Do you want to have healthy teeth and a beautiful smile? Monitor the condition of your gums. Soft tissues perform many important functions, so they must be protected. Proper nutrition, careful grooming and regular dental checkups significantly reduce the risk of developing gum disease.
However, gingivitis, periodontitis and other diseases are not the only causes of gum inflammation. This disorder can also be a consequence of a tooth bruise. Let's look at what leads to injuries and what complications can arise.
Causes of tooth bruises
According to statistics, closed dental injuries are most often encountered by children, adult men and professional athletes. You can get a serious injury:
- when falling or getting hit in the jaw,
- during an accident,
- in a fight
- in training.
The main causes of mechanical damage also include some bad habits:
- bite your nails,
- bite the threads,
- open bottles with teeth
- crack nuts and seeds,
- hold hard objects in your mouth.
This causes damage to the enamel, increasing the risk of serious tooth injury. Bruises are accompanied by aching pain, unpleasant sensations when closing the jaws and loosening of the injured dental unit.
Possible consequences
The most common complications of tooth trauma include gum inflammation. Due to severe mechanical damage, soft tissues become injured and inflamed, which slows down the recovery process. The following negative factors can aggravate the problem:
- decreased immunity,
- lack of vitamins D and group B,
- trauma to the oral mucosa,
- damage to the gums by hard brushes, dental floss or orthodontic appliances.
Inflammation of the gums can be local and generalized. In any case, you should consult a specialist.
Are your gums bleeding? Check your body!
General factors that affect the health of the body as a whole also affect the health of the oral cavity.
Endocrine disorders
This is especially true for women. Any change in the hormonal balance in the body inevitably leads to a complex of systemic disorders, including dental ones. Since the microflora of the oral cavity is very sensitive to any changes and, due to its location, is one of the most vulnerable places in the human body, inflammatory processes due to hormonal imbalance begin almost immediately. Regardless of whether endocrine disruptions are of a natural nature (adolescence, pregnancy, childbirth, menopause) or caused by an endocrinological disease.
Decreased immunity
Vitamin deficiency, infectious or viral diseases, exacerbation of chronic diseases, seasonal weakening of the body - all these factors are fertile ground for the development of a whole complex of pathologies. Infectious and inflammatory processes in the oral cavity against the background of decreased immunity rapidly progress, causing the development of concomitant diseases.
Digestive system disorder
Even the most minor digestive disorders have a negative impact on the health of teeth and gums. First of all, this is due to a change in the composition of saliva, namely the content of enzymes, which, when in excess, begin to corrode tooth enamel and injure the mucous membrane of the gums.
Taking medications
Even taking medications causes my gums to bleed. Medicines can cause harm not only in the form of side effects, but also if they are used incorrectly or if the rules of administration are not followed: chewing the tablet, removing the protective coating, violating the integrity of the protective coating, etc.
Gum injury
In 85% of cases, gum injury leads to the onset of an inflammatory process. If gum bleeding does not stop even after the wound has healed, this is a reason to consult a doctor. With any injury, even a minor one, there is a high risk of infection, and if there are additional prerequisites (for example, poor oral hygiene), the development of infection cannot be avoided. As a rule, the inflammatory process manifests itself almost immediately: the gums bleed, the color changes to bright red, and pain or itching occurs.
When to see a doctor?
You need to make an appointment with a dentist if you have the following symptoms:
- redness and bleeding of the gums,
- mild or intense pain,
- suppuration of soft tissues,
- bad breath,
- discomfort when eating and brushing teeth.
The listed signs indicate gum inflammation. There is no need to wait for them to disappear and put off visiting a doctor. Ignoring warning signs can lead to soft tissue infection, increased tooth mobility, and tooth loss.
What should the patient do?
At home you need:
- rinse your mouth with an antiseptic solution 2-3 times a day
- take pain medication
- there is on the opposite side
- consult a doctor as soon as possible for professional help to avoid the development of complications.
Getting food between the teeth often occurs either due to divergence of teeth during periodontitis, or due to the absence of the lateral part of the tooth when it is fractured or destroyed by caries, or due to shrinkage of the gums and bone due to bone melting during periodontitis or due to the roughness of composite fillings or ceramic crowns in as a result of long-term use.
What should the patient do:
- Try to remove food debris not with a toothpick, but with dental floss,
- Contact your dentist to restore the tooth wall or smooth out the filling and crown.
If you do not pay proper attention to this condition, food debris can get deep into the tissues and cause suppuration.
Gum mobility is one of the unpleasant conditions that causes swelling and pain, as well as the development of root caries.
When you eat, food debris gets deep into the tooth, and trying to remove it causes terrible pain. Brushing your teeth in the morning and evening also causes the gums to shift, which is accompanied by unpleasant sensations.
How to help a person whose gums have become mobile:
- Take liquid food
- Eat on the opposite side
- Use a soft toothbrush
- Brush your teeth with sweeping movements
- Immediately contact a periodontist for a full examination
Treatment of gum inflammation after tooth trauma
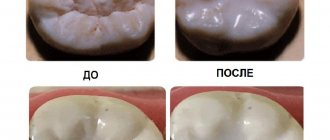
Dentists draw up a treatment plan taking into account the clinical picture, diagnosis and diseases suffered by the patient. To eliminate gum inflammation, experts most often prescribe:
- treatment of soft tissues with anti-inflammatory gels,
- rinsing the mouth with antiseptic solutions,
- professional teeth cleaning.
