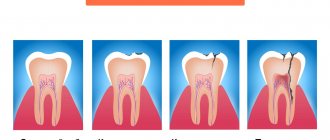
- Caries
- Pulpitis
- Stomatitis
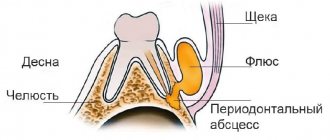
- Flux
- Gingivitis
- Tooth cyst
- Wedge-shaped defect
- Periodontal disease
- Periodontitis
- Periodontitis
- Causes of bad breath
- Signs of pulpitis
- Treatment of dental cyst
- Chronic periodontitis
Periodontitis – inflammation of the periapical (surrounding the root) tissues of the tooth – is a fairly “popular” dental disease.
In terms of frequency of occurrence, it is surpassed only by caries and pulpitis. The dynamics of the symptoms of this dental disease look like this:
- The appearance of aching pain associated with a specific tooth;
- The appearance of bad breath;
- Acute attacks of pain, becoming more pronounced when touching a tooth;
- Swelling of the gums around the affected periodontal area;
- Complication of chewing function - it is difficult for the patient to take not only hard food, but even drink;
- Formation of a fistula through which pus escapes into the oral cavity.
Many patients ignore the initial symptoms of the disease and self-medicate. But independent treatment of periodontitis is extremely incorrect: pain relief with medications, heating and rinsing with herbs will only lead to the fact that the symptomatic picture will be blurred.
An advanced disease is extremely dangerous: the pus that accumulates in the sac at the apex of the root may not find a way out, and the infection will begin to spread to other organs through the muscle tissue.
What is periodontitis?
We can easily notice changes in the appearance of teeth and the appearance of carious lesions on the enamel at home, limiting ourselves to one visual examination of the oral cavity. But things are completely different when you need to know the condition of the pulp. The pulp is the heart of the tooth, which is hidden from prying eyes. To see it, you need to undergo an x-ray examination by a dentist. The same applies to the root and basal tissue of the tooth; their diagnosis is carried out only using an x-ray. Inflammation of the periodontal tissues can be fraught with dangerous consequences; if the infection penetrates deep into the tooth and goes beyond the root canals, a person may lose the tooth.
Permanent canal filling
Permanent canal filling in the treatment of periodontitis is performed during the third visit to the dental office. Before proceeding with any manipulations, the specialist sends the patient for a control x-ray. The image will help determine the effectiveness of periodontitis treatment. If the percentage of bone tissue destruction has decreased significantly, permanent filling of the canals is performed.
The procedure begins with the removal of the temporary filling from the crown of the tooth, and then the canals are freed from the previously placed composite. The doctor will carry out an antiseptic rinse and then fill them to the apical part of the root with a composite. Upon completion of the work, the patient is given another x-ray to monitor the quality of the filling performed. Gutta-percha must be tightly packed into the canals to the very apex of the root, otherwise there is a high risk of relapse of periodontitis.
A couple of days later, the patient comes to the doctor for the fourth time and during this visit the crown part of the tooth is restored with a permanent filling to restore its aesthetics and functionality.
Reasons for the development of periodontitis.
When caries begins, pathogenic bacteria begin to actively multiply and if the disease is not cured in a timely manner, the inflammatory process spreads to the enamel and affects the dentin. When the infection reaches the pulp, a complication of caries develops. It is untreated pulpitis that causes periodontitis. Once in the periodontium, the infection begins to irritate it, causing its response. This is how our body reacts to problems: the patient may experience increasing pain, which is localized and sometimes becomes completely unbearable.
It should also be noted that the formation of periodontitis is also possible under other conditions:
Poorly sealed canals.
When filling, it is important to fill the root canals tightly and correctly with the material, and for this it is necessary to determine their size using radiography. If the dentist skipped this stage and did not fill the canal, inflammation may begin in the remaining space.
Mechanical injury to the jaw or teeth.
Very often, periodontitis occurs in children, because... Little fidgets constantly fall, and sometimes they can hurt their faces, you should pay attention if your child, after such an active walk, begins to complain of severe tooth pain.
Development of infection under the crown.
In this case, periodontitis occurs due to the incompetence of the doctor, or he incorrectly carried out the preparation stage and poorly processed the tooth and filled it, or an error was made when placing the crown, and the dentist did not remove the dead pulp.
Use of arsenic.
Previously, arsenic was used to kill the pulp, if the dose is incorrectly determined and with its long-term effect on the body, there is a high risk of an inflammatory process in the periodontal area. Currently, dentists use high-quality anesthetics that allow them to treat and remove the pulp without exposure to arsenic paste.
Use of antiseptic drugs.
One of the main reasons for the development of drug-induced periodontitis is the excess concentration of drugs during filling and treatment of root canals.
Materials for making crowns
Modern dental crowns are made from:
- Metal.
Metal dentures are considered obsolete due to their lack of aesthetics, but are still used because they are the cheapest option; - Metal ceramics.
A relatively inexpensive and durable option, but due to the metal base it is difficult to achieve a “healthy” whiteness of an artificial tooth; - Ceramics.
Ceramic crowns are more aesthetically pleasing than metal-ceramics, but are inferior in strength, so they are usually installed only on the front teeth; - Porcelain.
A type of ceramic crown. Porcelain dentures are indistinguishable from living teeth, since the optical properties of the material are almost identical to tooth enamel. They are also installed on the front teeth; - Zirconia.
