December 21, 2020
Trigeminal neuralgia (facial or trigeminal neuralgia) is a disease of the peripheral nervous system characterized by short-term, intense and repeated pain in the area of innervation of one or more branches of the nerve.
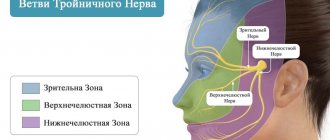
Trigeminal neuralgia (facial or trigeminal neuralgia) is a disease of the peripheral nervous system characterized by short-term, intense and repeated pain in the area of innervation of one or more branches of the nerve. The nerve received its name due to the presence of three branches in it: ophthalmic (upper), maxillary (middle), mandibular (lower).
It is extremely difficult to independently diagnose pathology due to the nonspecific symptoms inherent in many diseases (for example, dental ones). That is why, if any unpleasant sensations occur in the facial area, it is necessary to promptly contact a neurologist. Trigeminal neuralgia most often affects adults, especially the elderly, and is more common in women.
The pathogenesis is not completely clear. It is currently believed that the disease occurs as a result of compression of the trigeminal nerve (at the site of its exit from the pons) by tortuous, pathologically altered vessels or, less commonly, by a tumor. As a result of compression, the nerve root adjacent to the cerebral pons undergoes demyelination. This reason explains up to 80-90% of cases of the disease. Rarely, patients with multiple sclerosis develop a plaque in the area of the sensory nucleus of the trigeminal nerve, which leads to neuralgia.
The factors that most often provoke the development of the disease include: pinching of the trigeminal nerve (temporomandibular joint injuries, congenital anomalies in the development of bone structures of the skull, tumors of the brain and facial area, pathological vasodilatation, etc.); viral nerve damage (herpetic infection, polio); odontogenic infections (“unsuccessful” filling or extraction of teeth or other surgical interventions in the face and oral cavity, reaction to anesthesia of dental canals, dental flux).
What is the trigeminal nerve
The human face has many muscles and nerve endings. Not only the mucous membranes of the nose, pharynx, and conjunctiva, but also the nerve endings can become inflamed. This is most often associated with neurological disorders that change the sensitivity of the fibers that conduct impulses.
With neuropathy of the facial area, acute shooting pain occurs on the right or left. Mirror inflammation of the trigeminal nerve is extremely rare. It is located in the temporal region, near the base of the auricle. And from it there are branches along the entire half of the face:
- jaw nerve (upper and lower);
- optic nerve;
- infraorbital nerve.
The trigeminal nerve passes through the bone tissue in several places, which plays an important role in the occurrence of inflammation associated with pinching. Thus, inflammation of the trigeminal nerve can result in acute pain both in the upper and lower jaw, and in the forehead area, covering the eye sockets.
Symptoms of neuritis
The main symptoms of neuritis are:
Pain along the nerve
The most common symptom of neuritis is pain along the affected nerve. The pain, as a rule, is dull in nature and intensifies in the cold, with physical activity or uncomfortable body position.
Sensory impairment
Sensory loss in the area of the affected nerve is common. It can manifest itself in the form of numbness, tingling, or “pins and needles.”
Decreased muscle activity
There is a partial decrease in muscle strength (paresis), a decrease or loss of tendon reflexes, and in some cases, muscle paralysis (complete cessation of muscle activity).
Vegetative and trophic disorders
With neuritis, there may be such vegetative and trophic disorders as depigmentation of the skin, the acquisition of a bluish tint, local hair loss, increased sweating and dry skin, swelling.
Causes of inflammation of the trigeminal nerve
There are several reasons leading to inflammation of the nerve ducts:
- Poor blood supply associated with physical compression of the nerve. First of all, this is swelling caused by diseases of the ENT organs. The resulting tumor can also pinch the nerves.
- Inflammation associated with dentistry. This includes gingivitis, periodontitis, caries, pulpitis, and eruption of wisdom teeth. Each of these diseases can lead to suppuration, abscesses, swelling and bacterial infections of tissues.
