- Author:
Naumovich Yulia Yakovlevna - Specialty:
Dentist-orthodontist - Category:
Doctor of the highest qualification category
Learn more about the doctor Get a consultation
Periodontitis is an acute or chronic inflammatory process of the root membrane of the tooth and surrounding tissues. It develops against the background of the penetration of infection from the root canal through the hole that is located at the apex of the root due to advanced caries.
This dental disease is characterized by local throbbing pain that gradually increases. Exacerbations of pain occur when the jaw is clenched, as well as when trying to chew on the affected side. Also, the gums next to the affected tooth may become swollen and red. If you have periodontitis, it can be difficult for a patient to eat even liquid soups and soft foods. Sometimes it increases body temperature. The disease is unpredictable in terms of the likely complications that arise, including: acute sepsis, osteomyelitis, inflammatory purulent process. Therefore, when you identify the first symptoms of periodontitis, you should immediately consult a doctor.
Forms of periodontitis
Depending on the location of the inflammatory process, periodontitis is distinguished:
- apical (or apical) – the source of infection is located between the wall of the dental alveolus and the apex of the dental root;
- marginal (or marginal) - inflammation occurs from the edge of the injured gum.
Based on the nature of the inflammation, serous and purulent periodontitis is distinguished, as well as fibrous, granulomatous and granulating.
Classification of periodontitis
There are several classifications of periodontitis, which have more similarities than differences. However, in our country, the classification of I. G. Lukomsky, which provides for the separation of acute (serous and purulent) and chronic (fibrous, granulating and granulomatous) apical periodontitis, as well as chronic aggravated periodontitis, has become most widespread.
Classification of periodontitis according to I. G. Lukomsky is as follows:
- Acute forms.
- Acute serous apical periodontitis.
- Acute purulent apical periodontitis.
- Chronic forms.
- Chronic apical fibrous periodontitis.
- Chronic apical granulating periodontitis.
- Chronic apical granulomatous periodontitis.
- Aggravated chronic apical periodontitis.
- Root cyst.
Causes of acute periodontitis
Among the main reasons for the development of acute periodontitis are:
- acute inflammation of the pulp that occurs against the background of teeth affected by caries; pulp and periodontal tissues are closely related;
- the use of arsenic for pulp devitalization, which provokes inflammation of the pulp tissue due to the toxic effect of the drug penetrating the periodontium;
- the use of strong antiseptics and various cauterizing agents that are injected into the root canal, which provokes inflammation in nearby tissues;
- entry of a large amount of filling material into the periodontal space.
Foreign bodies
Gutta-percha, paper pins, calcium residues and a wide variety of other things can be found in the periapical tissues.
The apical periodontium always reacts to foreign bodies. They can enter through the root canal, through an injured mucous membrane or periodontal pocket.
In the case of paper pin penetration, it should be remembered that the human body does not know how to process cellulose, so the foreign body is surrounded by a bacterial plaque, which maintains inflammation.
Gutta-percha is a biocompatible material. However, at the same time it can give a reaction from the apical periodontium. Studies in guinea pigs have shown that large particles of gutta-percha are encapsulated and surrounded by collagen fibers, while small particles support a local tissue reaction. And magnesium and silicon, which are contained in excess gutta-percha, can cause resorption.
Causes of chronic periodontitis
Approximately 1.5–2 weeks from the moment the first symptoms of the disease appear, it becomes chronic.
Factors that also contribute to the development of chronic periodontitis are:
- advanced form of caries;
- pulpitis;
- advanced acute periodontitis is the most common cause.
Also, chronic periodontitis can develop due to tissue overload due to traumatic occlusion or adentia.
Chronic periodontitis can be infectious or non-infectious.
Causes of infectious periodontitis
Chronic infectious periodontitis can occur due to the presence of many bacteria in the oral cavity: streptococci, staphylococci, porphyromonas, proteus, diphtheroids, yeast-like fungi, etc. Infectious agents enter the tissue through the dentinal tubules or root canal openings, as well as through the bone type of alveoli. The second way is extradental.
