of the periodontal fissure is determined. In an acute purulent condition, a limited abscess is detected. In case of chronic pathology in the apex area, the images show a focus of destruction surrounded by a zone of rarefaction of bone tissue.
Indications and contraindications
With the help of implantation, you can restore a lost dental unit, replace a destroyed tooth that is subject to removal, restore a dental segment or a complete row in case of multiple edentia. It is performed on the upper and lower jaws.
If the patient’s medical history includes a diagnosis of osteoporosis, the doctor makes a decision regarding the possibility of implantation after a thorough diagnosis. For this purpose, a 3D computed tomography is performed. On it you can examine the condition of the jaw bone from any angle and layer by layer. Using a three-dimensional image, the doctor assesses the degree of development of the disease, bone tissue atrophy, and mineral composition.
In the list of contraindications:
- tuberculosis;
- bleeding disorders, blood diseases;
- malignant tumors;
- bruxism;
- mental disorders;
- severe vascular and cardiac pathologies;
- venereal diseases;
- pathological bite;
- acute infections;
- exacerbation of chronic diseases;
- alcoholism, smoking, in which the patient cannot give up cigarettes for a long period;
- pregnancy, lactation;
- exacerbation of chronic diseases;
- low level of immunity.
Some contraindications are temporary and surgery becomes possible after they are eliminated.
What to do if you have periodontitis
If the diagnosis is confirmed, the disease must be treated. How dental periodontitis is treated depends on the form and stage of inflammation. The correction program may include therapeutic and surgical techniques.
Conservative therapy
Conservative methods are aimed at maximizing the preservation of the structure of the unit and restoring its functionality. The program includes elimination of the source of inflammation and endodontic treatment. All manipulations are performed under local anesthesia. Treatment regimen:
- Conducting anesthesia.
- Opening the crown, providing access to the root canals.
- Expansion of the cavity.
- Pulpectomy (if the segment has not been previously treated) or unfilling of the canals.
- Antiseptic, medicinal treatment of cavities.
- Temporary filling (for the period of anti-inflammatory treatment).
- Removal of temporary filling, filling of root canal.
- Restoration of the coronal part of the unit.
- Prescribing a course of antibiotic therapy.
Surgical intervention
Invasive methods are used when other methods are ineffective. The operation can be carried out using different protocols:
- Resection of the apex of the tooth root followed by filling the cavity with special bone-forming materials.
- Extraction of the diseased segment.
If periodontitis is not treated, complications are possible: odontogenic periostitis (inflammation of the periosteum), abscess, phlegmon, etc. The infectious process spreads to nearby lymph nodes, and lymphadenitis occurs. In severe cases, possible: tooth loss, osteomyelitis, sepsis.
Implantation stages
Regardless of treatment protocols, the procedure is performed sequentially. The classic correction method takes a lot of time, and all manipulations using single-phase methods can take only a few days. This period includes diagnostics, surgery to install titanium roots, and prosthetics.
Preparing for implant installation
At the initial appointment, the doctor collects anamnesis, examines the oral cavity, and conducts a computed tomography scan. The patient undergoes blood and urine tests to exclude general contraindications. You may need to seek permission from your physician.
If one or more implants are installed, professional hygienic cleaning of the oral cavity from dental plaque is carried out. When dental diseases (caries, gingivitis, etc.) are detected, appropriate treatment is first carried out.
After diagnosis, the dentist chooses a method of restoring the dentition, implantation systems. If complete edentia is treated with one-stage protocols, then 3D modeling of the result is carried out, and surgical templates are printed.
Performing implantation
The procedure is carried out in stages:
- pain relief with local anesthetics;
- preparing a bed for a titanium root;
- screwing the implant into the bone.
If the tooth is previously removed, the prosthesis is installed on the same day. In this case, special systems are used that can be installed directly into the hole.
The final stage is prosthetics
In the immediate loading protocol, temporary crowns are installed within three days. The permanent prosthesis is installed after at least six months. Some temporary orthotic systems can last up to several years.
With delayed loading, prosthetics are done after the implant has completely healed. In this case, a permanent crown is immediately placed.