From this article you will learn:
- structural components of enamel,
- the structure of its organic and inorganic matrix,
- electron microscopy images.
Tooth enamel (enamelum) is the outer shell of the crown of the tooth, representing the hardest tissue in the human body. This hardness is explained by the fact that 95-97% of tooth enamel consists of mineral components (mainly calcium phosphate in the form of hydroxyapatite crystals). Organic matter accounts for only 1-2%, plus about 2-3% water. The strongest are the surface layers of enamel - especially on the occlusal surfaces of the teeth, and towards the enamel-dentin border, as well as when approaching the neck of the tooth - its hardness decreases.
The hardness of enamel is 397.6 kg/mm², which is comparable to quartz. Such hardness allows it to withstand extreme mechanical loads, but on the other hand, it makes it very fragile. The enamel of human teeth does not crack or chip only due to the presence under the enamel layer - a layer of dentin, which has a moderate elasticity coefficient. However, despite its hardness, enamel has good permeability to calcium and fluoride ions contained in saliva (or toothpastes and mouthwashes), as well as to pigments contained in food and drinks.
Structure and development of tooth enamel –
Tooth enamel can have different shades - from yellow to various shades of gray and white, which depends on its transparency coefficient. The more transparent the enamel, the more the underlying layer of dentin, which is physiologically yellow, will be visible through it. In addition, the enamel may have a blue tint - at the cutting edges of the incisors (where there is no underlying dentin layer), as well as at baby teeth. The transparency of enamel depends on the degree of its mineralization and homogeneity, which is associated with the ratio of its organic and inorganic matrices. Transparency also depends on the thickness of the enamel layer.
The thickness of the enamel will vary on different surfaces of the tooth crown. For example, in permanent teeth, the thickness of the enamel ranges from 1.7 to 2.5 mm in the area of the chewing cusps of the molars, and to only 0.01 mm in the cervical part of the tooth (where the enamel borders the root cement). Thus, the closer to the neck of the tooth, the less its thickness will decrease. In baby teeth, the thickness of the enamel will be two times less than in permanent teeth, not exceeding 0.8-1.0 mm.
Composition of tooth enamel
Dental enamel is the most durable, wear-resistant and hard component in the human body. It represents the outer or surface layer of the teeth, completely covers its coronal and partially cervical part, and also performs protective functions. The main characteristics of enamel include:
- The color of tooth enamel varies from white to yellowish, and it can change shade (color) depending on a person’s dietary habits or bad habits.
- The thickest areas of enamel cover the chewing molars in the area of their anatomical tubercles; their thickness varies between 2.3-3.5 mm;
- The thinnest areas of tooth enamel are localized in paroxysmal areas (places of contact in their lateral projection), here the thickness of the protective layer reaches approximately 1.3 mm;
- The enamel that covers all the teeth in the human oral cavity is not capable of regeneration, because there are no living cellular structures in the tissues of this protective layer;
- Depending on the characteristics of each person’s body, up to 95% of the chemical composition of tooth enamel is presented in the form of mineral compounds. The remaining percentage is divided between water and organic matter in approximately a 2:1 ratio, respectively. In addition, depending on the percentage of mineral content of tooth enamel, it can be more or less transparent (the higher the percentage of minerals, the more transparent the enamel becomes).
Development of cement (cementogenesis) –
The formation of cement occurs in two stages. At stage 1, the synthesis of an organic matrix (cementoid or primary cement) occurs. At stage 2, mineralization of the cementoid occurs - with the formation of secondary cement. Let's look at how this all happens.
First, the cells of the dental papilla (as a result of the inducing influence of the epithelial sheath) differentiate into root odontoblasts, which form root dentin. Next, the cementoblasts of the dental sac begin to produce the organic cement matrix (cementoid), as well as collagen fibers and the main amorphous substance. As a result, cementoid is deposited on the surface of the root dentin - in the form of a highly mineralized structureless “Hopewell-Smith” layer (this layer contributes to the strong attachment of cement to the root dentin).
Next, primary cementum, which does not contain cells, is the first to form. It is slowly deposited as the tooth erupts, covering 2/3 of the root surface (closer to the crown of the tooth). Next, mineralization of the cementoid occurs, which is associated with the deposition of phosphates and calcium carbonate. This process occurs in waves, and then in the apical third of the root and the furcation zone, a cell is formed, i.e. secondary cement. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Therapeutic dentistry” (Politun, Smolyar), 5. “Histology of the oral cavity” (Glinkina V.V.).
Other components in the enamel
In addition to the already mentioned main components of the enamel layer of the tooth, its chemical composition also contains a set of other components:
- Neonatal line - present exclusively on baby teeth, it looks like a dark-colored stripe (almost black). This line is located in the area of contact between two types of enamel, the first of which was formed before the baby was born, and the second after.