Among other causes of infectious periodontitis are chronic odontogenic infections, which include: periodontitis, osteomyelitis, pulpitis (ulcerative), pericoronitis. Often pathogenic organisms enter the oral cavity in the case of tonsillitis or scarlet fever.
Causes of non-infectious periodontitis
Periodontitis of non-infectious origin can occur as a result of trauma to a tooth with damaged periodontium of the intracanal pin. Thus, drug-induced chronic periodontitis develops as a response to the use of resorcinol-formalin or other drugs that provoke coagulative necrosis.
We know how to cure PERIODONTITIS
In the near future, a medical coordinator will contact you and advise you on the conditions and cost of treatment, select a doctor and make an appointment for you.
| Make an appointment | Or call us +375 29 699-03-03 +375 33 319-03-03 |
Symptoms of acute and chronic periodontitis
Symptoms of acute periodontitis are:
- acute pain in the teeth, intensifying at the time of percussion;
- swelling of the lips and cheeks;
- swelling of the gums;
- tooth mobility;
- low-grade fever (37.2-37.7 C);
- enlarged lymph nodes.
Chronic periodontitis is characterized by:
- pain when eating (especially hot);
- sharp pain when biting;
- swelling of the mucous tissues near the affected tooth;
- hyperemia of the oral mucosa;
- the appearance of submucosal, subcutaneous granuloma.
During an exacerbation, a fistulous tract may appear next to the affected tooth, from which pus is released. Often the opening of the fistula tract is localized in the area of the cheeks, cheekbones and chin. Serous-purulent fluid may ooze from the wound. Alternatively, granulation tissue may swell. After an exacerbation, closure of the fistula is observed with the formation of a scar in its place.
The chronic type of granulomatous periodontitis is often asymptomatic. As a result, a greatly enlarged granuloma changes into a cyst, which is characterized by the following clinical manifestations:
- swelling of the gums;
- severe pain in the tooth;
- changes in enamel color;
- hyperemia;
- flux.
If the cyst increases critically in size, even a jaw fracture is likely.
Fibrous chronic periodontitis is characterized by mild symptoms. With this form of the disease there may even be no pain at all. This form of periodontitis is the least dangerous. But in case of exacerbation, the pain can instantly intensify, swelling of the soft tissues of the collateral type is observed, loose teeth and enlarged lymph nodes appear.
Complications of chronic periodontitis include abscess of the soft tissues of the neck and face, meningitis, osteomyelitis of the jaws, periostitis, brain abscess, purulent sinusitis and blood poisoning.
Signs of the disease
The nature of toothache indicates the degree of neglect of the disease. A doctor will help you determine the properties of pain during your consultation.
Making an accurate diagnosis is the doctor’s task, but below are the symptoms of periodontitis:
- prolonged pain or painful throbbing in the tooth or gum;
- increased sensitivity when pressure is applied to the tooth surface;
- asthenia or increased body temperature;
- phantom feeling of tooth swelling;
- swelling of the gums;
- lack of response to cold, hot or sweet;
- easy mobility.
Note! Those places where deep caries treatment was previously carried out are examined. Often, untreated carious disease caused deep tissue damage.
In this case, chronic periodontitis, as a rule, is asymptomatic and is diagnosed only on an x-ray, or when it enters the acute stage.
Diagnostics
Diagnosis of periodontitis is carried out on the basis of a clinical examination, including:
- interviewing the patient,
- visual examination of the oral cavity,
- probing the entrance to the tooth cavity,
- determination of the degree of tooth mobility.
To accurately establish a diagnosis in dentistry, the following is used:
- X-ray examination;
- radiovisiography;
- transillumination;
- electroodontodiagnostics.
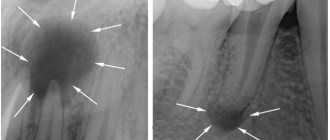
In case of acute inflammation, an X-ray image will not yet show any changes in the periodontium, but in the chronic course of the disease, an X-ray is simply necessary. With its help you can determine the form of chronic periodontitis:
– with fibrous periodontitis, the image will show uneven changes in the lumen of the periodontal fissure; sometimes there is thickening of the root in the apical region. In some cases, sclerosis of the alveolar bone tissue is observed around the source of inflammation.
