Painful sensations in the larynx are one of the signs of diseases of the respiratory organs. Infectious diseases of the upper respiratory tract in children are diagnosed 3 times more often than in adults. As a result, pain in the throat area is a fairly common problem at an early age. In addition to a sore throat, respiratory diseases in childhood are most often accompanied by symptoms such as a runny or stuffy nose, red eyes, fever and weakness. Such manifestations are usually evidence of the development of a serious pathology. If pain in the larynx occurs, you should urgently consult a doctor to establish a diagnosis and prescribe the correct therapy.
A child has a sore throat: what and how should parents do in this case?
consultation with a pediatrician at a medical center Sore throat is one of the common reasons for outpatient and emergency visits by parents of children to doctors for help. Upper respiratory tract infections are very common in both children and adults and have significant economic consequences associated with the frequent prescribing of antibiotics by physicians, even when the causative agent is not bacteria. About a quarter of children suffering from tonsillitis also suffer from bacterial pharyngitis. Identification and adequate antibiotic treatment of group A streptococcal sore throat is important for the primary prevention of acute rheumatic fever, which occurs in 3% of cases. Therefore, in any case, if you have a sore throat, you need to show your child to a doctor to rule out diseases that are dangerous to health and life.
Actions before visiting a doctor
Before seeking medical help, it is recommended:
- Maintaining bed rest. This will make it easier for the body to withstand the increase in temperature and recover.
- Drinking plenty of fluids to speed up the elimination of pathogens from the body through sweat, saliva and urine. Moreover, you can drink not only water, but also warm tea (berry tea is best - raspberry, currant, lemon), compotes, herbal decoctions. When making lemon tea, do not put too much citrus in the drink. You should not give a child with a sore throat soda and sour drinks, as this is fraught with additional painful manifestations in the throat.
- Following a “gentle” diet. The child should eat often, and the portion should be small. During treatment, you need to avoid rough and spicy foods and minimize sweets.
- Gargling. In such a situation, it is better to use gentle herbal infusions, the raw materials for which are sold at any pharmacy. For rinsing, it is recommended to use products based on sage, chamomile, calendula, linden blossom, and eucalyptus. You can prepare the infusion yourself. To do this, you need to pour 3-4 teaspoons of the herb with hot water in a volume of 500 ml and leave to infuse for at least half an hour. It is necessary to gargle before or after eating food. The duration of the procedure is 2-3 minutes. After rinsing, eating and drinking is prohibited for half an hour.
Before starting drug treatment, you should definitely consult a doctor. It is also important to read the instructions for the medicine, which tell you how to dose the drug correctly, taking into account the patient’s weight or age.
How does a sore throat manifest?
The main symptom of a sore throat is pain, both at rest and when swallowing or talking. A sore throat is the primary symptom of pharyngitis. The terms "angina" and "pharyngitis or pharyngotonsillitis" are often used interchangeably. Pharyngitis refers to objective signs of inflammation of the pharynx: swelling, exudation, ulceration or obvious erythema. Redness of the throat may occur as part of a general redness of all mucous membranes of the upper respiratory tract in young patients with fever. The diagnosis of pharyngitis is justified only when the pharynx is objectively redder than the rest of the mucous membranes.
Causes and routes of infection
The very name of the disease already makes it clear that the source of infection is a variety of viruses. These can be herpes viruses, influenza, Coxsackie viruses, ECHO viruses, adenoviruses, enteroviruses and others. Therefore, the disease is conventionally divided into adenoviral, influenza and herpetic.
The disease is highly contagious: you can become infected during a conversation, by sneezing, through dishes, toys, and food. Viruses that enter the body reach the surface of the tonsils and settle there. From the moment of infection, the patient remains a source of infection for another 30 days. Many factors increase the likelihood of developing the disease:
- cold season;
- improper and unbalanced diet;
- lack of personal hygiene;
- hypothermia (for example, caught in the rain, eaten cold ice cream);
- smoking in front of a child;
- bad ecology;
- climate change;
- weak immunity;
- the presence of a chronic source of infection in the body (for example, chronic tonsillitis);
- carious teeth;
- allergic reactions;
- tuberculosis, diabetes and other diseases;
- stressful situations.
Sore throats caused by influenza viruses or adenoviruses usually occur during the cold season, especially during outbreaks of epidemics, when the body's defenses weaken. Herpetic sore throats are more common in the summer. In order to understand in time that we are dealing with viral tonsillitis, it is necessary to be able to distinguish the main symptoms of the disease in a child.
What could be the causes of a sore throat?