- Bundles and plates of dental enamel are special enamel formations containing prisms of a hypomineralized type, between which the interprismatic substance consists of the same material. It is noteworthy that the molecular structure of this material involves a large number of protein compounds. Many dentists are of the opinion that through the mentioned bundles and plates, various microorganisms penetrate into the enamel from the oral cavity, making their way to deeper dental tissues, causing caries, etc.
- Gunter-Schräger stripes are lines that stand out on the tooth enamel in a darker or lighter shade, the width of which does not exceed 100 microns. They are located perpendicular to the surface of the enamel layer and are formed as a result of opening its prisms.
- Retzius lines - in shape they resemble arches offset from the central one, located symmetrically in relation to each other. When cut across a tooth , these formations resemble rings inside a tree trunk. The formation of Retzius lines corresponds to different periods of mineralization of the enamel layer.
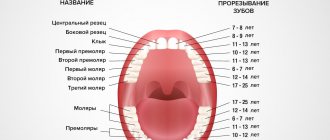
Teething
This stage is characterized by the active movement of temporary teeth from their places of origin inside the jaw until the crown completely exits into the oral cavity. This process is accompanied by active changes in the surrounding tissues, increased development of the root part, restructuring of the alveolar bone structure, as well as the formation and strengthening of the periodontium.
The first temporary teeth, which are usually the lower central incisors, erupt at the age of 5-6 months. Behind them appear the upper antagonists, other incisors and first primary molars. The last to erupt are the lower and upper canines. Typically the process lasts from 4-6 months to 2-2.5 years. With late eruption, the timing of the appearance of temporary teeth shifts from 8-10 months. up to 3.5 years.
Features of the structure of the enamel of baby teeth
The main distinguishing feature of the enamel layer of children's teeth is that it is less durable and also much thinner than the enamel of permanent teeth. This is explained by the lower content of mineral compounds in teeth in relation to water and organic substances. Considering these features, if you examine baby teeth and their enamel layer under a microscope, you will notice the following differences:
- Due to the fact that the service life, as well as periods of mineralization and the tendency towards this process are shorter, the Retzius lines are much less pronounced in the structure of primary dental units.
- If in permanent teeth enamel prisms are located apically, then in milk teeth their direction is completely different, they are located horizontally.
- In children's primary teeth, the final enamel layer is much less pronounced; prisms are clearly visible on its surface, while its structure is much more porous, with microscopic cracks present.
Under the influence of each of these features, tooth enamel in children is more susceptible to wear and damage. For this reason, children develop caries much more often and it progresses faster, which is why it is important to visit the dentist regularly and have their teeth treated in a timely manner.
Topography of cement in the area of the tooth neck –
There are 3 options for connecting cement and tooth enamel. It can be either “joint to joint”, or the cement may extend slightly onto the enamel, or there may be a strip of exposed dentin (Fig. 8). Studies have shown that enamel and cement border “joint to joint” - only in 30% of cases. At the same time, 60% of teeth have a layer of cement on the edge of the tooth enamel (Fig. 9), and a strip of exposed dentin is found in 10% of cases.
Variants of the enamel-cementum boundary (scheme and histology) –
Fig. 8, where 1 – enamel, 2 – dentin, 3 – cement, and options for joining enamel and cement (I – cement partially touches the tooth enamel; II – cement joins the enamel, III – cement does not reach the tooth enamel).
Types of damage to tooth enamel
Over the course of life, even if you provide your teeth with proper care and follow the rules of oral hygiene prescribed by dentists, the enamel layer gradually wears out and is destroyed. This contributes to the occurrence of various diseases of the oral cavity; it is influenced by the food a person eats, etc.
Among the main causes of damage and destruction of tooth enamel, dentists identify:
- Erosion is damage to the enamel layer, and then dentin, which is not associated with carious lesions of the teeth . The essence of this pathological process lies in disorders of mineral metabolism. As a result, disturbances occur in the crystalline structure of the enamel, which is manifested by its focal thinning and destruction. Externally, erosions look like local darkening on a round or oval tooth. The occurrence of erosions is provoked by the consumption of foods with high acidity levels, pathologies of the gastrointestinal tract, the use of certain medications, and the use of aggressive tooth powder or paste.
- Excessive sensitivity of tooth enamel - this disorder is especially pronounced in the form of painful sensations when the teeth cold or hot food, drinks, and even as a result of contact with cool air. The sensitivity of tooth enamel develops due to its thinning under the influence of the factors already described above. A thinned enamel layer puts teeth at increased risk of caries and other dental pathologies.
