Almost every person on earth has experienced toothache at least once. It can be very difficult to tolerate, and sometimes simply unbearable. To avoid complications, one of which may be periodontitis, you should immediately consult a doctor.
Periodontitis is an inflammatory process of the apex of the tooth root, as well as in the tissues adjacent to it. This is a rather dangerous disease that can lead to even more serious problems, so you should not delay treatment. Periodontitis can occur as a result of advanced pulpitis or poor-quality canal filling.
Also, the causes of this disease can be an infection, injury, or the consequences of medication. According to statistics, this disease accounts for 45-50% of all dental diseases. People with weakened immune systems are most susceptible to rapid development of the disease.
Indications for treatment of periodontitis
There are two main ways to treat periodontitis: conservative and surgical. Each of them has its own indications and contraindications.
According to modern dental standards, a doctor should give preference to conservative methods. They are indicated for both acute and chronic periodontitis, including the appearance of cysts and granulomas, loose teeth, and increasing inflammation.
However, orthograde treatment cannot be used in all cases. Indications for surgical intervention are:
- obstruction of the tooth root canals;
- the presence of a stump tab or pin that cannot be removed without damaging the roots;
- multiple perihilar cysts or cysts growing into the maxillary sinus;
- wide affected area (over 10 millimeters);
- perforation of the tooth cavity or root wall;
- ineffectiveness of conservative treatment methods.
Important!
When we talk about periodontitis, we often mean apical (also known as periapical or apical) periodontitis - that is, inflammation at the apex of the tooth root. The cause of this disease is endodontic problems. Another type of periodontitis, marginal, affects the gums in the cervical area of the tooth, but it already belongs to the field of periodontology. This material is devoted to the treatment of apical periodontitis only.
The use of antibiotics in modern dental practice is necessary today, because... Despite the development of dentistry, the number of patients with foci of acute and chronic inflammatory processes in the maxillofacial area and oral cavity is not decreasing, so the prescription of antibiotics in dental practice today is completely inevitable. Every day, a dentist is faced with situations when it is necessary to decide on antibacterial therapy: this is an exacerbation of chronic periodontitis, abscess formation of inflammatory periodontal diseases and endodontic-periodontal lesions. In addition, the need to use antibacterial drugs in dentistry is also dictated by the fact that any dental procedure is accompanied by the risk of bacteremia, which is of little importance for somatically healthy patients, but dangerous for people weakened by intercurrent diseases and the presence of conditions for local colonization of pathogenic microorganisms. Thus, when the endodontic instrument extends beyond the apex by 2 mm during canal treatment, bacteremia is detected in 54% of patients. If the canal is treated with a distance of 1 mm from the apex, bacteremia is detected in 31% of patients, and in the vast majority of cases anaerobic microflora is detected. Bacteria that enter the blood of healthy people are destroyed within 10 minutes due to immune defense factors, and bacteremia is transient [6], while for patients with somatic diseases, people taking drugs, alcohol, steroids, whose immune response is reduced or absent , bacteremia can pose a real danger.
Thus, in dental practice, antibiotics are used in the following clinical situations:
- In the treatment of acute and exacerbation of chronic purulent-inflammatory processes in the maxillofacial area: odontogenic inflammatory processes, incl. periostitis, osteomyelitis, pericoronaritis, sinusitis, abscesses and phlegmon, severe infectious diseases of the oral cavity; for inflammatory periodontal diseases.
- For the prevention of postoperative infectious complications.
