Herpangina is one of the most common viral diseases in children. Almost everyone experiences this disease in childhood, although this diagnosis also occurs in adults. From a scientific point of view, the very name “herpetic sore throat” was incorrectly given to the disease. Previously, the disease was little studied. Scientists, noticing the similarity of rashes during the disease with those of herpes, came to the conclusion that the causative agent of the disease was the herpes virus, and gave the disease a name that has stuck and is found in the medical literature in exactly this form. Although the disease has nothing in common with herpes infection. It has been established that the cause of herpetic sore throat is enteroviruses - Coxsackie viruses of groups A and B and ECHO viruses (echoviruses). In medical reference books you can find different versions of the names of this disease: aphthous tonsillitis, vesicular pharyngitis, herpetic tonsillitis, herpangina, etc.
As already mentioned, children under ten years of age are at risk: infants, preschoolers and children of primary school age. The severity of the disease depends on the age of the child. The disease is most severe in children in the first year of life. Preschoolers are more often infected because at this age they do not pay due attention to hygiene, have contact with animals and are often in children's groups. To become infected, it is enough to eat unwashed fruit. This should also include the immaturity of immunity at an early age. The disease is highly contagious, and often its outbreaks become epidemic. It is noteworthy that this disease does not occur in babies in the first months of life - the antibodies found in mother's milk create some kind of immunity to herpangina.
One can trace the obvious seasonality of herpetic sore throat: the peak occurs in summer and autumn. As a rule, having been ill once, a child becomes immune to re-infection, so this disease is less common among adolescents and adults.
Infection can occur in one of three ways:
- airborne
- contact
- fecal-oral.
With the airborne method, infection occurs by sneezing, coughing, or talking with a carrier of the virus. In case of contact - through discharge from the nasopharynx. With the fecal-oral method - through dirty hands, through unwashed food, toys and pacifiers, which is especially typical for children.
Even a recovering person can still spread the infection around him for about a month, so it is believed that herpes sore throat is highly contagious: a child can easily become infected in kindergarten from a baby who does not even have obvious symptoms of the disease. If one family member gets sick, most likely everyone will suffer from the disease.
How does infection spread throughout the body? First, the virus from the nasopharynx reaches the intestinal lymph nodes through the lymph flow. Already in the intestines, the virus gains strength and enters the blood, and severe inflammation begins in the oropharynx.
Probable Causes
Red spots in the throat are the main sign of the occurrence of pathological processes in the mucous membrane of the airways. The following factors can trigger their development:
- dry air;
- inhalation of volatile chemicals;
- hypothermia;
- vitamin deficiency;
- allergic reactions;
- decreased body reactivity;
- infectious diseases;
- disruptions in the gastrointestinal tract;
- endocrine disorders;
- bad habits.
The cause of the appearance of red spots on the throat and palate can be identified by their location, number and accompanying manifestations.
Most often, the causes of the occurrence lie in the development of bacterial and viral infections. However, in order to make sure that such suspicions are correct, you need to seek help from a doctor.
Pediatric infectious diseases
Many infectious diseases that manifest as a rash on the palate are known as “childhood” diseases. But this does not mean that adults are not susceptible to infection. Having suffered from such diseases once, a person receives lifelong immunity. But if you do not get the same chickenpox in childhood, there is a risk of contracting this infection in adulthood.
Rubella
With rubella, red spots may first appear on the child's palate, and only then on the face and body. Rubella usually resolves easily and without complications in childhood, with the exception of infants up to one year old. These babies endure the disease very hard, so scarlet specks in the mouth, which quickly merge into specks, should alert parents: this may be the first symptom of rubella. This disease is also dangerous for adults who did not have it in childhood, especially for pregnant women.
Measles
As with rubella, with measles a rash in the mouth may appear earlier than on the body - sometimes within a day or two. But the nature of the rash is very different: with measles, the rash looks like dots of white or pale gray color, reminiscent of semolina. Their accumulations on the upper palate, tonsils and back of the throat are surrounded by a pinkish border, this phenomenon is called Belsky-Filatov syndrome.