Most often, sore throats are caused by viruses. Less commonly, sore throats occur due to bacterial infections. Viral pathogens such as corona virus, rhinovirus, adenovirus, influenza and parainfluenza are the most common and usually present as a cold. Other viral infections that may present with a sore throat are the Epstein-Barr virus and HIV, which lead to the development of a sore throat early in the disease.
Recurrent tonsillitis may occur due to cytomegalovirus or fungal infections in young patients with immunodeficiency.
Among bacterial infections, group A beta-hemolytic streptococcus (GABHS) is the most common cause of bacterial sore throat. It accounts for 15–36% of cases of acute pharyngitis in children in developed industrial countries. Other pathogens may include streptococci types C and G.
Rarer causes of sore throat include infections with Staphylococcus aureus, Mycoplasma, Chlamydia pneumoniae, Moraxella catarrhalis and Yersinia.
Fusobacterium necrophorum infection is an uncommon infection that begins with fever and sore throat and may subsequently develop into Lemierre's syndrome, which is characterized by blood poisoning, thrombosis of the internal jugular vein, and at least one metastatic site of infection.
Another group of causes of sore throat in children are peritonsillar, retropharyngeal and lateral pharyngeal abscesses, which arise due to the spread of infection from local sources, for example, bacterial tonsillitis. Along with fever and sore throat, these cases may present other symptoms such as painful swallowing, drooling, trismus, visible swelling under the lower jaw and deviation of the uvula away from the source of inflammation.
Allergies can also be the cause of a sore throat, especially when it is complicated by nasal bleeding. Irritants such as dust, tobacco and silt stove smoke, and chemical air pollutants can lead to chronic sore throat.
Talking for a long time in a raised voice or shouting for a long time also lead to a sore throat.
A sore throat can also occur due to damage to the larynx by stomach acid due to gastroesophageal reflux disease (GERD).
Prevention of acute respiratory infections and acute respiratory viral infections in children
Prevention of acute respiratory infections should include, first of all, protection in children from sources of infection with acute respiratory diseases
, during periods of epidemic, it is recommended to wear a medical mask in kindergarten and school. In addition, you must:
- provide the child with vaccinations on schedule and during the epidemic;
- avoid hypothermia;
- carry out hardening;
- feed the child correctly - in a balanced manner, according to a schedule, with food rich in vitamins;
- spend less time in public places during outbreaks;
- at the first signs of illness, consult a doctor, even if you need to miss school or kindergarten;
- walk more with your child in the fresh air;
- introduce general strengthening gymnastics into the child’s daily routine.
Sources:
- S.O. Klyuchnikov, O.V. Zaitseva, I.M. Osmanov, A.I. Krapivkin, E.S. Keshishyan, O.V. Blinova, O.V. Bystrova. Acute respiratory diseases in children (Manual for doctors) // Russian Bulletin of Perinatology and Pediatrics, 2008, supplement No. 3.2008.
- L.A. Balykova, Doctor of Medical Sciences, corresponding member. RAS, T.I. Razdolkina, candidate of medical sciences, associate professor. Acute respiratory diseases in children // Remedium Privolzhye, 2022, No. 3(163), pp. 18-22.
- T.A. Samsygina. Modern treatment of acute respiratory diseases in children // Pediatrics, 2013, No. 3, pp. 38-42.
- Seto WH, Conly JM, Pessoa-Silva CL et al. Infection prevention and control measures for acute respiratory infections in healthcare settings: an update // East Mediterr Health J., 2013, i9 (Suppl. i), p. 39-47.
Markova Daria Olegovna Clinic
Author of the article
Markova Daria Olegovna
Specialty: endocrinologist
Experience: 15 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
What signs of the disease are assessed by the doctor?
When collecting an anamnesis and examining a child, the doctor will pay attention to the following symptoms:
- Onset and duration of sore throat
- Severity of fever
- Associated cough, runny nose, conjunctivitis, headache, myalgia (muscle pain)
- Any difficulty breathing, especially snoring at night or stridor
- History of rash, diarrhea, or allergies
- Regurgitation (reflux of gastric contents into the esophagus), pain in the epigastric or retrosternal region.
- Family history of sore throat in the past 2 weeks.
- Similar complaints in the past,
- Vaccination history
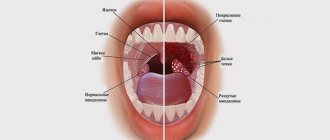
When examining the throat, the doctor may reveal:
- White or gray plaques on the surface of the tonsils or pharynx that rub off easily without bleeding.
- Ulcerations
- Plaques in the form of films, characteristic of infectious mononucleosis, diphtheria and sometimes streptococcal infection. Tularemia can also be a rare cause of such plaques.