- Necrosis - this term characterizes multiple lesions of the hard tissues of the tooth, especially the enamel layer and dentin. The pathological process is initially expressed in the appearance of small light spots on the surface of the tooth , which subsequently darken and deepen. The progression of pathology threatens tooth destruction and is accompanied by a number of other oral diseases. The main reasons for the development of necrosis include gastrointestinal diseases, hormonal imbalances, metabolic disorders in the body, and work in hazardous industries.
- Caries is a carious lesion that threatens teeth , primarily affecting the enamel layer of the structure , gradually destroying it and spreading to deeper tissues. There are many reasons for the development of caries, from non-compliance with the rules of oral hygiene and irregular tooth brushing, to pathologies of the structures of the oral cavity, diseases of the gastrointestinal tract and metabolic disorders. If you start caries treatment at the stage when the lesions have affected only the enamel layer, you can only get by installing a filling or even restoring the enamel. But progressive caries is dangerous for teeth due to destruction, which may lead to the need for its complete removal.
- Mechanical damage - due to the fact that the main function of the enamel layer is to provide protection to the teeth , it primarily suffers from the effects of external adverse factors. Mechanical damage to the enamel includes cracks and other violations of its integrity due to blows, bruises, eating too hard food, etc. If the enamel of at least one tooth has been subjected to aggressive mechanical action, you should consult a doctor for an examination and, if necessary, subsequent treatment.
- Wedge-shaped defect – this term characterizes the pathological process in which the area of the dental neck is exposed. In such cases, the thinnest and most vulnerable areas of the enamel layer, located at the base of the teeth, are negatively affected. In addition to visible receding gums, damage to the enamel is indicated by a change in its color, as well as an acute reaction to hot and cold.
Organic and inorganic enamel matrices –
Tooth enamel is quite unique, and in many ways is absolutely unlike other hard tooth tissues. Firstly, enamel is the only dental tissue that comes from the ectoderm (the development of all others is associated with the mesoderm). Secondly, if the organic matrix of other dental tissues is formed mainly by collagen fibers, then the organic enamel matrix does not contain collagen and is formed by the so-called “enamel proteins”. Thirdly, hydroxyapatite crystals in tooth enamel are much larger than in other mineralized tooth tissues.
The last point is that other hard dental tissues continue to be synthesized by cells during the life of an individual (odontoblasts and cementoblasts, respectively), but in mature enamel there are no cellular elements, and therefore, after its maturation, no growth can occur. This is due to the resorption of enameloblast cells during the process of enamelogenesis.
1) Organic matrix of tooth enamel –
We have already said above that the organic matrix of tooth enamel consists of non-collagenous proteins (proteins), which are the product of secretion of enameloblasts, and they are called the term “enamel proteins”. The function of the organic matrix is to adsorb minerals, resulting in the formation of apatite crystals around the enamel proteins. However, as the enamel matures, the organic matrix is almost completely lost.
All enamel proteins are conventionally divided into four types - 1) enamelins and 2) amelogenins, 3) ameloblastins and 4) taftelins. Enamelins are acidic glycoproteins with a large molecular weight, which are characterized by a high content of glycine, serine, aspartic and gamma-carboxyglutamic acids. In turn, amelogenins are hydrophilic glycoproteins (2 times less molecular weight), enriched with proline, leucine, histidine and gamma-carboxyglutamic acid.
Ameloblastins and taftelins occur only during the period of amelogenesis (enamel formation). In addition to enamelins and amelogenins, the organic matrix of mature enamel also contains glycosaminoglycans, proteoglycans, as well as various classes of lipids. All these organic substances are one way or another involved in the processes of mineralization of the organic matrix (protein calcification).
2) Inorganic enamel matrix –
According to research by E.V. Borovsky, tooth enamel contains the following inorganic compounds (average values):
- hydroxyapatite [Ca10(PO4)6(OH)2] – 75.04%
- carbonate-apatite [Ca10(PO4)6(CaCO3)2] – 12.06%,
- chlorapatite [Ca10(PO4)6(Cl)2] – 4.39%,
- fluorapatite [Ca10(PO4)6(F)2] – 0.66%,
- calcium carbonate – 1.33%,
- magnesium carbonate – 1.62%.
These compounds contain about 37% calcium and about 17% phosphorus. Thus, the main mineral salt in the composition of enamel (as well as dentin and tooth root cement) is “calcium phosphate” in the form of apatite crystals, which will additionally contain either hydroxyl residues, or a carbonate group, or chlorine or fluorine. But in addition to these elements and compounds, lead, zinc, aluminum, copper, molybdenum, sodium, strontium, sulfur, tin and titanium are also included in enamel apatite crystals (in extremely small quantities).