– with granulating periodontitis, more or less extensive granulations (growths) appear in the periodontium, usually round in shape with unclear boundaries. The image also shows a pronounced deformation of the periodontal fissure and reduced bone density.
– with granulomatous periodontitis, it is clear that the growing granuloma (round in shape with clear boundaries) gradually destroys the bone tissue of the alveoli, developing into a cystogranuloma, and then into a cyst, which begins to grow from the apex of the tooth towards the bone tissue. Such a pathological process usually requires surgical intervention.
Prevention of periodontal inflammation
In order not to encounter chronic periodontitis, avoid complications of dental diseases such as pulpitis and caries. Treatment of caries in all cases is much simpler and faster, and it costs much less than the fight against inflammatory processes in the periodontium.
Remember that regular visits to the dentist once every six months can keep your teeth healthy and protect you from large financial expenses in the future.
In addition, strictly observe oral hygiene, using only high-quality toothpastes to brush your teeth, for example, ASEPTA SENSITIVE, which is specially designed to prevent inflammation of the teeth and gums, as well as provide gentle care for sensitive enamel. The carefully selected ratio of enzymes, thermal mud and herbs in its composition ensures maximum therapeutic and prophylactic effect.
ASEPTA mouthwash will also provide invaluable assistance in creating a healthy microflora that prevents the occurrence of periodontitis. Its regular use can significantly reduce the number of pathogenic microorganisms in the mouth, which most often cause infectious inflammatory processes.
Preventive measures also include a healthy diet. Try to eat as many fresh vegetables and fruits as possible, while simultaneously reducing the amount of sweets and carbohydrates in your diet.
Remember that some medications and orthodontic appliances can also have a destructive effect on teeth. Be sure to use additional oral care products while wearing braces and dentures, as well as in cases when you are forced to take medications that are harmful to tooth enamel.
Take full care of your dental health, and they will not make you experience pain and unpleasant emotions.
Treatment of periodontitis
The treatment regimen for the disease is determined by the stage of its progression and the specific clinical picture. The doctor pays special attention to finding out the cause that provoked periodontitis.
The traditional method of treating the disease includes: the use of pastes that promote the resorption of granulomas and cysts, as well as drugs that activate the restoration of bone tissue. Resection of the apex of the tooth root is prescribed only if therapeutic methods do not bring the expected result. In any case, the doctor strives to preserve the integrity of the tooth as much as possible.
The most important thing in treatment is pain relief and elimination of the source of inflammation in order to spread the infection to other areas of the maxillofacial area. In case of mild infectious periodontitis, it is enough to clean the root canals using an antiseptic.
In case of acute periodontitis, it is necessary to drain the exudate from the canal through the root or gingival canal or the hole remaining after tooth extraction. Then the doctor prescribes antibiotics (sulfonamide medications). If the pain is severe, then analgesics are also prescribed.
After the acute inflammation has been relieved, the doctor begins cleaning the root canal and administering medications. If there is no discharge from the root canals and no pain, the canals are sealed. If exudate is released, then drainage of the canal cavity will follow.
If periodontitis has developed as a result of the action of strong drugs, then treatment begins with eliminating the cause that provoked the disease. First, you should reduce the intoxication of periodontitis by reducing exudation and draining the contents from the root canal. This can be done through mechanical treatment or antidotes that reduce the release of exudate.
If periodontitis is caused by injury, then treatment will be aimed at eliminating it. For example, it may be necessary to grind off a filling that injures the gums. If the damage has led to tooth displacement or damage to a bundle of blood vessels, then it is necessary to check the tooth for electrical excitability. This examination will help identify a possible tooth root fracture.
Treatment of chronic periodontitis is similar to treatment of the purulent type. In this case, the canal is drained to drain the exudate. Next, using an X-ray image, the location of the source of inflammation is clarified, in particular, it is clarified which of the canals should be cleaned first. After relief of inflammation, antimicrobial and instrumental treatment of the root canals is carried out, often using impregnation or physical methods of therapy.
It is worth understanding that after periodontitis, a relapse may occur if the patient soon froze in the cold or suffered another injury. The latter will inevitably lead to tooth extraction and implantation.
Reviews about our doctors
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020