Therapeutic methods for treating periodontitis
The key to successful therapeutic treatment is complete patency of the root canal. In this case, the root canal can be reliably sealed, which will eliminate it as a source of irritants that support the inflammatory process. Single-rooted teeth with canals that are easily accessible for treatment are treated therapeutically with medications, followed by filling the canals.
Treatment of acute process
Acute periodontitis is characterized by the following symptoms:
- Constant severe aching pain in the tooth;
- Increased pain in the tooth when biting or touching the tooth;
- Feeling of a grown tooth: the patient feels as if the tooth has moved out of the dental arch;
- The tooth becomes slightly mobile;
- Swelling of the gums develops;
- There is a headache, a feeling of malaise;
- Body temperature may rise to 38°C.
Death and decomposition of the pulp occurs in the root canals; the products of its decay, together with pathogenic microorganisms, penetrate through the apical foramen into the periodontium, causing its inflammation and destruction. Periodontitis can develop near a pulpless tooth due to improper root canal filling. In any case, the goals of treating periodontitis are the following:
- Cleansing root canals from pulp decay products.
- Destruction of pathogenic microflora.
- Elimination of the inflammatory process in the periodontium.
- Stimulation of periodontal regeneration processes.
- Preservation of the tooth.
Treatment of acute periodontitis is carried out in several visits; at the first visit to the dentist, the following actions are performed:
- At the initial consultation: examination, necessary photographs and studies, drawing up and agreeing on a treatment plan;
- Anesthesia;
- Preparation and treatment of carious cavities, creating access to root canals.
- Removal of the affected pulp and its decay products. If depulpation has already been performed previously, the canals are unsealed to provide access to the root apex.
- Instrumental channel processing. Using instruments, the remaining pulp is carefully removed, the root canal is expanded and given a shape suitable for filling.
- Medicinal treatment of canals. The channels are treated with drugs with an antibacterial effect. The root canal is washed several times with an antiseptic solution, then a cotton swab with an anti-inflammatory drug, antiseptic or liquid lysozyme solution is placed in it, and the tooth cavity is isolated with an airtight bandage.
- Installation of a temporary filling.
In acute periodontitis, there is usually no significant accumulation of exudate at the root apex, so the measures taken are quite sufficient to eliminate the inflammatory process. If acute periodontitis is accompanied by purulent inflammation, the canals can be left unsealed for several days to drain the pus and carry out antiseptic rinses.
If the condition of the root canals is satisfactory, there is no purulent exudate and pain, the canals are sealed, a temporary filling is placed, and then after a few days a permanent one is placed.
A second appointment is scheduled after 2-4 days, the patient is recommended to take painkillers, and sometimes antibiotics. At a follow-up appointment:
- Removing the temporary filling of the bandage and cotton wool from the canal
- If there are traces of purulent discharge or contamination of the turunda, the canal is re-treated with solutions of enzymes and antiseptics according to the described method;
- If there are no traces of discharge on the turunda and the clinical course is favorable, the canals are again subjected to medicinal and instrumental treatment, washed with an antiseptic and dried with a stream of air;
- Sometimes, to speed up the recovery processes in the periodontium before filling the root canal, biologically active preparations are removed from the root apex;
- Afterwards, the root canals are filled. The filling material prevents the entry of bacteria and their toxins into the periodontium, sometimes this is enough to eliminate the source of chronic inflammation and restore bone tissue;
- In case of a poorly passable canal, filling is postponed to the next visit. In this case, the turunda with the medicinal substance is left in the canal again, and the tooth cavity is closed with a bandage.
The use of a microscope in the treatment and treatment of canals can greatly improve the quality of these operations, and therefore increase the duration of the prognosis for the resulting treatment result.
Currently, the best material for filling canals in the treatment of periodontitis is gutta-percha. Compared to other materials, gutta-percha has the following advantages:
- Maximum dense filling of the channel.
- Reliable sealing of the apical foramen.
- Ability to penetrate deltoid branches of root canals.
- Resistance to tissue fluid.
- Biological inertness, lack of toxic effects on tissue.
- When the canal is properly filled with gutta-percha, it does not move beyond the apex of the tooth, which means the periodontium is not injured.
The quality of canal filling can be improved if you use an injection device for liquid gutta-percha (3D root canal obturation technology), for example, in Dental World dentistry we use the Dentsply Calamus device.
Inspection and primary treatment of dental canal cavities
Treatment of periodontitis begins with a thorough examination of the patient by a dentist, after which the specialist prescribes an x-ray for the patient. The image will help make the diagnosis as accurately as possible, as well as study in detail the number of dental canals, their length and shape. Next, an anesthetic injection is made into the area of the diseased tooth, without which treatment of periodontitis can be a very painful and uncomfortable process for the patient.