- Medical error by an anesthesiologist - if the injection was given unsuccessfully and the needle got into a nerve, pain cannot be avoided.
- Hypothermia causes muscles to lose their elasticity, which leads to pinching of the nerves passing between the fibers.
- Bacterial infections, in particular tetanus and polio.
- The cause of inflammation of the trigeminal nerve, which is difficult to diagnose, is the psychological state of a person - frequent experiences, stress, and nervous disorders.
To determine the cause of inflammation, you need to consult a specialist.
Causes of neuritis
Local neuritis is caused by:
- local infection;
- local hypothermia;
- injury. Often neuritis develops after a nerve injury;
- compression of the nerve. Thus, neuritis of the axillary nerve can develop due to prolonged use of a crutch, neuritis of the peroneal nerve - due to working in an uncomfortable position, etc.;
- arthritis (in this case the nerve of the joint may become inflamed);
- tumor (if the tumor compresses the nerve).
Multiple neuritis (polyneuritis) can be caused by such reasons as:
- infectious diseases, including measles, herpes, influenza, malaria, diphtheria and some others;
- intoxication. Poisoning with arsenic, lead, mercury, carbon monoxide, phosphorus, bismuth and other highly toxic substances can lead to the development of various types of neuritis. The most common cause of multiple neuritis is alcohol poisoning;
- systemic diseases (diabetes mellitus, rheumatism, gout);
- avitaminosis;
- vascular disorders;
- as well as some other reasons.
Treatment methods
Depending on what caused the inflammation, a course of treatment is prescribed. For bacterial lesions, the emphasis is on antibacterial therapy through systemic administration of drugs.
However, regardless of the reasons, the doctor prescribes painkillers to relieve pain and reduce inflammation. It could be:
- ibuprofen;
- paracetamol;
- analgin;
- ketorol;
- diclofenac.
All of the listed drugs can be prescribed either in the form of tablets for oral administration, or prescribed in the form of solutions for intramuscular administration.
When conservative methods are not possible, the help of a surgeon may be needed. This primarily concerns abscesses due to the eruption of wisdom teeth, pulpitis or other dental diseases. In this case, the abscess will be opened, pus will be removed, the wound will be treated with antiseptic, and the tooth will be removed, if necessary. If a pinched nerve occurs as a result of pathologies in the structure of the skull, the surgeon will perform an operation to correct the situation and free the nerve bundles.
As a complex therapy, massage, heating or exposure to a magnetic field and electric current can be prescribed. You cannot massage or warm the inflamed area yourself, because this can lead to complications associated with rupture of the purulent capsule, blood poisoning and paralysis of the facial nerve.
Separately, you may need to consult a neurologist who will determine the cause of the inflammation if other specialists have not found obvious foci of infection and abscesses.
Traditional methods of treatment are permissible only as an addition to the main therapy. For example, rinsing with chamomile decoction will relieve inflammation and reduce swelling. But you can resort to such procedures only with the permission of the attending physician.
Risk factors
Only those who have had chickenpox can get shingles. But there are certain groups that are more susceptible to postherpetic neuralgia:
- Age – the chance of postherpetic neuralgia is higher in the older age group. (30% of people over 60 years of age who have had herpes zoster subsequently develop postherpetic neuralgia) and only 10% of the younger group develop postherpetic neuralgia.
- Localization of rashes - symptoms of neuralgia are more pronounced if the rashes were in the forehead or eyes.
- Concomitant pathology – The presence of a suppressed immune system (after chemotherapy or taking immunosuppressants) or diseases such as AIDS.
Early treatment of herpes zoster is important. Treatment started within 2-3 days after the rash appears can help reduce symptoms and avoid the risk of postherpetic neuralgia.
Possible complications
Doctors call facial paralysis the first complication that appears in the absence of adequate treatment. This means that a person who does not receive medical care in a timely manner is deprived of the opportunity to express his emotions through facial expressions on one side of his face. This condition can no longer be corrected, which will certainly affect the quality of life. Distortion of facial expressions will lead to the development of depression and constant dissatisfaction with one’s appearance. Not every patient can come to terms with irreversible changes in their appearance without deep distress.
