The development and formation of teeth is the longest process of organogenesis in the human body: starting from the 28th day of gestation with the formation of the primary epithelial cord, it ends by the age of 18-25 years with the completion of the formation of the roots of the third molars. The formation of roots begins in the postembryonic period shortly before eruption and continues for another 2-3 years after the start of eruption [1].
Normally, in the early stages, tooth root formation is carried out by cells of Hertwig's epithelial root sheath (HERS), which consists of two rows of enamel organ cells. Cells of the inner layer of the root sheath induce the differentiation of peripheral mesenchymal stem cells of the dental papilla into odontoblasts, which ensures the formation of dentin of the tooth root [2]. As the root grows, the dental papilla is reduced and in later stages these cells are present only in the apical part of the tooth root, the so-called apical papilla [3]. Stem cells of the apical papilla are able to differentiate into primary odontoblasts and ensure the formation of dentin in the tooth root [4]. After HERS reduction, poorly differentiated mesenchymal cells of the dental sac come into contact with root dentin and differentiate into cementoblasts, which ensures the histogenesis of tooth root cementum [5].
It is assumed that if the dental pulp is damaged, physiological root growth is possible only if the vital pulp is preserved in the apical part of the tooth root and the cells of the apical papilla and root sheath are preserved. In a study by Domenico Ricucci et al. (2017) it was found that with a long-term irreversible inflammatory process, as well as with pulp necrosis, the integrity of the apical papilla and HERS are disrupted, which makes further physiological apexogenesis impossible even with proper treatment. However, the same authors noted that in teeth with unformed roots, the preservation of viable pulp in the middle and apical parts of the tooth root is possible even in the presence of a focus of clearing in the periapical tissues, which is usually considered as a symptom of the death of the neurovascular bundle [6].
In addition to the wide lumen of the apical foramen and the absence of anatomical apical narrowing, the early stages of root growth are characterized by small thickness and low strength of the walls of the root canal due to the low degree of mineralization of root dentin [5]. That is why the main task of the doctor in case of pulp necrosis in teeth with unformed roots is to bring artificial apexogenesis as close as possible to physiological one. It is optimal if therapeutic measures stimulate the growth of the root in length to ensure the stability of the organ in the dentofacial system and create optimal conditions in case of need for further orthopedic restoration, provide an increase in thickness of the tooth root tissue to prevent the development of tooth root fractures with the formation of an apical part close to the natural one tooth root. At the same time, it is also desirable to complete the treatment in the shortest possible time with the fewest number of visits.
Several techniques are used for apexification (artificial formation of the apical part of the tooth root). The main procedure used is the classic procedure of apexification with calcium hydroxide, proposed back in 1964 and involving long-term exposure of a highly alkaline root dressing in the root canal in order to stimulate the formation of a calcified barrier in the area of the apical foramen, mainly due to the activation of alkaline phosphatase and pyrophosphatase, which take direct action participation in the mechanisms of bone formation and mineralization of newly formed tissue [5]. The shape of the solid tissue barrier is variable, with the following options described in the literature: cap, bridge, or ingrown wedge. Histologically, the newly formed tissue is represented by cementum or dentin-like tissue (“osteodentin”) [7]. According to the literature, the creation of a solid tissue barrier requires from 6 to 24 months [8].
However, this technique has a number of disadvantages. Exposure of calcium hydroxide in the root canal for more than 180 days increases the risk of root fracture and resorption due to drying of root dentin. After 12 months of calcium hydroxide remaining in the root canal, the elastic modulus of bark dentin decreases by 2 times, which also reduces resistance to fractures [9–11]. In addition, high cooperation on the part of patients is required due to the frequency of appointments and duration of treatment, while the risk of reinfection is high due to the possible failure of temporary restoration, which further prolongs the treatment period and worsens its prognosis [8].
As an alternative to the calcium hydroxide apexification method, it has been proposed to create a 3-4 mm MTA plug in the area of the open apical foramen. This technique also has a number of limitations: firstly, it can only be used at the last stages of root formation and in the absence of pronounced destruction of periapical tissues [9], secondly, the formation of an apical plug from MTA does not in any way affect the growth of the root in length, nor the thickening of the root walls; accordingly, they also remain susceptible to fractures [12].