In the superficial layers of enamel there are more apatite crystals containing fluorine, lead or zinc, but in the deep layers of enamel their content will be less. At the same time, on the contrary, there will be more apatite crystals containing sodium, magnesium or carbonates in the area of the enamel-dentin junction, and fewer in the surface layers of enamel (24stoma.ru). This "ion gradient" has a certain meaning. For example, apatites with inclusions of sodium, magnesium or carbonates are highly resistant to splitting along the enamel-dentin junction.
More superficially located apatites with inclusions of fluorine, lead and zinc - thanks to these elements, they acquire special strength and resistance to acids. Enamel containing such apatite crystals (such as fluorapatite) is significantly resistant to caries, because fluorapatite begins to degrade at a lower pH value compared to ordinary hydroxyapatite. For example, for ordinary hydroxyapatite the critical pH value will be 5.5, but for fluorapatite – pH 4.6.
In addition, it should be noted that enamel hydroxyapatite crystals (compared to dentin and cement) will have a significantly larger size. For example, in dentin, hydroxyapatite crystals are 20 nm long, 18-20 nm wide, and 3.5 nm thick, which indicates their small size and needle-shaped shape. In turn, in enamel, hydroxyapatite crystals look like hexagonal plates with a length of about 200 nm (but crystals with a size of 500 to 600 nm can also be found), a width of 40–90 nm and an average thickness of 25–40 nm.
Important: due to the absence of enameloblasts in mature enamel, enamel does not have the ability to regenerate (like tooth root cement or dentin). However, despite this, the inorganic enamel matrix is in the process of constant remodeling - thanks to the ongoing processes of mineralization / demineralization. Moreover, the entry of calcium, phosphorus, and fluorine ions into the enamel occurs not only from saliva, but also from the dentin and pulp of the tooth (thanks to the so-called “enamel spindles”).
Strengthening tooth enamel
Today in dental practice there are many effective ways to strengthen the enamel, which allows you to maintain its integrity and prevent destruction and diseases of the dentition. At the same time, methods of strengthening and protecting the enamel layer are divided into two groups, the first are intended for adults, the second for children.
Resorption and preparation for shift
At the age of 5-6 years, the process of completely replacing the temporary bite begins. This period begins immediately after the resorption of milky roots and the beginning of the growth of permanent rudiments. Temporary teeth begin to undergo resorption and ejection from the alveoli. Odontoclasts, which carry out demineralization and intracellular destruction, as well as pulp tissues that secrete osteoclast-like cells, which are responsible for the destruction of dentin and predentin from the internal side, actively participate in the process. Removal of the crown of temporary teeth, as a rule, occurs under the influence of chewing pressure. The root remaining in the hole undergoes a natural process of destruction and resorption. The location of the crown is quickly epithelialized due to granulation tissue.
The process of loss of temporary teeth occurs symmetrically on both jaws and ends with the appearance of permanent teeth. The individual nature of its course is determined genetically.
Strengthening baby teeth enamel
As was said earlier in relation to baby teeth, their enamel is more vulnerable. To protect it, saving the child from premature loss of dental units and problems in the future, doctors perform the following actions to provide temporary protection:
- Fluoridation involves treating teeth with special fluoride-based compounds; it is recommended to repeat this procedure 2-3 times a year.
- Fissure sealing - the dentist performs the procedure of filling the recesses and grooves of chewing teeth with temporary filling material, protecting the dental structures from the negative effects of harmful microorganisms and other unfavorable factors.
- Application gels and preventive mouth guards for teeth - the method is based on enriching the enamel layer with useful components (fluorine, calcium, vitamins) through the use of special products.
Stabilization
This period is characterized by a complete stop of all processes of tissue formation and development. The crown and root reach the required shape, size and level of strength that allows them to perform their basic functions.
The period of stabilization of primary teeth lasts on average 2.5-3 years. At this time, it is important to ensure optimal chewing load on the bite, which will ensure the normal development of facial and other muscles, as well as periodontal tissues and jaw bones. If a child has caries or other diseases, it is during this period that treatment of temporary teeth will be most effective in terms of preserving them, preventing the spread of infection and ensuring normal conditions for changing the bite.
Strengthening the enamel of molars
There are more methods to preserve molars and maintain the condition of their enamel layer. Firstly, this is due to fewer contraindications for adults. Secondly, molars require long-term strengthening.
The main methods of strengthening the enamel of permanent teeth include:
- Drug therapy is based on the use of vitamin complexes containing vitamins of groups B6, B12, D. In addition, the patient is selected drugs that promote better absorption of calcium and fluoride by the body.
- Special gels and oral hygiene products – this technique uses specialized toothpastes and gels containing components necessary for teeth to strengthen and maintain the condition of the enamel layer. Also, teeth are subjected to unimaginative cleaning in a dental office.