One of the most unpleasant manifestations of paralysis is the inability to close the eyelids on the injured side of the face. In this case, the eye will have to be regularly instilled with artificial tears to prevent the cornea from drying out, since natural hydration through blinking becomes unavailable for this eye.
Diagnostics
Thanks to the characteristic symptoms, establishing a diagnosis for neuritis of the facial nerve does not cause difficulties. Diagnostics is aimed mainly at determining the causes, nature of the inflammatory process, as well as concomitant diseases.
At the initial appointment, the doctor examines and palpates the face, assesses the degree of muscle spasticity and movement disorders. At the same time, he pays attention to the smoothing of natural folds (nasolabial, frontal, etc.), as well as to the non-closure of the eyelids (the inability to close the eye).
For this purpose, several standard tests are performed in which the patient is asked to close his eyes, try to smile, close his eyes, frown, wrinkle his forehead, puff out his cheeks, blow, wrinkle his nose, raise his eyebrows, and bare his teeth. In addition, the taste sensitivity of the tongue is determined.
If additional data is needed, the patient is sent for an MRI or CT scan to identify possible lesions of the brain, blood vessels (in particular, the presence of a tumor, hematoma, aneurysm, etc.), and the presence of inflammatory foci.
To assess the affected area and disturbances in the innervation of facial muscles, electromyography (EMG) is used - a method for studying bioelectrical activity. Using electroneurography, the speed of signal transmission through nerve channels (fibers) is assessed.
In addition, a general urine and blood test and a biochemical blood test are performed.
Important! Eastern medicine views the human body as a single system. Inflammation of the peripheral nerves in this context represents a particular, local manifestation of a general imbalance, almost never the only one.
Therefore, when diagnosing neuritis, a doctor of oriental medicine assesses the degree of imbalance as a whole, identifies concomitant diseases, disorders, functional disorders of the nervous, hormonal, reproductive, immune and other systems.
A treatment plan is designed to address the common causes of all these disorders.
Prevention of inflammation
To prevent the risk of developing inflammation of the trigeminal nerve, it is recommended to follow a number of measures:
- monitor oral hygiene and consult a dentist in a timely manner;
- do not stay in the cold for a long time or protect your face from freezing with a scarf;
- do not self-medicate otitis media.
At the first manifestations of pain on the face, you should immediately consult a doctor. This will stop the development of inflammation. In addition, early diagnosis allows for conservative treatment methods.
What to do in case of an attack of pain?
At the first stage, first of all, you should observe bed rest, limit any movements, it is better to take a pose with support on your healthy leg. When lying on your back, it is recommended to place a small pillow under your lower back and knees. If you cannot lie down, you should shift your weight from one leg to the other alternately and move more often. With light dynamic movements, the muscles relax faster. Take pain medication as prescribed by your doctor.
At the second stage, you can use dry heating (a warm heating pad, a heat-retaining blanket) or a compress with herbal tinctures on the affected area. It is not recommended to use heat at elevated temperatures. In the absence of contraindications, you can perform a massage with rubbing and kneading of the lumbar region and limbs.
To prevent relapses, it will be useful to wear a fixing corset, and for pregnant women, a prenatal bandage if there is a noticeable increase in the abdomen. All intramuscular injections should be performed by trained medical personnel and placed only in the unaffected leg.
What should you avoid if you have sciatica?
First of all, you should avoid hypothermia: do not stay in the cold or open wind for a long time, do not lie on cold surfaces, do not swim in cold water. To strengthen the immune system, you need to strengthen the body with exercise therapy, water treatments, yoga, and massage.
It will be important to change your occupation if it involves heavy physical work. It is also necessary to limit long stays in one position, sharp bends and turns of the body, running, fast walking, and transferring the entire body weight to the affected leg.
If you tend to be overweight, it is recommended to create a diet. Excess weight will aggravate the inflammatory process and increase pain.