A relatively new, insufficiently studied, and therefore less common method of treating teeth with immature roots is the use of regenerative endodontics - the so-called revascularization or pulp-like tissue regeneration (RPT) technique. RST is based on the principles of tissue engineering and is defined as a set of biological interventions aimed at replacing damaged structures, including dentin and other elements of the tooth root, such as pulp cells and the vascularized pulp-dentin complex, with tissue, preferably of similar origin, which allows for further root growth and tooth function [13]. According to the literature, in animal experiments, as well as according to the results of individual x-ray studies, this technique gives a greater increase in root dentin compared to apexification techniques with calcium hydroxide and the creation of an apical barrier from MTA, and the newly formed apical part of the tooth is histologically closer to the physiological structure of the tooth root [14].
The purpose of the study was to compare the effectiveness of apexification with Ca(OH)2 and regeneration of pulp-like tissue in the treatment of children with pulp necrosis in incisors with immature roots.
What does it represent?
Apexification is a labor-intensive process. The duration of execution directly depends on the qualifications of the doctor and strict adherence to the sequence of actions.
Various medical technologies are used to close the root tip. The most effective method is considered to be the sequential replacement of artificially installed materials in the formed root canal. As a rule, materials containing calcium are used to carry it out.
There is another method by which apexification is carried out. It consists of using the Pro Ruth MTA material. It has full biocompatibility with natural tissues, which has been confirmed by many medical tests, and is therefore widely used in pediatric dentistry.
Results and discussion
The average duration of apexification with calcium hydroxide depending on the stage of Tsweku root formation is presented in Fig. 1 . The duration of formation of the apical barrier ranged from 5 to 21 months, while in 56% of cases the duration of treatment exceeded 12 months.
Rice. 1. Median duration of apexification with calcium hydroxide depending on the stage of root formation at the time of pulp necrosis.
Treatment took less than a year only for stage III of root formation; accordingly, the prognosis of this group is better with regard to the resistance of the root walls to fractures in the long term.
Clinical and radiological characteristics of patients in the prospective study, as well as data on treatment outcomes and the growth of hard tissues of the roots of the teeth are presented in Table. 1 and 2 .
Table 1. Dentin growth of the tooth root after using the apexification technique with calcium hydroxide
| Age at time of injury (months) | Tooth number | Nature of injury | Root Formation Stage | Estimated duration of the inflammatory process | Duration of apexification (months) | Crown length/root length ratio before treatment | Crown length/root length ratio after treatment | The ratio of the total root size in thickness to the lumen of the root canal before treatment | The ratio of the total root size in thickness to the lumen of the root canal after treatment |
| 77 | 2.1 | Incomplete lateral dislocation | II | 36 months | 7 | 1,09 | 0,8 | 2,33 | 2,6 |
| 2 | 3 | ||||||||
| 2,5 | 1,75 | ||||||||
| 83 | 1.1 | Uncomplicated crown fracture | III | 2 weeks | 6 | 0,83 | 0,78 | 2,5 | 3,5 |
| 2,6 | 2,6 | ||||||||
| 2,25 | 3 | ||||||||
| 95 | 4.1 | Uncomplicated crown fracture | III | 2 months | 5 | 0,33 | 0,33 | 2,33 | 3,25 |
| 3 | 3,66 | ||||||||
| 2,25 | 9 | ||||||||
| 126 | 1.1 | Complicated crown fracture + incomplete lateral dislocation | IV | 2 weeks | 11 | 0,5 | 0,5 | 2,46 | 3,2 |
| 2,27 | 2,9 | ||||||||
| 3 | 3 | ||||||||
| 94 | 1.1 | Complicated crown fracture | II | 2 days | 12 | 0,33 | 0,29 | 2,6 | 2,4 |
| 1,83 | 2 | ||||||||
| 2 | 2 | ||||||||
| 120 | 2.1 | Uncomplicated crown fracture | III | 9 months | 10 | 0,5 | 0,39 | 2,2 | 2,5 |
| 2,5 | 2,67 | ||||||||
| 2,5 | 2 |
Table 2. Growth of dentin in the root of the tooth after applying the technique of regeneration of pulp-like tissue