- Mineralization and preventive cleaning – mineralization is performed using special means to increase the strength of the enamel and reduce its susceptibility to a number of negative factors. As for cleaning, such procedures are performed by dentists in the clinic using special equipment. During cleaning, plaque and tartar are eliminated , pathogenic bacteria and microorganisms that can harm the enamel layer are removed.
- Home prevention - to maintain healthy teeth and enamel, patients are advised to perform a light massage of the gums, enrich the diet with fresh vegetables and fruits rich in vitamins.
Author: Zhukov M.A.
Teething in children: modern concepts
The eruption of baby teeth in children is a routine process that no individual can avoid. This process is determined by both genetic and environmental factors. Theoretically, innervation-induced pressure in the apical part of the teeth induces the process of eruption, which requires long-term adaptation from the periodontal membrane, as well as active movement of the crown follicle, which destroys the overlying bone tissue.
For many years, discussions have continued among representatives of pediatric specialties regarding teething and its impact on the health of infants [1–3]. Therefore, it was even proposed to consider the so-called “teething syndrome in infants,” which has a corresponding reflection in the International Classification of Diseases, 10th revision - ICD-10 (code K00.7) [2]. Apparently, in the coming years it will find its place in ICD-11.
The opinion of the medical community on the issue of the use of special gels that alleviate the main symptoms that often accompany teething, which will be discussed below, seems equally ambiguous.
The appearance of teeth: just the facts
The formation of teeth occurs approximately on the 40th day of embryonic life. The eruption of primary teeth most often occurs in the second half of the first year of life, usually at the age of 6–8 months.
The order of teething in the first year of life is as follows:
- lower middle incisors;
- upper middle incisors;
- upper lateral incisors;
- lower lateral incisors.
In the latest (20th) edition of the Nelson Textbook of Pediatrics, N. Tinanoff (2016) provides the following information about baby teeth:
- lower middle incisors: first signs of calcification (SCC) - 4.5 months of intrauterine development, crown formation (FC) - 4 months, eruption (E) - 6.5 months;
- upper middle incisors: PPK - 3–4 months of intrauterine development, FC - 4 months, P - 7.5 months;
- upper lateral incisors: PPK - 4.5 months of intrauterine development, FC - 5 months, P - 8 months;
- lower lateral incisors: PPK - 4.5 months of intrauterine development, FC - 4¼ months, P - 7 months;
- lower canines: PPK - 5 months of intrauterine development, FC - 9 months, P - 16–20 months;
- upper canines: PPK - 5.5 months of intrauterine development, FC - 9 months, P - 16–20 months;
- first upper molar: PPK - 5 months of intrauterine development, FC - 6 months, P - 12–16 months;
- first lower molar: PPK - 5 months of intrauterine development, FC - 6 months, P - 12–16 months;
- second upper molar: PPK - 6 months of intrauterine development, FC - 10-12 months, P - 20-30 months;
- second lower molar: PPK - 6 months of intrauterine development, FC - 10-12 months, P - 20-30 months [1].
It is quite natural that the timing and order of teething may differ significantly from those given above (the individual characteristics of this process are often genetically determined). To a certain extent, the timing of teething depends on the gender of the child; in girls it usually occurs somewhat earlier and faster.
According to the proposal of A.F. Tour, to calculate the number of baby teeth that a child aged 6–24 months should have, it is necessary to subtract the number 4 from the number of months of life (actual calendar age) [4].
Currently, it is believed that in the process of teething, it is not so much direct perforation of the gum mucosa by crowns that occurs, but rather an increased production of certain hormones in the child’s body, which cause cell death in the gums, freeing up space for teeth.
The review work by I. Kjær (2014) outlines modern ideas about the mechanisms of the process of primary teething in children, and also presents the author’s own hypothesis, according to which the described physiological process depends on three main factors:
- free space in the path of teething;
- lift or pressure from below;
- adaptability (adaptability) of teeth in the periodental membrane [5].
In general, among the many theories and hypotheses (there are about 500 in total) explaining the mechanisms of teething, only four deserve attention: 1) growth of the tooth root; 2) increased hydrostatic pressure in the periapical zone or dental pulp; 3) reconstruction of bone tissue; 4) periodontal traction [6].
In the Russian Federation, explanations for the mechanisms of teething are usually found in the theories of John Hunter (“root” theory), G. V. Yasvoin (“rocket” theory) and A. Ya. Katz (the theory of pressure of a growing tooth on the side walls of the alveoli), as well as I. G. Lukomsky (theory of simultaneous development of tooth and alveolar bone), which readers can familiarize themselves with if they wish.
The crown follicle destroys the overlying bone tissue and thus provides the necessary space along the teething route. This process depends on the state of the ectoderm in the tooth follicle.
The root shield acts as a glandular membrane, the innervation of which creates excess pressure that forces the teeth towards the surface of the shield, periodontal membrane and pulp tissue. As a result of this pressure, the teeth rise in the direction of eruption.