Thus, the prescription of antibiotics in dental practice can be aimed at preventing infectious complications (antibiotic prophylaxis) and eliminating the existing inflammatory process (antibiotic therapy). The need for antibiotic prophylaxis is associated with the existing statistics of infectious complications of dental operations: thus, according to research results, the incidence of such complications is 3.3% for “clean” wounds, 10.8% for conditionally “clean” wounds, 16.3% for contaminated wounds , 28.6% – for “dirty” wounds [14]. Antibiotic prophylaxis refers to the use of antibiotics to prevent microbial colonization and reduce the risk of postoperative complications. The administration of the antimicrobial drug must be carried out no earlier than an hour and no later than 30 minutes before surgery, i.e. to bacterial contamination of tissues. The goal of antibiotic prophylaxis is to create an effective concentration of the drug in tissues throughout the entire operation and during the first 3-4 hours after surgery. The effective concentration of the antibiotic in the surgical wound must be maintained throughout the entire operation and, most importantly, maintained at the time of suturing, when microbial contamination reaches its maximum. As part of antibiotic prophylaxis, continued administration of an antibiotic after surgery for longer than 24 hours is undesirable, as it negatively affects the dynamics of the inflammatory response, leads to the growth of resistant strains, adverse drug reactions, additional costs and often does not lead to increased effectiveness in the prevention of infectious complications . On the other hand, administering antibiotics after surgery is ineffective. Antibiotic prophylaxis started after the “critical period” is considered late, and according to some data [11], has no effect at all.
Principles of antibiotic prophylaxis:
The benefit of prophylactic use of an antibiotic outweighs the risk of side effects, superinfection and the development of resistant strains.
The choice of drug for antibiotic prophylaxis must be made taking into account the most likely pathogen.
The antimicrobial drug must reach the site of action before microorganisms enter there.
The antibiotic concentration must be maintained throughout the entire period of possible contamination of the operating area.
Indications for antibiotic therapy [2, 4, 5]:
- Increase in temperature, disturbance in general condition.
- A history of diseases such as rheumatism, endocarditis, uveitis, iridocyclitis.
- The patient has transplanted organs and foreign bodies (stents, prosthetic valves and joints).
These indications must be taken into account when choosing chemotherapeutic drugs during endodontic treatment and treatment of inflammatory periodontal diseases.
In modern dental practice, the following groups of antibiotics are most common [1, 7, 8]:
- penicillins (amoxicillin, co-amoxiclav) – first-line drugs;
- lincomycin - an antibiotic used for abscess formation;
- fluoroquinolones: ciprofloxacin, ofloxacin. These drugs are effective in the most severe cases during periodontal treatment when Aggregatibacter actinomycetemcomitans-associated periodontitis is detected, especially in patients with concomitant diabetes mellitus [3].
In recent years, along with a significant increase in the number of patients with purulent-inflammatory processes, there has been an increasingly widespread distribution of microorganisms with natural and acquired resistance to antibiotics, and the situation is often complicated by the fact that several pathogenic microorganisms are involved in the development of the inflammatory process. The difficulty of choosing a drug for antibiotic therapy in the treatment of purulent-inflammatory processes is due to the presence at the site of infection of various groups of aerobic and anaerobic pathogens that differ significantly in sensitivity to antibiotics. Therefore, the goal of rational antibiotic therapy is to select an effective antibacterial drug and its dose, which allows creating the necessary concentration of the active substance in the tissues to suppress the growth of pathogenic bacteria. For effective treatment of patients with purulent-inflammatory processes, there is a need for the combined use of antibiotics or drugs that include antibacterial substances that act on different groups of pathogens. These requirements are met by the combination drug Ciprolet A (A means effectiveness against anaerobes), the effect of which is due to the components included in its composition: ciprofloxacin 500 mg and tinidazole 600 mg.
Ciprofloxacin is a broad-spectrum antimicrobial agent, a fluoroquinolone derivative that affects gram-positive and gram-negative bacilli and cocci, Staphylococcus aureus, viridans streptococcus, Haemophilus influenzae, Escherichia coli, Pseudomonas aeruginosa.
Tinidazole is an antiprotozoal and antimicrobial agent, an imidazole derivative. Tinidazole is similar in structure and action to metronidazole. The activity of tinidazole is 1.5 times greater than that of metronidazole against anaerobes, which is successfully used when pathogen resistance to metronidazole is established.
The action spectra of ciprofloxacin and tinidazole ensure the high effectiveness of Ciprolet A against a wide range of pathogens, gram-positive, gram-negative aerobes and anaerobes. Resistance to it develops extremely slowly: bacterial cells do not have enzymes that inactivate it, and there are practically no persistent microorganisms left.
