Signs of trigeminal neuralgia
A typical symptom of trigeminal neuralgia is prosopathy - facial pain. The sensation can be compared to an electric shock. Pain of a paroxysmal nature lasts 5-15 seconds and occurs abruptly. It is usually localized in the area of the lower jaw and cheekbones, but can appear in any part of the face. Neuralgia in severe form leads to partial or even complete loss of sensitivity.
Other symptoms:
- nervous eyelid tic;
- impaired coordination of movements;
- increased body temperature;
- headache;
- chills, fever;
- general weakness.
Trigeminal neuralgia
Trigeminal neuralgia (TN) - (synonyms: tic douloureux, or Fothergill's disease) is one of the most common facial pain (prosopalgia - (Greek prosopon (face) + algos (pain)) and is one of the most persistent pain syndromes in clinical neurology TN is a typical example of neuropathic pain and is considered the most painful type of prosopalgia. TN most often has a chronic or recurrent course, much more difficult to treat than many other types of chronic pain. High intensity and persistence of trigeminal neuralgia, its special, often painful nature, resistance traditional methods of pain relief give this problem exceptional relevance. According to WHO, the prevalence of TN is up to 30–50 patients per 100,000 population, and the incidence is 2–4 people per 100,000 population. TN is more common in women than in men, debuts in fifth decade of life and in 60% of cases has a right-sided localization.Causes of TN The most common cause of TN is compression of the proximal part of the trigeminal root within a few millimeters from the entrance of the root to the pons (i.e. n. "entry zone of the spine"). In approximately 80% of cases, compression occurs by an arterial vessel (most often a pathologically tortuous loop of the superior cerebellar artery). In other cases, such compression is caused by an aneurysm of the basilar artery, space-occupying processes in the posterior cranial fossa, tumors of the cerebellopontine angle and multiple sclerosis plaques. At the extracranial level, the main factors leading to the occurrence of TN are: tunnel syndrome - compression in the bone canal through which the nerve passes ( often in the infraorbital foramen and lower jaw), associated with its congenital narrowness, the addition of vascular diseases in old age, as well as as a result of a chronic inflammatory process in adjacent areas (caries, sinusitis); local odontogenic or rhinogenic inflammatory processes. The development of TN can be provoked by infectious processes, neuroendocrine and allergic diseases, demyelination of the trigeminal nerve root in multiple sclerosis.
Clinical manifestations of TN
The disease, in most cases, develops on one side; a bilateral process is extremely rare. First, pain occurs at the site of innervation of any of the three branches; later, as the disease progresses, pain can gradually cover areas of the face innervated by neighboring branches. The localization of pain depends on which branches are involved in the process:
- when the first branch is affected, pain is localized in the area of the superciliary arch, forehead, temple, sometimes pain occurs in the eyelids and eyeball;
- when a pathological process occurs in the second branch, pain occurs in the upper lip, wing of the nose, in the projection of the zygomatic bone, upper cheek, upper jaw and palate;
- when the third branch is affected, the pain zone is localized in the lower lip, chin, cheek, lower jaw, half of the tongue and soft palate.