Chicken pox
With chickenpox, a red rash in the mouth should alert you, as it indicates a complicated course of the disease. Bubbles filled with liquid can shed the gums, tongue, inner surfaces of the baby’s lips and cheeks, and are often found at the top - on the hard and soft palate. Breaking through, they form ulcerations in the oral cavity.
Scarlet fever
With scarlet fever, a small red rash covering the child's body may also appear on the upper palate. The mucous membranes of the pharynx with scarlet fever are bright red, the regional lymph nodes and tonsils are enlarged, the tongue becomes crimson in color and is covered with a white coating - see photo.
Speckled rashes are usually accompanied by a very high fever and vomiting, and in severe forms of the disease - convulsions and clouding of consciousness.
- Causes of rashes in children
Roseola
Since the disease begins with a high fever, and after a couple of days, when the temperature subsides, a rash appears, roseola is often mistaken for ARVI and an associated allergy to medications. Small red spots and blisters in the throat and palate precede the appearance of similar rashes on the body. Their presence is accompanied by redness of the pharynx and pain when swallowing.
The difference between a rash in the mouth and on the body with roseola and any other is that it disappears when pressed.
Angina
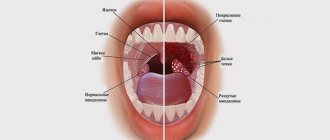
Herpetic sore throat is also a fairly common cause of the formation of red dots in the throat on the roof of the mouth. The disease is characterized by high fever that lasts for several days, pain when swallowing, discomfort in the abdomen, and enlarged lymph nodes.
Streptococcal sore throat is accompanied by general malaise, headache, and high body temperature. The tonsils become loose and covered with plaque. In this case, antibiotic therapy is used, but the treatment regimen must be drawn up by a qualified specialist.
Other reasons
Rashes in the throat, if severe discomfort and pain occur, can signal a change in the morphological properties of soft tissues in the areas of their localization. Erythematous spots, which are localized on the soft palate, in some cases develop due to the occurrence of complex diseases:
- exudative erythema;
- staphylococcal infection;
- syphilis;
- Kawasaki syndrome;
- roseola;
- meningitis;
- typhus
Since the list of possible pathologies is very extensive, if red spots appear in the throat, a visit to the therapist cannot be postponed. The principles of therapy depend on the etiological causes of the development of the disease, the localization of pathological formations and accompanying clinical symptoms. As a rule, in order to eliminate infectious ENT diseases, antiviral and antibacterial drugs are used. Analgesics, antipyretics and antihistamines can also make the patient feel better and eliminate discomfort.
Some bacterial and viral infections cause rashes and spots on the mucous membrane of the throat. They are most often red in color, but can be of different sizes and shapes, and their localization also differs. They can be located in different places.
In some pathologies, red spots in the throat occur only in rare cases and are not important for diagnosis. They do not affect subsequent therapy of the underlying disease. Similar diseases include influenza and ARVI, in which red spots in the throat do not always appear and not in all patients.
However, there are situations when a doctor, looking at a rash in the throat, can make a diagnosis immediately, since in some cases characteristic spots become one of the main symptoms. Such pathologies include, for example, acute stomatitis and herpetic sore throat. It is very unpleasant to notice such a rash in the mouth, especially if red spots are found in the throat of a small child.
Treatment of herpes sore throat in children
There is no specific antiviral treatment. Treatment of the cause of herpetic disease should be carried out according to the following scheme:
- isolation of the patient
- drinking plenty of fluids, bed rest
- actions aimed at relieving and alleviating symptoms.
At the moment, no drug has yet been invented that can kill the causative agent of the disease. You can only alleviate or remove the symptoms. A person recovers completely only when the body develops immunity to the virus. Usually the body takes a week to do this.
First of all, it is advisable to isolate the child from other family members - separate dishes, linen and towels - the disease is contagious. For herpetic sore throat, children are prescribed antihistamines to relieve swelling and irritation. "Claritin", "Suprastin" and others are suitable. To reduce the temperature, use antipyretics: Nurofen, Efferalgan, Paracetamol, etc. To relieve pain in the throat, gargle with decoctions of sage, chamomile, calendula, salt or soda solution. Rinsing should be done every hour. You can use special sprays and aerosols: Hexoral, Ingalipt, Tantum-Verde. Tablets and lozenges relieve pain. It is advisable to use the antiseptic agents Miramistin and Chlorhexidine.