The undoubted advantage of the antibacterial drug Tsiprolet A is the frequency of administration (2 times a day), while for co-amoxiclav the frequency of administration is 2–3 times, and for lincomycin and metronidazole – 3 times a day. A very unpleasant side effect of antibiotic therapy is antibiotic-associated diarrhea [12, 13]. For Tsiprolet A, the probability of this side effect occurring is less than 1%, while for lincomycin it is 20–30, and for co-amoxiclav it is 10–25%. This is due to the activity of Tsiprolet A against Clostridium difficile [10]. The most important indicator that determines the effectiveness of an antibiotic in inflammatory diseases of the maxillofacial area is its ability to penetrate bone tissue. For Tsiprolet A, this figure is 0.27–1.20, which is twice as high as the same figure for co-amoxiclav and three times higher than for lincomycin [9].
Indications for use of the drug Tsiprolet A: infections of the ENT organs (otitis media, sinusitis, tonsillitis, pharyngitis); infectious and inflammatory processes of the oral cavity; infections of the skin and soft tissues (infected ulcers, wounds, burns, abscesses, cellulitis, ulcerative skin lesions); infections of bones and joints (osteomyelitis, septic arthritis); postoperative infections. Indications for use are related to the fact that its therapeutic concentrations are created, incl. in saliva, tonsils, lung tissue, bronchial secretions, bone tissue, muscles, synovial fluid, articular cartilage and skin, i.e. in all organs and tissues located in the oral cavity, maxillofacial and adjacent areas.
Such a wide range of application and high effectiveness of Tsiprolet A in the treatment of purulent processes in the maxillofacial area are due to the unique spectrum of antimicrobial activity of the drug: Tsiprolet A is active against the Enterobacteriaceae spp. family, which plays a key role in the development of severe purulent lesions in dentistry. Lincomycin, clarithromycin and metronidazole have no effect on these microorganisms. Tsiprolet A is effective against microorganisms that are also not affected by clarithromycin. This is Peptostreptococcus spp. and Fusobacterium spp. – anaerobic bacteria that contribute to the progression and spread of odontogenic infection [8, 9].
When prescribing Tsiprolet A, it is necessary to inform the patient that tinidazole, which is part of the drug, is not compatible with alcohol, because causes disulfiram-like reactions in the form of skin hyperemia, tachycardia, nausea, vomiting, etc., therefore, it is not recommended to take alcoholic beverages during the treatment period.
The wide spectrum of antimicrobial activity of the combined drug Tsiprolet A, the rapid creation of therapeutic concentrations in the organs and tissues of the oral cavity and maxillofacial area allow us to recommend it for wide use in dental practice.
Treatment methods for dental periodontitis
| Conservative treatment | Surgery |
Therapeutic:
Physiotherapeutic:
Conservative treatment of periodontitis is accompanied by the use of antibiotics. | Surgical treatment:
|
Important!
The probability of successful conservative treatment of periodontitis is 70 - 90%
Stages of periodontitis treatment
The number of visits to the clinic for the treatment of periodontitis depends on the stage of the disease (acute periodontitis, chronic, chronic in the acute stage) and the chosen technique. Often, therapy is carried out in several stages and requires at least 2 - 3 visits to the attending physician, since it is not recommended to install a permanent filling until the inflammation is completely removed.
- Preparation for treatment: diagnosis using an x-ray, anesthesia injection.
- Drilling a tooth to access canals, removing a nerve, or removing an old filling.
- If necessary, expand channels.
- Antiseptic treatment of canals, application of medications, physiotherapeutic procedures.
- Installation of a temporary filling.
- Removal of the temporary filling, antiseptic treatment of the canals (this stage is repeated until the source of inflammation is completely eliminated; sometimes this may take several months).
- Installation of a permanent filling, control x-ray.
In parallel, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as home rinses with disinfectant solutions.
First visit
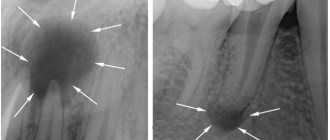
- When a patient comes to the dentist with complaints and the doctor suspects periodontitis, an X-ray examination of the jaw is initially performed to identify the source of pain.