Taxonomy of trigeminal prosopalgia
From the point of view of topical diagnosis, the development of any form of trigeminal prosopalgia is associated with damage to the peripheral trigeminal neuron - the peripheral trigeminal branches, the sensory trigeminal ganglion (located at the base of the skull), the sensory root of the trigeminal nerve that follows it in the direction of the brain stem, as well as those entering the brain stem sensory trigeminal fibers and sensory nuclei of the trigeminal nerve. Depending on the impact of the pathological process on the corresponding part of the trigeminal system, TN is divided into predominantly central and peripheral genesis. In the occurrence of TN of central origin, neuroendocrine, immunological and vascular factors play an important role, which lead to impaired reactivity of cortical-subcortical structures and the formation of a focus of pathological activity in the central nervous system. In the pathogenesis of peripheral TN, the compression factor, infections, injuries, allergic reactions, and odontogenic processes play an important role. Despite the difference in the symptomatology of the clinical forms of trigeminal prosopalgia, the features of facial pain are of primary importance for their differentiation, in some cases manifested by prolonged (constant) pain, and in others in the form of paroxysms of pain. Paroxysmal forms of trigeminal pain are traditionally referred to as neuralgia, and non-paroxysmal forms - trigeminal neuropathy. These forms of facial pain—neuralgia and trigeminal neuropathy—fundamentally differ in their approaches to treatment. Deafferentation trigeminal neuropathy (prosopalgia)
Deafferentation facial pain (prosopalgia) is the most severe form of trigeminal lesion, manifested by highly intense facial pain, often resistant to conservative therapy, and severe sensory impairment. Develops as a result of significant damage (destruction) of the peripheral or central structures of the trigeminal system. The concept of “deafferentation trigeminal prosopalgia”, as a general syndromological definition, was proposed by Yu. V. Grachev and Yu. A. Grigoryan (1995) to designate a special form of facial pain that develops as a result of deafferentation in the sensory system of the trigeminal nerve. The pathophysiological term “deafferentation” (de- + lat. afferentis bringing), literally means the separation of the receptor zones of peripheral nerves from the central sensory structures, due to a violation of the integrity or conductivity of nerve fibers. Typical peripheral forms of deafferentation trigeminal prosopalgia are postherpetic, tumor and iatrogenically caused facial pain (caused by destruction of the ganglion and trigeminal nerve root), and central are two quite rare forms caused by syringobulbia and medulla oblongata infarction.
Diagnostics of TN
Clinical interview plan for the evaluation of patients with facial pain. Description of pain:
- Localization of pain
- Temporary characteristics of pain (paroxysmal/non-paroxysmal, prolonged)
- Frequency of pain attacks
- Pain intensity
- Sensory nature of pain
- Other sensations accompanying facial pain (associated signs)
- Conditions and time of pain occurrence
- Medicines (other factors) that reduce or eliminate pain
Anamnestic data:
- Duration of the disease
- Conditions for the development of the first exacerbation
- The nature of the course of prosopalgia (acute, recurrent, continuous)
- Frequency of exacerbations of prosopalgia
- Previous treatment
- Disorders (neurological, somatic) accompanying the development of the disease.
When conducting palpation examination of the facial area, it is necessary to distinguish between “neuralgic” and “myofascial trigger” (English trigger). Neuralgic trigger points or zones (in patients with trigeminal neuralgia) are hyperexcitable areas of the skin and mucous membrane, with mechanical irritation, including light touch, causing a painful attack. At the same time, strong pressure, usually applied by the patient himself, not only does not cause pain, but in some cases leads to a decrease or disappearance of pain. Myofascial trigger points (essentially pain points) are located in the soft tissues of the face in the projection of the masticatory muscles. “Pressing” on them is accompanied by localized or radiating pain.
Treatment of TN The main directions of drug therapy are:
- elimination of the cause of TN, if it is known (treatment of diseased teeth, inflammatory processes in adjacent areas, etc.),
- carrying out symptomatic treatment (pain relief).
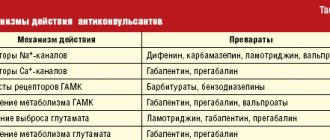
- Anticonvulsants are the drugs of choice for the treatment of TN, and carbamazepine was one of the first drugs officially approved for the treatment of this condition.