For successful recovery it is necessary to create favorable conditions for the child. It is necessary to provide conditions for sleeping in a well and frequently ventilated room. The diet should consist of soups, purees, and cereals. Food should not be hot so as not to irritate a sore throat. Don't forget about drinking plenty of warm drinks. The patient can be given rosehip decoction, tea with jam or honey.
Note to parents! In case of herpes sore throat, do not inhale, warm up or apply compresses under any circumstances. Such measures will only activate viruses, and the disease will drag on.
Some parents mistakenly lubricate the bubbles in the larynx with iodine or brilliant green. This measure is absolutely ineffective, does not bring any practical benefit, but causes severe pain to the baby.
There is no need to give your child antiherpetic drugs such as Acyclovir and its analogues. As we have already mentioned, the course of the disease has nothing to do with the herpes virus.
What causes the appearance of rashes
- viruses that cause diseases of the upper respiratory tract;
- influenza virus;
- Epstein-Barr virus (causative agent of mononucleosis);
- adenovirus;
- enterovirus HSV - 1 (virus that causes herpetic sore throat).
If infected with any of these viruses, the ciliated epithelium lining the upper respiratory tract is affected.
Of the bacterial microorganisms that can cause the symptom of “red throat,” the most common is streptococcus A (GAS). This is practically the only bacterium that can infect the throat. This is what causes streptococcal sore throat.
- Encyclopedia of rashes - 2
Allergic reaction as a cause of rash without fever
The pathological reaction of the immune system is the result of exposure to external factors. The causes of an allergic reaction may be:
- rinses, toothpastes of bright color, with a pungent odor and taste;
- low-quality filling material or dental structures - braces, veneers;
- certain foods: citrus fruits, honey, nuts;
- low quality plastic toys that a small child puts in his mouth.
The allergic reaction occurs without fever. Rashes are observed not only on the mucous membrane of the oral cavity, but also on the skin. A typical symptom is severe itching of the skin.
Treatment includes antiallergic drugs; local dosage forms are prescribed only in severe cases. These can be hormonal ointments that reduce itching and reduce redness on the skin. The main task is to eliminate contact with the allergen and prevent its re-entry.
Symptoms
Gingivitis has a main symptom by which it is easily identified - inflammation affecting the child’s gums. The process begins with a slight redness that quickly gains strength. This signal often goes unnoticed by parents, and children go to the dentist with an active inflammatory process, bright red swollen gums, burning, and pain. These signs indicate that the disease has entered an acute phase.
Children suffer most from the catarrhal form of this disease, which can be chronic or acute. In the first case, the symptoms are not pronounced, pain occurs only when brushing, there is slight swelling, redness, and cyanosis of the gums.
A sign of an acute form of the disease is intoxication of the child’s body. It manifests itself as headache, nausea, lethargy, and fever.
The most complex type of disease, ulcerative gingivitis, manifests itself as follows:
- the inflammatory process progresses;
- their structure changes;
- there is an unpleasant odor from the mouth;
- lymph nodes in the neck enlarge;
- saliva is produced profusely;
- the skin turns pale.
If these signs are left unattended, an ulcerative-necrotic form of the disease may occur, when necrotic areas with a gray-green coating and a putrid odor appear on the gums, saliva becomes viscous, body temperature rises and the general condition significantly worsens.. All this indicates severe intoxication in organism.
During puberty in a teenager or if he has problems with hormones, hypertrophic gingivitis occurs. It occurs due to improper orthodontic treatment of dental anomalies. The inflammatory process is accompanied by increased growth of gingival tissue, which leads to partial closure of dental crowns. This form of the disease is usually localized. One or two gums are affected, sometimes the affected area expands. The most common location is the lower anterior incisors and canines.
Atrophic gingivitis does not have a pronounced inflammatory process and occurs without pain, although over time it can be complicated by periodontal disease.