| Age at time of injury (months) | Tooth number | Nature of injury | Root Formation Stage | Estimated duration of the inflammatory process | Deadline for root growth (months) | Crown length/root length ratio before treatment | Crown length/root length ratio after treatment | The ratio of the total root size in thickness to the lumen of the root canal before treatment | The ratio of the total root size in thickness to the lumen of the root canal after treatment |
| 113 | 2.1 | Complicated crown fracture | III | 2 weeks | 18—24 | 0,56 | 0,54 | 2,33 | 2,33 |
| 2,8 | 2,8 | ||||||||
| 2,75 | 3,66 | ||||||||
| 89 | 1.1 | Incomplete impacted dislocation | II | 60 months | 6—12 | 0,76 | 0,73 | 1,75 | 2,15 |
| 1,5 | 2 | ||||||||
| 1,67 | 3,5 | ||||||||
| 100 | 1.1 | Complicated crown fracture + incomplete lateral dislocation | II | 12 months | 12—18 | 0,47 | 0,42 | 2,3 | 2 |
| 2,67 | 2,33 | ||||||||
| 2 | 2,66 | ||||||||
| 87 | 1.1 | Uncomplicated crown fracture | II | 6 months | 12—18 | 0,76 | 0,75 | 2,08 | 2 |
| 2,5 | 3,25 | ||||||||
| 1,8 | 3,3 | ||||||||
| 92 | 2.1 | Complicated crown fracture | II | 2 months | 12—8 | 0,78 | 0,69 | 2 | 2,5 |
| 2,33 | 2,25 | ||||||||
| 2 | 2,33 | ||||||||
| 79 | 2.1 | Complete dislocation | II | 36 months | 12—18 | 1,14 | 1 | 1,33 | 2 |
| 1,33 | 2 | ||||||||
| 2 | 4 |
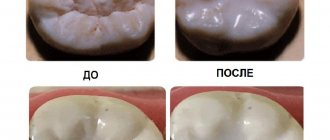
All patients showed healing of the OPPT both after apexification and after RPT. Root formation in group 1 took from 5 to 12 months and from 4 to 6 visits. After completion of the RPT protocol, root formation in group 2 took from 12 to 18 months. An increase in root length was observed in 83% of all cases, but the pattern of growth of root dentin was different in the groups. The increase in root dentin thickness in the RPT group was more pronounced in the apical third of the root canal and was observed in 100% of cases, while in group 1, dentin thickness increased mainly in the coronal and middle third of the root, and the increase in hard tissue in the apical third in the group apexification was observed in only 33% of patients (Table 3) . At the same time, in some cases, we were faced with the impossibility of permanent filling of the root canal evenly along the entire length after the apexification procedure with calcium hydroxide in the presence of a clinically detectable hard tissue barrier (Fig. 2) .
Table 3. Growth of hard dental tissues after treatment of patients with pulp necrosis in teeth with immature roots in the apexification groups with calcium hydroxide (group 1) and RPT (group 2)
| Total | 1st group | 2nd group | |
| 12 | 6 | 6 | |
| Growth of tooth root tissue along the length | 10 (83%) | 4 (67%) | 6 (100%) |
| Growth of root dentin in thickness in the coronal third | 8 (67%) | 5 (83%) | 3 (50%) |
| Growth of root dentin thickness in the middle third | 8 (67%) | 6 (100%) | 2 (33%) |
| Growth of root dentin in thickness in the apical third | 8 (67%) | 2 (33%) | 6 (100%) |
Rice. 2. Sight radiographs of patients after the formation of the apical barrier and permanent obturation of the root canals.
a — formation of a mineralized barrier at the border of the middle and apical third of the tooth root; b — permanent filling material is shifted to the distal wall, the lumen of the root canal is unevenly changed.
This can be explained by the “quality” of the apical barrier formed during apexification with calcium hydroxide. Histological study of Maha MF Mounir et al. (2018) showed a difference in the quality of the newly formed attachment after apexification with calcium hydroxide and RPT: in the first case, the apical part of the tooth root was represented by dentin-like mineralized tissue with islands of calcification in the lumen of the root canal and was separated from the bone tissue by a layer of granulation tissue even after 6 months observations, after applying the RPT technique, the formation of a layer of tubular dentin in the apical third was observed, islands of calcifications were present in only 5% of cases, and the dentin bridge was surrounded by newly formed periodontal ligament, although dental pulp tissue was not found in the lumen of the root canal in any sample [ 16].