- Films of gray or black color, extending beyond the tonsils, with swallowing problems and the absence of severe fever, are characteristic of diphtheria.
- Oral thrush, which is common in newborns and infants, may have a pseudomembrane (curdled plaques), the removal of which can cause mild pinpoint bleeding.
- Convexity of the oropharynx or lateral displacement of the uvula indicates a parapharyngeal or peritonsillar abscess.
- Herpetic sore throat is characterized by painful vesicular (bubble-like) formations on the pharynx and tonsils. Herpes simplex causes painful blisters limited to the front of the mouth, which can sometimes spread to the front of the tonsils.
- Lymphadenopathy (enlarged and painful anterior and posterior cervical lymph nodes is characteristic of bacterial tonsillitis or Epstein-Barr virus infection.
- Streptococcal pharyngitis is characterized by sore throat, temperature ≥38.3°C, tonsil and pharyngeal plaque, and cervical lymphadenopathy.
- Cough, runny nose and diarrhea are more common with viral pharyngitis.
Still have questions?
Get an online consultation from leading pediatricians in St. Petersburg!
A professional and experienced pediatrician will answer your questions.
Medical care for a child without leaving home at a convenient time.
sign up for a consultation
A Skype consultation lasts 45 minutes.
Possible complications
As a rule, the viral form of tonsillitis, if a sore throat is treated correctly and in a timely manner, does not pose a danger and goes away without complications.
ARVI can be complicated by the addition of a bacterial infection of the nasal cavity: a characteristic sign is green discharge from the nose. The prognosis for this development is favorable, just the duration of treatment will increase by several days.
Influenza viruses cause complications more often than other viruses. This can be pneumonia, lung abscess, hepatitis, diseases of the heart muscle, neuritis. Adenoviruses can cause sinusitis and pneumonia.
A common consequence of viral tonsillitis is infection of the oral cavity and pharynx by fungus. Bacterial tonsillitis often develops. Exacerbations of chronic diseases are possible.
Additional research for sore throat
The main problem when diagnosing a sore throat is not to miss the dangerous diagnoses of diphtheria and GABHS sore throat. To do this, a throat swab is taken from the child for bacterial and culture tests, including Albert's stain for diphtheria. A provisional diagnosis of diphtheria is suggested if the smear shows typical drumstick organisms. However, definitive diagnosis requires confirmation of C. diphtherium growth in culture.
To diagnose GABHS sore throat, there are antigen rapid tests. Their action is based on the extraction of group A carbohydrate antigen from throat swab materials with nitrous acid. These rapid tests are very specific (>95%) and provide immediate results, but have variable sensitivity. Confirmation of a positive result is not required, and if negative, a culture is recommended to exclude an infection dangerous to the child. Streptococcal antibody titers are not useful for diagnosing streptococcal pharyngitis and are not generally recommended.
Other studies:
- General blood analysis
- Peripheral blood smears - for the presence of atypical lymphocytes.
- Serology of Epstein-Barr virus (IgM antibodies)
- X-ray of the soft tissues of the neck (lateral view) if a retropharyngeal abscess is suspected.
- CT scan of the neck, including the base of the skull, to look for an abscess.
Treatment for a child with a sore throat
Prescriptions must be made by a doctor based on the established diagnosis and the identified or suspected pathogen. Self-prescription of medications by parents is unacceptable. This can lead to serious consequences for the child's health.
Farnigitis caused by GABHS infection is a disease that goes away on its own. However, treatment with antibiotics in this case provides rapid relief of symptoms, prevents purulent (otitis media, sinusitis, tonsillitis) and non-purulent complications, and also reduces the possibility of transmission of infection. Antibiotics reduce the incidence of rheumatic fever by more than two-thirds.
Clinical features, epidemiological criteria, and the judgment of an experienced clinician, with or without additional testing, usually indicate the need for antibiotics. The currently used pharyngitis decision score was adapted by adding age to the four components of the original Centor score (no cough, no swollen and tender anterior cervical nodes, temperature >38°C, tonsil plaque or swelling. Each component is given 1 point. age from 3 to 14 years is also given 1 point. Children or adolescents with a score of 0 or 1 do not need antibiotic therapy. Patients with a score of 2 or 3 points should undergo microbiological diagnosis of the pathogen and receive antibiotics if the results are positive. Children with A score of 4 or higher is at high risk for streptococcal GABHS pharyngitis and should receive antibiotic therapy.
Due to cost, narrow spectrum of action, safety and effectiveness, penicillin is the drug of choice. A shorter duration of treatment increases the risk of bacteriological relapse of the disease. The unjustified use of macrolides for the treatment of GABHS pharyngitis has become the main reason for the formation of resistant strains of pathogens.