- Then, under anesthesia, the doctor uses a drill to remove carious tissue and open access to the mouths of the tooth tubules. At the same time, the affected pulp is removed and, if necessary, the filling material previously placed there is drilled out of the canals.
- The length of the root canals is certainly measured - using a special device or directly on an x-ray.
- The channels are mechanically expanded and filled with turundums soaked in antiseptic. Without preliminary treatment, it will be difficult for the doctor to properly fill the canal to the very top. Doctors prefer to use Crezofen or its cheaper analogues as a disinfectant. The product does not contain arsenic, does not irritate locally, and is approved for the treatment of pregnant women.
- After all the manipulations, a temporary filling is installed, and the patient goes home. If the dentist deems it necessary, the patient is prescribed anti-inflammatory drugs and medications to prevent the development of allergic reactions. If the form of periodontitis is chronic, antibiotics will not be required.
Features of the treatment of periodontitis with fistula
Odontogenic fistula is one of the complications of periodontitis, mainly granulating. It consists of holes in the mucous membrane, which are formed due to the proliferation of granulations and destruction of the tissues surrounding the tooth. In severe cases, a fistula can appear not only in the gum, but also in the cheek, and even on the skin of the face. Purulent contents are released through the hole, which appears due to the inflammatory process in the periodontium.
On the one hand, the formation of a fistula facilitates the course of the disease, since inflammatory products are eliminated through it (which means that the patient most likely will not suffer from severe pain). On the other hand, non-intervention over time can lead to tooth loss.
You can get rid of a fistula only by eliminating its cause - damage to periodontal tissue. Treatment follows a standard scheme: mechanical treatment of the canals, disinfection and thorough filling. Due to the outflow of pus through the fistulous tract, treatment is most often successful and takes less time. After creating suitable conditions, the fistula goes away on its own, but in severe cases, surgical removal of overgrown granulations may be necessary.
Signs
Clinical manifestations of periodontal inflammation depend on the form of the disease.
In the acute course, the symptoms are pronounced, often accompanied by the formation of a painful abscess on the gum, gumboil (deeply located abscess with intense swelling of the soft tissues of the gums and face), increased body temperature, etc. Acute inflammation can occur in two forms:
- Serous periodontitis occurs without the formation of a purulent cavity. Accompanied by constant aching pain that does not intensify when touching a tooth or biting food.
- Purulent periodontitis is accompanied by the formation of an abscess. Accompanied by sharp, bursting or throbbing pain, the intensity of which may vary. Flux is noticeable on the gum near the diseased tooth, and the soft tissues of the face on the affected side swell. The mobility of the tooth is increased, the pain intensifies when biting and touching the tooth.
In the chronic form, periodontitis is not as severe as acute periodontitis. There are three forms of the disease:
- Fibrous , the symptoms of which are sluggish inflammation without the formation of an abscess and fistulas. Pain with this form rarely occurs. An external sign is a change in the color of the enamel to gray, a change in its transparency. Signs of inflammation are visible only on x-rays.
- Granulomatous , the symptoms of which are periodic formation of an abscess. As it “ripens,” a duct opens on the gum, from which purulent contents pour out. Such ducts can form permanent non-healing fistulas. On x-rays, this form of periodontitis looks like a lesion with a diameter of up to 5 mm at the root apex.
- Granulating , the symptoms of which are chronic toothache, aggravated by biting hard, hot or cold food with a sore tooth. The gums near the tooth are constantly swollen and hyperemic. The opening of the fistula can open both on the oral mucosa and on the skin of the face.
Symptoms of any form of periodontitis tend to subside when the purulent cavity is cleared of its contents.
It is important to know! The main difference between periodontitis and pulpitis is the nature of the pain. With pulpitis, it is acute, painful, reminiscent of electric discharges, intensifying when the diseased tooth comes into contact with solid food particles, hot or cold air.
Treatment of chronic forms of periodontitis
There are three types of chronic periodontitis: fibrous, granulating and granulomatous.
- In fibrous periodontitis, the tissues surrounding the apex of the tooth are replaced by fibrous tissue. The patient usually does not feel pain, and the disease can only be determined by an x-ray.