Problematic teething
On the one hand, many pediatricians believe that the teething process does not cause fever or diarrhea. On the other hand, tens to hundreds of articles report hypothermia accompanying teething, bowel disorders and many other symptoms accompanying this physiological process. In general, the medical community recognizes that teething can be accompanied by pain and increased body temperature (hyperthermia) [1].
The so-called “difficult teething” (dentitio difficilis) may be accompanied by local symptoms (swelling/redness/itching of the gums), general malaise, loss of appetite, hypersalivation, rhinorrhea, restlessness and irritability, nausea, regurgitation/vomiting, sleep disturbances, increased body temperature , dyspeptic symptoms, skin rashes, delay or slowdown in weight gain, etc. [7–10].
As indicated by A.L. Zaplatnikov et al. (2018), a key role in the development of various teething symptoms belongs to pro-inflammatory cytokines (in the gingival fluid during primary teething, the concentration of interleukin-1, interleukin-2 and interleukin-8, as well as tumor necrosis factor α, increases) [2].
The presence of symptoms such as hyperthermia, sialorrhea/hypersalivation, sleep disturbances and irritability in children during the first years of life during teething is confirmed by the work of M. Memarpour et al. (2015), S. Massignan et al. (2016), and M. A. Nemezio et al. (2017), and the last two publications used tools and approaches of evidence-based medicine - a systematic review and meta-analysis [11–13].
Since it has been repeatedly demonstrated over the years that the eruption of primary teeth can be problematic and accompanied by pathological manifestations, there is no doubt about the need to treat these symptoms. For this purpose, paracetamol and ibuprofen (oral or rectal dosage forms), some systemic homeopathic remedies (Viburkol, etc.), as well as special children's gels for gums during teething can be used [14–17].
The most convenient to use are topical gels, which are widely used in many countries around the world.
Teething Gels: Possible Ingredients
Currently, about a dozen products for this purpose are simultaneously presented in the pharmacy network of the Russian Federation. If we try to symbolically classify all the currently available gels for gums during teething, then they can be conditionally classified into one of three categories:
1) synthetic gels (with analgesics/anaesthetics); 2) gels based on natural plant extracts; 3) combined gels: synthetic anesthetics combined with natural plant extracts.
The anesthetics in the described gels are most often lidocaine, benzocaine and/or choline salicylate.
Among the antiseptic ingredients of the gels are cetylpyridinium chloride and cetalkonium chloride.
Other components that may be used are polidocanol (a non-ionic detergent) and trometamol (an anti-acidemic agent); these pharmacological agents provide a predominantly local cooling effect when applied to the child's gums.
Dangerous components of teething gum gels
In 2011, the US Food and Drug Administration (FDA) called for the avoidance of any benzocaine-containing products to treat teething symptoms. This recommendation is based on the risk of developing methemoglobinemia in children under the influence of the described anesthetic. Methemoglobinemia is a rare but very serious condition that can sometimes be fatal.
EJ Ip et al. (2018) asked two hundred pharmacists working in 115 pharmacies in the San Francisco Bay Area (USA) to complete a 16-item questionnaire. The majority of respondents (63.0%) were still inclined to recommend benzocaine-containing gum gels for teething infants [18]. Pediatricians have known about the possibility of acute and chronic intoxication with salicylates contained in teething gum gels for more than forty years.
In 2014, the FDA did not recommend the use of lidocaine in teething gels for children. An overdose of lidocaine rubbed into the gums, or if a child swallows too much of it, may cause seizures, severe brain damage, or cardiovascular problems. There are also cases of accidental poisoning of children with lidocaine during its topical use, sometimes with a fatal outcome.
As it turned out, the use of teething gels is accompanied by a potential risk of developing intoxication due to the content of salicylates in them. This, in particular, is reported in the publications of GD Williams et al. (2011), as well as in the latest works of T. Nguyen et al. (2018) and K. E. Hofer et al. (2018) [19–21].
Since 2014 in the UK, the use of oral gels containing salicylates is not recommended for patients under the age of 16 years, which completely excludes such indications for their use as teething in infants. T. K. Oman et al. (2008) demonstrated a case of the development of Reye's syndrome in a 20-month-old child after using a teething gel with choline salicylate [22]. It is believed that this particular case served as the basis for the corresponding recommendations of the British Commission on Human Medicines (CHM). Although representatives of the Medicines and Healthcare Products Regulatory Agency (MHRA) are inclined to believe that the described case is more consistent not with Reye's syndrome, but with acute salicylate poisoning, the recommendation is not to use oral topical gels with salicylic salts acid is retained.