In most cases, a hard tissue barrier is formed at the point of contact of the root dressing with adjacent tissues, which leads to a change in the shape of the root canal, the formation of calcifications in the lumen of the root canal, and also limits the length of the canal at the level of calcium hydroxide.
According to the literature, apexification with Ca(OH)2 ensures the formation of a barrier in the apical part of the tooth root, however, complete closure of the apex of the tooth root can be achieved only in 10.8% of cases [16]. CBCT data after the apexification procedure in our study showed a picture of incomplete closure of the tooth root apex during the formation of the apical barrier (Fig. 3) .
Rice. 3. CBCT of teeth 1.1, 2.1 after 12 months of apexification with calcium hydroxide.
The formation of a hard tissue barrier is visualized at the border of the middle and apical third of the root canal in tooth 1.1; in tooth 2.1, the formation of an apical barrier in the form of a “cap” with a significant defect in the newly formed tissue from the palatal surface of the tooth root is noted.
The growth of hard tissues in the RPT group was not always accompanied by the formation of a radiologically complete root. According to the results of our previous analysis of the outcomes of tooth dislocations accompanied by pulp necrosis, continued root growth during RPT occurs only in 70% of cases [17]. We observed the formation of a radiologically complete root during early treatment after the onset of periodontitis (Fig. 4) . In the presence of a pronounced radiological focus of clearing in the periapical tissues, indicating the duration of the inflammatory process, after treatment, healing of the OPPT was noted, but the growth of hard tissues in the apical part of the tooth root was insignificant and atypical (Fig. 5) .
Rice. 4. Targeted contact radiograph of teeth 1.1, 2.1.
Tooth 1.1 - 2.5 years after high pulp amputation, tooth 2.1 - 2.5 years after RPT. The estimated duration of the inflammatory process before starting treatment is 2 weeks. The formation of a conical root is observed, the course of the root canal can be traced throughout, the periodontal gap is uniform throughout the entire length of the tooth root.
Rice. 5. Sight X-ray images of tooth 2.1, clinical diagnosis: tooth dislocation, chronic periodontitis, pathological resorption (external).
a - before treatment, there is an extensive OPST, an area of external tooth root resorption; B - after RPT; B — 6 months of observation; D — 21 months of follow-up, complete healing of OPPT, no progression of resorption observed.
During a longer period of observation, we noted the following complications in individual clinical cases.
Clinical case 1
A 10-year-old patient presented one month after the injury. Tooth 1.1 clinical diagnosis S03.2 Tooth dislocation (impacted), K04.5 Chronic periodontitis. Stage of tooth root formation - III. Treatment was carried out using apexification with calcium hydroxide. Duration of treatment - 11 months. 4 months after permanent filling of the root canal, a control radiograph revealed an oblique transverse fracture of the tooth root (Fig. 6) .
Rice. 6. Sight X-ray images of the tooth 1.1.
a — after permanent filling of the root canal; b - after 4 months.
Clinical case 2
An 8-year-old patient presented 3 weeks after the injury. Tooth 1.1 diagnosis S03.2. Dislocation of tooth (impacted), S02.5. Tooth fracture (complicated). An apexification technique with calcium hydroxide was performed, however, during the treatment process, low cooperation on the part of the patient and her parents, missed appointments, and non-referral of the patient in cases of loss of temporary restorations were noted. During the year, no positive dynamics in the formation of a calcined barrier were observed; it was not possible to create an apical plug from MTA. It was decided to conduct RPT in one visit. Then the patient came back 30 months after RPT with complaints of re-injury and loss of permanent restoration. X-ray examination revealed extensive OPPT. In the absence of tightness, reinfection of the blood clot in the lumen of the root canal occurred and the development of chronic apical periodontitis. After disinfection, the root canal was filled with MTA along its entire length due to partial resorption of the apical part of the root and a decrease in the length of the root - 7 mm from the mouth of the root canal (Fig. 7) . The patient is currently under medical observation.
Rice. 7. Sight X-ray images of the tooth 1.1.
a — after RPT.; b — 30 months after reinfection of the root canal; c — after filling the root canal with MTA.