After the drug takes effect, the doctor will perform the following manipulations:
- It will remove from the diseased dental unit all tissues damaged by the carious process, as well as some healthy enamel and dentin. This is necessary to gain access to the mouths of the dental canals;
- If the tooth has not been treated before, the doctor will remove the inflamed pulp from it. If treatment of the unit with the removal of nerves has previously been carried out, the tooth canals are unfilled;
- Expand the tooth canals manually, using specialized instruments for this purpose. After expansion, the tooth canals are thoroughly washed with an antibacterial solution;
- Place a medicine with enhanced antiseptic action into the channels.
After applying the antiseptic to the dental unit, a temporary filling is installed, and the specialist thoroughly advises the patient on oral care, prescribes anti-inflammatory drugs and medications that reduce the risk of allergic reactions. The next time you will need to visit the doctor approximately three days after completing the first stage of periodontitis treatment.
Treatment of chronic periodontitis
Chronic periodontitis can develop in several forms, the diagnosis of some of them is difficult due to the minimal number of complaints from the patient. Often, when a diagnosis of acute periodontitis is made, a more in-depth examination reveals an exacerbation of the chronic process. Chronic periodontal inflammation is confirmed by x-ray examination: the x-ray image shows a focus of rarefaction of bone tissue around the apex of the tooth root.
Clinical manifestations of chronic periodontitis depend on the form of the disease. Symptoms of the disease apply the classification according to Lukomsky:
- Granulating periodontitis causes periodic mild pain. At the time of exacerbation of this form of periodontitis, a gingival fistula often appears, through which purulent contents accumulated around the root apex emerge;
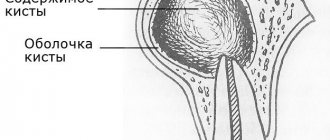
- Granulomatous periodontitis is characterized by an almost asymptomatic course; patients complain of discomfort when biting on a tooth. An x-ray reveals a granuloma around the apex of the tooth root, which, if left untreated, turns into a cyst;
- The fibrous form of chronic periodontitis is difficult to diagnose, since patients do not present any complaints. X-ray reveals deformation of the periodontal fissure.
Treatment of chronic periodontitis is similar to the treatment of acute periodontitis. After diagnosis and approval of the treatment plan, mechanical and antiseptic treatment of the canals is carried out. The carious cavity is first prepared and the pulp is removed. Irregularities are removed from the inner walls of the canal, the canal is straightened, and it is given a conical shape. After finishing the mech. treatment, the canals are washed repeatedly with antiseptics (mainly chlorine-containing), and then turundas with antiseptics are left in the canals under a sealed bandage. The patient is scheduled for the next visit.
The differences between the treatment of chronic periodontitis and acute periodontitis are as follows:
- Manipulations associated with medicinal treatment of the canals are carried out more often: until the signs of inflammation disappear. This is especially true for the treatment of granulomatous periodontitis: treatment is carried out until the granuloma is completely reabsorbed.
- When filling the root canal with a medicinal substance, it is injected into the apical space, which helps reduce the inflammatory process, resorption and replacement of granulations. Currently, research shows that it is not necessary to remove medicinal materials beyond the apex.
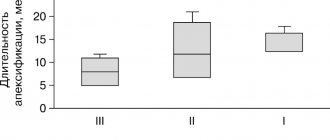
- After eliminating symptoms during exacerbation of chronic periodontitis, the root canals are filled with a filling material based on calcium hydroxide - this is a temporary material, the use of which achieves several goals: calcium hydroxide has antibacterial and anti-inflammatory effects, stops further tissue resorption, and stimulates regeneration processes. Temporary filling with calcium hydroxide is performed for 3-8 weeks, then the material is renewed; Treatment with it can last up to a year.
- If the patient does not complain, and percussion of the tooth and palpation of the gums are painless, the canals are re-treated with antiseptics and sealed. After this, a permanent filling is placed on the tooth.
- In the treatment of chronic periodontitis, physiotherapeutic methods are actively used: UHF, microwave therapy, magnetic therapy, darsonvalization, electrophoresis.
Prevention
To prevent the development of granulomatous periodontitis, it is necessary to promptly identify and treat dental diseases. To do this, you need to visit a doctor at least twice a year, and not just when the problem becomes obvious. We must not forget about regular oral hygiene, as well as periodic professional teeth cleaning, since dental plaque is a breeding ground for pathogenic bacteria that cause various diseases, including granulomatous periodontitis.
Treatment of periodontitis in one visit
Over the past decades, methods for treating chronic periodontitis have been improved, which has reduced the number of visits to one.