Due to the fact that all anesthetics without exception (benzocaine, lidocaine, salicylates) included in anesthetic gels can pose a danger to the health and life of children, preference should be given to those topical products that do not contain the components listed above, but natural extracts medicinal plants. A similar point of view is shared by T. V. Kazyukova et al. (2015), I. A. Khoshchevskaya (2013), M. G. Lukashevich (2016), E. I. Kleschenko et al. (2017), as well as E. A. Goreva et al. (2017) [7, 9, 10, 23, 24]. M. G. Shchegoleva writes about the preference of protective gels for gums during teething (2015) [25].
Protective gels versus anesthetic gels
One of the newest concepts in recent years is the use of gum gels during teething, which create a protective film at the site of application and do not contain sugar or parabens. Thus, quite recently S. Rosu et al. (2018) presented the results of a pilot randomized trial (open and controlled) carried out by representatives of a number of Romanian and Italian medical institutions. In the study described, a protective gel for gums was used [26].
This gel was used in 27 children (age 3–36 months) for 7 consecutive days; The FLACC system (Face, Legs, Activity, Cry and Consolability Pain Assessment Tool) was used to assess pain. The presence of teething was determined by at least three signs: local pain, swelling, erythema, hypersalivation and deep characteristics of unerupted teeth. Primary symptoms were assessed at baseline and then on days 3 and 7. In addition, the patients' parents recorded daily changes in crying, oral spasms, salivation, local tenderness, swelling and hyperemia of the gums in the charts. The comparison group consisted of 30 children of the same age, in whose treatment a standard industrial gel was used (containing lidocaine, lauromacrogol 600 and chamomile extract); The same research methods were used as in the main observation group [26].
The results of the study made it possible to demonstrate in children of the main group a significant reduction in the severity of pain and swelling of the gums (from the first to the seventh day, p = 0.034), hyperemia (from the first to the third day - p = 0.045, and from the first to the seventh day - p < 0.001 ), which was confirmed by the records of the patients' parents. When assessing the sum of indicators using the FLACC system, the differences between the observation groups were p < 0.005 (in favor of the main group) [26].
As one of the new representatives of protective gels based on natural ingredients available in Russia, one should consider Dentinale® natura, which is an over-the-counter product. Children's gel for gums during teething Dentinal Nature contains the following herbal ingredients:
- natural extract of boswellia/frankincense tree resin (Boswellia serrata);
- natural extract of chamomile (Chamomilla recutita);
- natural extract of aloe/agagae leaf juice (Aloe barbadensis);
- natural extract of saffron (Crocus sativus);
- Sweet orange peel oil (Citrus aurantium dulcis).
All of these components have a pronounced anti-inflammatory, antiseptic and regenerating effect when the described gel is applied to the gums [27]. Boswellia, in addition to the properties described above, also has analgesic properties [28].
Dentinale nature gel, when applied to the gums, forms a protective film, thereby reducing hypersensitivity, inflammation and irritation of the gums (without the use of analgesics). Additional positive characteristics of the product are the absence of sugar and parabens (esters of parabenzoic acid) in its composition.
Apparently, it should be considered that protective gels based on natural plant extracts (Dentinale Natura, etc.) are not just a full-fledged alternative to products for a similar purpose containing lidocaine, benzocaine and/or salicylates, but are significantly superior to them. Protective gels based on natural plant extracts have better tolerability and, most importantly, a better safety profile, and there are no restrictions on their use.
Literature
- Nelson textbook of pediatrics. Kliegman RM, Stanton BF, St Geme III JW et al., eds. 20th ed. Philadelphia. Elsevier, 2016. 3474.
- Zaplatnikov A.L., Kasyanova A.N., Maykova I.D. Teething syndrome in infants: a new look at an old problem // RMJ. 2018; 5 (II): 68–71.
- Sood S., Sood M. Teething: myths and facts // J. Clin. Pediatr. Dent. 2010; 35(1):9–13.
- Tur A. F. Propaedeutics of childhood diseases. 5th edition. L.: Medicine, 1967. 492 p.
- Kjær I. Mechanism of human tooth eruption: review article including a new theory for future studies on the eruption process // Scientifica (Cairo). 2014; 2014: 341905.
- Pediatric therapeutic dentistry. National leadership / Ed. Leontyeva V.K., Kiselnikova L.P.M.: GEOTAR-Media, 2010. 896 p.
- Kazyukova T.V., Radtsig E.Yu., Pankratov I.V. Symptoms of the eruption of primary teeth and possible ways of pharmacological action // RMJ. 2015; 22: 1342–1344.
- Zakharova I. N., Kholodova I. N., Dmitrieva Yu. A., Morozova N. V., Mozzhukhina N. V., Kholodov D. I. Can the physiological process of teething be pathological? // Medical advice. 2016; 01:31–35.