They are made on the basis of zirconium dioxide and covered with ceramics on top. Durable, aesthetic, but quite expensive crowns.
Zirconium dentures can be installed on any tooth.
The material, contrary to popular belief, does not cause toothache, but may be the answer to the question of why the gums hurt after installing a crown. Inflammation of the mucous membrane and gums can cause an allergic reaction to the metal in a metal-containing crown. Patients with ceramic and zirconium prostheses do not encounter such problems.
Symptoms and signs of periodontitis.
As mentioned earlier, periodontitis may not manifest itself for a long time; the patient runs the risk of finding out about the disease too late, when it has entered the acute stage. In this case, the signs of inflammation of periodontal tissues will be felt much more clearly. Periodontitis is characterized by the following symptoms:
Deterioration of general condition.
There is an increase in temperature, worsening sleep, weakness, etc.
- Pain when chewing food and when closing the jaws.
- Change in gum color (become darker).
Based on this symptom, periodontitis can be identified in its initial stages of development. Also, the periodontal tissues may swell, and the swelling may spread to the cheek and neck.
Painful sensations.
In the acute course of the disease, the patient begins to be bothered by a sharp, aching pain that radiates to neighboring teeth.
- Slight tooth mobility.
- The appearance of bad breath.
- Increased sensitivity due to mechanical impact on the tooth.
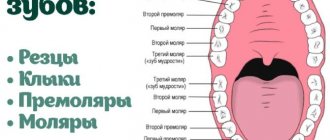
Types of periodontitis.
There are several classifications of periodontitis; it is usually distinguished by the place of formation: apical (infection affects the base or apex of the root) and marginal (occurs in the area of the gum edge due to injury).
According to the nature of the course of the disease, the following stages are distinguished:
Acute periodontitis.
It is further divided into several forms: serous acute periodontitis is the initial stage of the development of inflammation; it occurs after the infection penetrates through the apex of the tooth root into the periodontal area. Then it develops into purulent acute periodontitis. This form of the disease is very dangerous because The pus penetrates the bone structures and can spread throughout the body. It is characterized by: severe increasing pain, painful sensations when pressing on the tooth and when biting, headache, swelling of the mucous membrane, etc.
Chronic.
It has three stages of development: fibrous, granulating and granulomatous. Chronic periodontitis is characterized by a calm and even imperceptible course of the inflammatory process; only sometimes the patient may experience slight pain when tapping a painful tooth. But at the same time, this stage is considered the most dangerous, because may lead to tooth loss. With the development of the granulating form, the unit and the tissues around it are destroyed. A fistula forms on the gum, from which pus flows. Granulomatous periodontitis is characterized by the formation of a granuloma, a sac filled with purulent fluid, which subsequently develops into a cyst if not removed. Tooth mobility increases, gums bleed, and abscesses develop.
Treatment of periodontitis.
During the examination, the dentist will determine the degree of development of periodontitis, and the treatment plan will depend on this. Making a diagnosis is not difficult; upon visual examination of the oral cavity, one will notice severe destruction of the tooth structure, a change in the color of the gums, and there is no reaction to cold and hot water. Eliminating the consequences of inflammation of periodontal tissue can take quite a long time; you will have to visit the doctor several times. Several years ago, such a diagnosis forced doctors to remove the damaged tooth, but now the patient has the opportunity to maintain the integrity of the dentition and get rid of the inflammatory process.
Treatment of periodontitis is possible in several ways; if therapeutic methods are not effective, the dentist uses surgical intervention. Let's take a closer look at the stages of treatment:
Treatment of a damaged tooth.
First, it is necessary to open access to the root canals, remove softened dentin and remnants of infected tissue. This procedure is performed using a special bur, after which the cleaned cavity is treated with antibacterial drugs. Then the tooth canals are widened, washed with antiseptic solutions and the medicine is placed in them. Until the inflammation is stopped, the doctor has no right to proceed to the next stage.
Filling.
At the end of the treatment, the root canals are tightly filled. In most cases, these actions are enough to get rid of inflammation, the microflora of the tooth is normalized, and its tissues are regenerated.
This treatment option is a conservative method; surgical intervention is performed according to a different plan:
The operation is performed under anesthesia. In the area where the granuloma is located, an incision is made into the mucous membrane and periosteum, resection of the root apex is performed and the purulent neoplasm is cleaned out. The wound is washed with antibacterial drugs, disinfected, and sutures are applied.
If the patient's periodontitis is in the last stages of development and treatment does not have a positive effect, then a decision is made to remove the tooth.
Temporary filling
During a second visit to a dentist-therapist during the course of treatment of chronic periodontitis, the area of manipulation is examined. The specialist will also clarify whether the patient has any complaints of pain, swelling in the gum area or other discomfort. If such negative phenomena are not observed, temporary filling of the dental canals is performed.
For this purpose, the temporary filling is initially removed, as well as the antiseptic placed in the tooth canals. The canal openings are thoroughly washed with an antiseptic and then filled with a special type of composite material used for temporary filling. This composite contains calcium hydroxide, a substance that destroys pathogenic microflora and also catalyzes the process of bone tissue regeneration in the area of the upper zone of the tooth root. Temporary filling of canal cavities is done for a fairly long period - from two to three months. The dentist then places a temporary filling in the crown of the tooth.