If there are signs of a bacterial infection, your doctor may prescribe antibacterial medications. They must be taken strictly as prescribed by a specialist. It is also important to use suitable toothbrushes and other personal hygiene products.
Severe pain after removal and surgeon error -
When a tooth has been removed, the gums hurt so much that even strong analgesics help little - the reason most often turns out to be the incompetence of the surgeon. Unfortunately, many surgeons do not strive to minimize trauma to bone tissue and gums during the removal process, which leads to severe pain. Below we list the main medical “flaws” in the process of tooth extraction -
- When cutting out bone with a drill - according to the rules, when cutting out bone around a tooth, the doctor must use a surgical handpiece that supplies coolant to the drilling area.
In 90% of cases, handpieces without such cooling are used in surgical rooms (24stoma.ru). As a result, the bone suffers a thermal burn and superficial necrosis, and the patient suffers acute pain after removal. If you have had a bone cut out and your gums hurt after tooth extraction: what to do in such a situation will depend on the condition of the socket of the extracted tooth. If the clot is dense and there are no symptoms of inflammation other than pain, you should wait and take strong NSAID-based analgesics. If the socket is empty and there are signs of inflammation (see below), you need to go for a second visit to the dentist and clean the socket.
- Sharp edges of the bone stick out from the socket (Fig. 4-5) - if the bone walls have sharp edges after tooth extraction, then they can injure and break through the mucous membrane (Fig. 4), and even stick out from under it. Or if the interradicular bone septum of multi-rooted teeth has a large height, then it may not be completely covered by a blood clot, protruding from under it.
The origin of this problem is that the doctor either did not bite down the sharp edges of the bone and the high interradicular septum with forceps, or did not apply sutures to the too mobile gum around the tooth in order to bring the edges of the wound closer together. The presence of exposed bone fragments can be determined by the characteristic pain when touching such fragments with the tongue, as well as the occurrence of acute pain in response to cold/hot water. Sometimes they can be seen with the naked eye in the mirror.
- Moving bone fragments in the wound - the surgeon can leave large, inactive bone fragments in the socket of the extracted tooth, which are formed when the tooth dislocates/rocks. Their presence can lead to severe pain and inflammation of the extracted tooth socket, as well as the need for a second visit to the surgeon to remove them.
- An incorrect removal strategy is the most common mistake. The fact is that different doctors (due to differences in experience and intelligence) remove exactly the same teeth in different ways. This leads to the fact that one surgeon can torment the patient for 1-2 hours, trying to use only forceps and elevators when removing and regardless of the trauma caused to the bone, while another will decide to immediately saw the tooth into 2 parts (removing them separately), and spending only 15-25 minutes on the entire removal.
- “Empty hole” (Fig. 6) –
if the doctor used too much anesthetic with a vasoconstrictor (this component promotes vasospasm at the site of anesthesia), then the hole after removal may not fill with blood. Doctors usually don't test for this, but simply apply a tampon and send the patient home. In an empty socket, the bone tissue will be exposed and will react with severe pain.
- The doctor did not put sutures - before removal, the mucous membrane around the tooth is peeled off from it with a trowel, which leads to the fact that the edges of the mucous membrane around the socket of the extracted tooth will be mobile.
Often, even seeing the need for suturing, surgeons are too lazy to do it. Ideally, at least 1 suture should be applied even after the removal of small single-rooted teeth, not to mention multi-rooted ones. Studies have shown that suturing the socket can reduce the intensity of pain by 30-50%, reduce the risk of developing inflammatory complications by up to 90%, accelerate wound healing, and almost completely prevent the loss of a blood clot from the socket and the risk of bleeding. I can recommend to you - always, before removal, ask the doctor to suture the hole (even if you have to pay an extra 250-500 rubles for 1 or 2 stitches). This will save you a lot of nerves. - If the doctor does not prescribe antibiotics after a complex removal, there is a high risk of developing inflammation of the socket and, as a result, severe pain. Antibiotics should only be prescribed by a doctor, so you should go for a re-examination and complain about pain.
What to do in all these situations -
How long does the gum hurt after tooth extraction in these situations - normally, pain should last no more than 1-2 days after simple removal, and its severity should be mild or moderate. Moreover, pain, swelling (if it also appears) and other negative symptoms should gradually decrease. After complex removal, pain can be severe and normally last 3-5 days, but starting from the next day they will also begin to decrease.
If the intensity of the pain does not decrease within 2 days, if you feel bone fragments in the wound with your tongue, if you experience pain in the socket when responding to cold/hot water, if a blood clot has fallen out of the socket, if there is an unpleasant odor from the socket... – you need to urgently go to the surgeon for a second appointment (without waiting for your gums to become inflamed after tooth extraction).
Important: in some cases, pain can also be caused by the patient’s mistakes in how he cares for the socket of the extracted tooth. For example, very often patients begin to rinse their mouth intensively, believing that this will be better. But this leads to the blood clot falling out of the socket and causing severe pain. Read about what you can and cannot do after removal in our article: → “Memo for the patient on how to behave after removal”