Clinical picture
Most dentists are unanimous in the opinion that therapeutic measures aimed at preserving the dental pulp are the treatment of developing immature teeth that are located on the pulp.
The apexogenesis technique allows the dentist to continue root formation and provide apical closure. Previously, two medications were used for the procedure. Despite the fact that the list of analogues has expanded, they are still used today.
- USP (calcium hydroxide). A popular remedy used for this therapeutic event. It allows you to preserve the vital activity of the pulp and is widely used in many dental clinics. To date, this drug is considered the most effective. It can be used to achieve maximum intensity during biocoating of the natural dental nerve.
- MTA (mineral trioxide). Some doctors consider this drug to be a real endodontic find, since it can be used in various clinical cases, and also has isolating properties.
Other drugs are also used in dental practice.
Ways to achieve successful apexification
In case of damage to the growth zone when treating teeth with incomplete root development, it is very important to be able to form a dense barrier in the area of the canal apex. This process is called apexification. The main materials for growing the barrier are osteodentin, acellular or cellular cement, bones or bone-like tissues. Very rarely it covers the entire apical part of the root. Most often, the barrier maintains communication between the periapical tissues and the internal cavity of the tooth.
Achieving successful apexification is carried out in two ways: multi-step and one-step. In both cases, the children's dental clinic first performs a standard set of preparatory work. It includes wide opening of the cavity, cleaning the walls using 35-50 size files, and thorough but gentle rinsing of the canals. Next, the specialist carries out specific manipulations based on the chosen apexification method.
- Multi-step. In this case, the treated canals are obturated with pastes based on calcium hydroxide, which are delivered to the treatment area using a plugger, canal filler, syringe, amalgam tregger and other instruments. The cavities are first thoroughly dried with paper points. After filling the canals, the crown is sealed with glass ionomer or zinc oxide-eugenol cement. After 30 days, calcium hydroxide is replaced. After about 3-6 months, an x-ray examination is performed to determine the presence or absence of a dense barrier bridge in the apical part of the tooth.
- One-step. This method of apexification involves obturation of the apical zone of the root canal with MTA preparations. Within a few hours, the material hardens completely, after which a permanent tooth filling is performed. This method is used for endoparadontal lesions, the inability to prolong treatment, the insufficient effectiveness of other drugs for apexification, as well as when it is impossible to ensure reliable sealing of a temporary filling and in other cases.
Regardless of the condition of the tooth and the chosen treatment technology, permanent root canal filling can be carried out only after the process of forming a dense and durable apical barrier in the area of the root apex has been completed.
Diagnostics
In some cases, the diagnosis of pulp necrosis is accompanied by certain difficulties. We are talking about those teeth in which the root apex is not yet fully formed.
Pathologies can occur due to physical trauma. Taking a patient's history is considered to be of paramount importance during diagnostic workup and subsequent treatment.
The possibility of radiographic examination is limited by the fact that at the root apex it is possible to view the radiological clearing. Electrical methods for assessing the condition of the dental nerve of units with incompletely formed roots, as a rule, do not bring the desired results.
During diagnostic procedures, it is important to take into account the patient’s pain threshold, changes in the color of the crown and other factors. Opening a problematic tooth can only be done if there are no contraindications. Timely tooth restoration allows you to avoid the subsequent development of an infectious process in the pulp.
Features of apexogenesis
Most specialists in the field of dentistry agree that treatment procedures based on preserving the vitality of the pulp are a therapy for the emerging immature teeth located on the vital pulp.
With apexogenesis technology, the dentist is given the opportunity to continue root formation and apex blocking. Until recently, two main drugs were used to form the dental apex:
- Calcium Hydroxide USP . It is considered a popular means for this type of treatment while preserving living pulp and is still used in clinics in many countries around the world. This product ensures intensification of the process of biological coating of dental pulp. A drug that exceeds this one in terms of biocompatibility characteristics has not yet been developed.
- Mineral trioxide (MTA) . According to some doctors, it is considered a real endodontic miracle material that can be used in various situations. This is a reliable insulating agent.
Many other drugs are used today.
Diagnostic measures
In some situations, problems may arise with diagnosing pulp necrosis in those teeth in which the upper part of the root has not fully formed.