- Granulating periodontitis is characterized by the growth of granulation tissue: the process of bone resorption (resorption) starts, fistulous tracts are formed, through which inflammatory products are separated. As the granulations expand, the patient begins to experience periodic aching pain.
- Granulomatous periodontitis is accompanied by the appearance of a granuloma - a neoplasm at the root apex. It is a chamber of connective tissue filled with granulations. If the disease is not treated, the growth of granuloma can even lead to a jaw fracture.
Treatment of chronic periodontitis is often carried out using conservative treatment methods. According to modern standards, doctors, as a rule, do not carry out separate treatment for granulomas, cysts and fistula tracts: if the canals are disinfected and properly sealed, the neoplasms will disappear on their own. In advanced cases, surgical intervention is permissible.
How is acute periodontitis treated?
As was said at the beginning of the article, the acute form of periodontitis is characterized by severe pain that occurs for the first time, that is, not associated with a chronic process. In this form, the disease usually occurs due to the lack of timely treatment of pulpitis or the implementation of therapeutic measures at a low professional level.
First visit
The main task at the first visit to the dentist is to ensure the outflow of pus from the purulent sac and eliminate the phenomenon of intoxication in the patient’s body. The necessary activities are carried out in the following sequence:
- An x-ray is taken to identify an acute inflammatory process or exacerbation of a chronic disease. This is of great importance, since to treat these two forms of periodontitis, you need to use different tactics.
- Anesthesia is administered.
- Tissues affected by caries are drilled out.
- The necrotic pulp is removed. This is done if the cause of periodontitis is previously untreated tooth pulpitis. If the disease arose due to poor quality of root canal filling, then the tooth filling is drilled out and the root canals are unfilled.
- The length of the root canals is measured.
- Root canals are expanded with the help of special medical instruments so that the dentist has the opportunity to fill them efficiently. In parallel, they are treated with antiseptic solutions, for which jet washing is carried out. At the end of this stage of treatment, the apical opening of the root canal is enlarged so that the pus can freely drain from the periodontium.
- In this case, a temporary filling is not applied; the tooth remains “open” until the next visit to the dental office. However, before each meal, the patient must always cover the cavity with a carious lesion with a cotton swab to prevent clogging of the root canals with food debris and disruption of the outflow of pus. If there is flux on the gum, it may be necessary to cut the gum.
Features of the treatment of periodontitis in the acute stage
Exacerbation of periodontitis goes through two phases: intoxication and exudation (appearance of discharge). As the disease progresses, the patient first experiences aching and episodic pain, and then constant throbbing and tearing pain, so treatment cannot be delayed.
Acute periodontitis can be serous or purulent. In the second case, purulent exudate accumulates in the apical part of the tooth root, and the main task for the doctor is to remove it. Sometimes this is enough to clean the tooth cavity and treat the canals, but in severe cases it may be necessary to cut the periosteum for drainage.
Treatment of periodontitis at home
Periodontitis cannot be cured at home, since the disease is caused by bacteria that colonize the dental canals. The only way to get rid of them is to carry out antiseptic treatment and sealing of the canals, and this can only be done by a doctor, but by waiting for a visit to the clinic, you can alleviate the symptoms and reduce pain.
Disinfectants that do not irritate the mucous membranes can be used for rinsing 4 - 5 times a day. Doctors also recommend rinsing with a solution of salt and soda, including after treatment, to relieve swelling and reduce inflammation. Non-steroidal anti-inflammatory drugs are suitable for pain relief. All this will help relieve symptoms, but is not a cure.
You may experience pain after periodontitis treatment. Normally, they last 3–5 days and gradually fade away. If the pain does not subside or returns with renewed vigor, re-therapy is necessary.
Why does periodontitis occur?
The most common causes of periodontitis are the following:
- caries in an advanced stage, which was not subjected to timely treatment;
- pulpitis in an advanced stage, lack of modern treatment;
- falls or blows to the jaw;
- poor-quality root canal treatment in the past;
- an inflammatory process that develops under the crown.
At risk of periodontitis is any patient who does not seek help from the clinic in time for caries. The problem often “pops up” in patients who do not attach importance to pain, and ordinary caries over time transforms into a more global pathology of the periodontium and canals.