- Lukashevich M. G. The place of drugs based on plant extracts in alleviating the symptoms of painful teething // RMZh. 2016; 18: 1232–1234.
- Kleshchenko E. I., Zhdanova I. A., Lukisha A. N., Krakovets I. V., Smychkova E. V., Kartavtseva A. V. Symptoms of teething in infants: condition or disease? // Kuban Scientific Medical Bulletin. 2017; 24 (4): 78–81.
- Memarpour M., Soltanimehr E., Eskandarian T. Signs and symptoms associated with primary tooth eruption: a clinical trial of nonpharmacological remedies // BMC Oral Health. 2015; 15:88.
- Massignan C., Cardoso M., Porporatti AL, Aydinoz S., Canto Gde L., Mezzomo LA, Bolan M. Signs and symptoms of primary tooth eruption: a meta-analysis // Pediatrics. 2016; 137(3):e20153501.
- Nemezio M.A., de Oliveira K. Mh., Romualdo PC, Queiroz A.M., Paula-E-Silva F. Wg., Silva R. Ab., Küchler E.C. Association between fever and primary tooth eruption: a systematic review and meta-analysis / /Int. J. Clin. Pediatr. Dent. 2017; 10 (3): 293–298.
- Shelkovsky V.I., Studenikin V.M., Pak L.A., Tursunkhuzhaeva S.Sh. Nonsteroidal anti-inflammatory drugs in pediatric practice // Attending Physician. 2011; 11:82–84.
- Studenikin V.M., Tursunkhuzhaeva S.Sh., Shelkovsky V.I. Ibuprofen and its use in pediatrics and child neurology // Issues. pract. pediatrics. 2010; 5 (5): 140–144.
- Studenikin V.M., Akoev Yu.S. Antipyretics/analgesics in modern pediatrics: allopathy and homeopathy // Attending Physician. 2016; 6:7–11.
- Taneja D., Khurana A., Vichitra A., Sarkar S., Gupta AK, Mittal R., Bawaskar R., Sahoo AR, Prusty U., Singh S., Sharma M., Pant R., Singh U., Upadhyay AK, Sehegal S., Patnaik S., Nath T., Manchanda RK An assessment of a public health initiative of homeopathy for primary teething // Homeopathy. 2018; Nov. 20. DOI: 10.1055/s-0038–1673650. .
- Ip EJ, Patel PB, Chi JJ, Shah-Manek B., Lau B. What are pharmacists recommending for infant teething treatment? // J. Am. Pharm. Assoc. 2018; 58(1):79–83.
- Williams GD, Kirk EP, Wilson CJ, Meadows CA, Chan BS Salicylate intoxication from teething gel in infancy // Med. J. Aust. 2011; 194(3):146–148.
- Nguyen T., Cranswick N., Rosenbaum J., Gelbart B., Tosif S. // J. Paediatr. Child Health. 2018; 54(5):576–578.
- Hofer KE, Kaegi S., Weiler S. The acute toxicity profile of a teething gel containing salicylamide in toddlers: an observational poisons center-based study // Clin. Toxicol. (Phila). 2018; 16:1–2.
- Oman TK, Stewart MC, Burns A., Lang TF Topical choline salycilates implicated in Reye's syndrome // BMJ. 2008; 336:1376.
- Khoshchevskaya I. A. Teething: how to help a child? // Medical advice. 2013; 2:36–40.
- Goreva E. A., Petrenko A. V., Babailov M. S. The use of herbal preparations for teething syndrome in children // Health and education in the XXI century. 2017; 19 (10): 71–73.
- Shchegoleva M. G. Comparative assessment of means that facilitate teething // Medicine today and tomorrow. 2015; 2 (67): 142–146.
- Rosu S., Barattini DF, Murina F., Gafencu M. New medical device coating mouth gel for temporary relief of teething symptoms: a pilot randomized, open-label, controlled study // Minerva Pediatr. 2018; Oct. 4. DOI: 10.23736/S0026–4946.18.05360–4. [Epub ahead of print].
- Nutrients, conditional nutrients and antinutrients in neurodietology of childhood (handbook) / Ed. Studenikina V. M. M.: Dynasty, 2016. 184 p.
- Prabhavathi K., Chandra US, Soanker R., Rani PU A randomized, double blind, placebo controlled, cross over study to evaluate the analgesic activity of Boswellia serrata in healthy volunteers using mechanical pain model // Indian J Pharmacol. 2014; 46(5):475–479.
V. M. Studenikin , Doctor of Medical Sciences, Professor, Academician of RAE and MAE
OOO NPSMC "Dream Clinic", Moscow
Contact Information
Teething in children: modern concepts / V. M. Studenikin For citation: Attending physician No. 1/2019; Page numbers in the issue: 7-11 Tags: baby teeth, fever, hypersalivation, itchy gums