The indication for treatment of periodontitis in one visit is the presence of a fistulous tract in a single-rooted tooth. An outflow of purulent discharge occurs through the fistula, so filling the canal and removing the filling material beyond the apical opening of the tooth root is not accompanied by an exacerbation of the inflammatory process.
If conservative treatment of chronic periodontitis is ineffective, surgical methods are resorted to, in particular cystectomy and root apex resection.
Causes of the disease
The main reason for the development of the disease is a chronic inflammatory process due to an advanced form of pulpitis or carious lesions. Other reasons may be injuries to the dentition due to mechanical impact, for example, when biting hard foods or during a fall or impact.
Also, the body’s reaction to incorrectly formulated drug treatment and incorrectly selected dental braces can also be expressed by inflammation in the gum area. An exacerbation of the process occurs in the presence of endocrine diseases, as well as a lack of vitamins and minerals in the body, reduced immunity.
Surgical methods
The arsenal of a dental surgeon in the treatment of periodontitis includes the following manipulations:
- Opening the gums - used to facilitate the drainage of pus that has accumulated at the apex of the root and caused the formation of an abscess on the gum.
- Hemisection is an operation to remove the root of a multi-rooted tooth, at the apex of which a focus of inflammation is found, while at the same time the crown part of the tooth adjacent to the root is removed. The canals of the remaining roots must be thoroughly treated before surgery. The hole remaining after hemisection is filled with osteoplastic material, and the mucous membrane is sutured. The tooth is later covered with a crown.
- Root amputation is an operation to remove the root of a multi-rooted tooth, but preserving the crown part.
- Root apex resection – the root apex is removed through a hole formed on the outer surface of the jaw in the area of the projection of the root apex of the diseased tooth. The operation is often performed in combination with cystectomy - removal of a granuloma or cyst. The cavity formed after their removal is filled with osteoplastic material. Also, resection is indicated if it is not possible to unseal the canal (provided that it is thoroughly sealed throughout its entire length, except for the apical part).
- Tooth replantation is a complex operation that involves removing a tooth and then returning it to the socket after curettage of the alveoli, filling of the canals and resection of the apex (sometimes resection is not performed). The method is used on multi-rooted teeth, the healing of the replanted tooth can last up to 10 weeks, during which time the tooth must be kept at rest using splints or trays. Even with successful engraftment, a replanted tooth must be removed on average after five years due to root resorption and loss of stability.
- Tooth extraction – if it is impossible to use other methods of treating periodontitis, they resort to tooth extraction. Subsequently, it is recommended to carry out implantation - implantation of an artificial root (implant) with further installation of a crown. Thanks to implantation, full chewing function is preserved, and the appearance of the artificial tooth does not differ from the natural one.
Modern methods of treating periodontitis allow, in most cases, to save the tooth, but if the patient seeks dental care late, it may be lost. To avoid unpleasant consequences, you need to monitor your dental health, conduct timely preventive examinations of the oral cavity and treat identified diseases.
Diagnostics
In order to correctly diagnose and differentiate this type of periodontitis from fibrous or granulomatous, the dentist conducts a visual examination of the oral cavity, which allows us to identify:
- severely damaged natural tooth crown/large filling/artificial crown;
- change in color of the affected tooth;
- communication between carious and dental cavities;
- insignificant pain reaction to percussion;
- looseness of the gums, on which, after pressing with a dental instrument, a depression is formed.
During a visual examination, the specialist sees swelling of the gums, severe tooth decay, and a change in the color of the enamel. Granulating periodontitis is often observed on teeth with large fillings that have not been changed in a timely manner. Probing of pathological carious tissues does not lead to pain. When the probe is pressed on the affected mucous membrane, the gums become pale and indented. The recess is preserved for a long time. Electroodontodiagnosis is used to accurately identify granulating periodontitis. An increase in the sensitivity threshold of the pulp to 100-150 μA is detected. An x-ray is taken which shows the destruction of the jawbone.
In addition to a visual examination, dental x-rays are performed, which reveals destruction of the jaw bone, and electroodontodiagnostics, which determines an increase in the threshold of pulp excitability.
Possible complications
- Death of the rudiment if the pathology spreads before mineralization begins.
- With prolonged inflammation, the root of a temporary tooth is exposed.
- Change in the position of the follicle in the jaw.
- Local enamel hypoplasia due to infection of the follicle at the beginning of mineralization.
- Destruction of the bone tissue septum between the primary periodontium and the germ of permanent teeth.
- Follicular cyst.
- Delayed eruption of permanent teeth.
- Formation of dental anomalies due to premature removal of milk.