In most cases, such disorders occur as a result of physical trauma. Obtaining detailed information about the history of the injury is considered a matter of paramount importance in the process of diagnostics as well as treatment procedures.
The process of X-ray diagnostics in this situation can be complicated by the fact that during the process of root formation, where its apex is located, an area of X-ray clearing can be seen.
In this case, it is necessary to carry out a detailed comparison of the formation of the root of the diseased tooth with a symmetrical tooth located on the other side of the jaw.
Methods of testing dental pulp with incomplete root formation through electrical testing in most cases do not bring the desired results.
In the process of carrying out diagnostic procedures, it is advisable to take into account the presence of severe or chronic pain, changes in the color of the crown, the body’s positive reaction to intense percussion, and general tooth mobility before opening the dental cavity.
Such measures are necessary in order to ensure the development of necrosis in the pulp. Tooth restoration is necessary in order not to contribute to the further development of infection in the pulp.
Prevention of gum disease in children
Experts are confident that you can completely avoid gum disease if you follow 5 rules:
- Teach your child to chew food correctly with all chewing teeth.
- Show your child the correct technique for brushing teeth and additional flossing.
- Eliminate malocclusions in a timely manner and select orthodontic appliances.
- Do not give your child too cold or hot food (temperature no more than 30o C).
- Use a fingertip to stimulate the gums as baby teeth emerge.
Forms of gum inflammation in children
Parents whose children suffer from various forms of gum inflammation come to our clinic. The most common of these is gingivitis. This disease occurs as an inflammation of the gum mucosa and has the following symptoms:
- bleeding gums;
- swelling of the interdental papillae;
- painful symptoms when brushing teeth.
If not treated promptly, gingivitis can develop into a more serious form - periodontitis. And its treatment often requires surgical intervention. In addition, inflammation of the gums can lead to the appearance of fistulas on the gums of a child, and this phenomenon also requires immediate treatment by a professional dentist.
Periodontitis is an inflammation that, in addition to the gum mucosa, also covers other tissues and causes bleeding and loosening of teeth, and can also lead to the appearance of periodontal pockets.
If a child’s diet is not balanced and his body does not receive enough vitamins and minerals, dystrophic periodontal disease may occur: periodontal disease. Cases of its occurrence in children are quite rare, and treatment should be carried out in a complex manner.
What gum diseases occur in children?
Dystrophic – represent tissue atrophy caused by crowded teeth or malocclusion. The disease is localized in only one place (usually near the fangs and incisors). There is no burning sensation or pain, so treatment begins already at a severe stage. By that time, the root of the tooth is exposed, pain and increased sensitivity appear.
But children do not have such severe pathologies as periodontal disease. These are rare cases that progress with a lack of vitamins and diseases of the immune system. If treatment is not started, gums and bone tissue will be reabsorbed. Therefore, molars will have to be removed, since it is impossible to save them at a severe stage.
Inflammatory – this is gingivitis, which in severe stages turns into periodontitis. Treatment must begin immediately, because in the future the bone tissue, jaws, and ligaments may become inflamed. Despite the rare occurrence in children, a visit to the dentist should not be put off. The chronic form of periodontitis cannot be treated and persists for life. If treatment is delayed, periodontitis may progress to a granulating form, accompanied by the appearance of fistulas on the gums. Complications of the pathology can be identified by visual examination (inflammation spreads from the gums to the teeth).
Risk factors
Common risk factors are diseases:
- Of cardio-vascular system.
- Hormonal system.
- Immunity.
- Gastrointestinal tract.
- Respiratory system.
Diseases often develop against the background of a lack or excess of vitamins and allergic reactions to medications or foods.
Local risk factors in most cases are associated with pathogenic bacteria that accumulate on the enamel. This occurs due to irregular or improper brushing of teeth. Gradually, the plaque becomes hard, which leads to gum inflammation.
A high probability of progression of gingivitis occurs during the period when baby teeth appear. Pathologies are formed due to increased load on the jaw. An abnormal bite develops, leading to injury while eating.
If you notice redness, increased bleeding or swelling of the gums, do not delay a visit to the pediatric dentist. He will choose the right treatment strategy during an in-person consultation.