In the early 90s of the last century, a new generation of antiepileptic drugs appeared, and now anticonvulsants are usually divided into first and second generation drugs. First-generation drugs are practically not considered as the first line of treatment for NB (with the exception of carbamazepine for TN). Second generation anticonvulsants include pregabalin (Lyrica), gabapentin (Neurontin, Gabagamma, Tebantin), lamotrigine (Lamictal), oxcarbazepine (Trileptal), topiramate (Topamax), levetiracetam (Keppra), tiagabine (Gabitril), zonisamide (Zonegran), vigabatrin (Sabril), felbamate (Taloxa). These drugs have more favorable pharmacokinetic characteristics and safety profiles, as well as a lower risk of drug interactions compared to first-generation anticonvulsants. According to the recommendations of the European Federation of Neurological Societies (2009), pharmacotherapy for TN is based primarily on the use of carbamazepine (Finlepsin, Tegretol) proposed by S. Blum in 1962 (200–1200 mg/day), which is the drug of first choice (level of evidence A) . The analgesic effect of this drug is mainly due to its ability to reduce the permeability to sodium of the membranes of neurons involved in nociceptive reactions. The following treatment regimen with carbamazepine is usually prescribed: in the first two days the daily dose is 200 mg (1/2 tablet in the morning and evening), then within two days the daily dose is increased to 400 mg (morning and evening), and after that - to 600 mg (1 tablet in the morning, lunch and evening). Gabapentin (Neurontin) is the first drug in the world to be registered for the treatment of all types of neuropathic pain. Many studies have shown the effectiveness of gabapentin in patients with TN who do not respond to treatment with other drugs (carbamazepine, phenytoin, valproate, amitriptyline); in most cases, complete relief of pain was observed. The therapeutic dose ranges from 1800 to 3600 mg/day. The drug is taken 3 times a day according to the following regimen: 1st week - 900 mg/day, 2nd week - 1800 mg/day, 3rd week - 2400 mg/day, 4th week - 3600 mg/day. The results of an open-label, prospective, 12-month study of 53 patients with TN were recently published, evaluating the effectiveness of pregabalin (Lyrica) at a dose of 150–600 mg/day. Treatment with pregabalin resulted in pain relief or at least a 50% reduction in pain intensity in 25% and 49% of patients, respectively. The use of levetiracetam (Keppra) in the treatment of TN was first reported in 2004 by KR Edwards et al. The properties of this drug are particularly suitable for the treatment of TN patients with severe pain who require a rapid response to therapy. Unlike other anticonvulsants, especially carbamazepine, the hepatic cytochrome P450 system is not involved in the metabolism of levetiracetam and the drug is excreted through the kidneys. In addition, this drug has a favorable therapeutic index and has few adverse side effects (which is the main problem when using drugs to treat TN). A 10-week, prospective, open-label study showed that higher doses of levetiracetam, ranging from 3000–5000 mg/day (50–60 mg/kg/day), were required for the treatment of TN compared with the treatment of epilepsy, but did not caused significant side effects. This circumstance indicates the prospect of using this drug for the treatment of TN. Since the 1970s, antidepressants have been used to treat TN. Currently, the effectiveness of the use of tricyclic antidepressants (TCAs) in the treatment of TN has been proven. Pathogenetic treatment of patients with TN includes the use of drugs with neurometabolic, neurotrophic, antioxidant, and antihypoxic effects. In recent years, high efficiency of the use of metabolic drugs has been discovered. In the treatment of patients with TN, the high effectiveness of the metabolic drug Actovegin, a deproteinized derivative from the blood of young calves, has been shown. The main effect of this drug is to stabilize the energy potential of cells. Actovegin also has an antihypoxic effect, being an indirect antioxidant. In addition, the effect of Actovegin is manifested by indirect vasoactive and rheological effects by increasing capillary blood flow, reducing peripheral vascular resistance and improving the perfusion of organs and tissues. During an attack, it is advisable to use Actovegin intravenously in a slow stream or drip for 10 days at a dose of 400–600 mg/day. In the interictal period, the drug is prescribed orally at a dose of 200 mg 3 times a day for 1–3 months. The pathogenetic treatment of patients with TN includes the use of high doses of B vitamins as part of multicomponent preparations, which is due to their multimodal neurotropic effect (impact on metabolism, metabolism of mediators, transmission of excitation in the nervous system), as well as the ability to significantly improve nerve regeneration. In addition, B vitamins have analgesic activity. Such drugs, in particular, include Milgamma, Neuromultivit, Neurobion. Until now, the selection of analgesic therapy for NB is more an art than a science, since the choice of drugs is carried out mainly empirically. There are often situations when the use of one drug is not effective enough and there is a need for a combination of drugs. Prescribing “rational polypharmacotherapy” (simultaneous use of drugs with neurotropic, neurometabolic and analgesic mechanisms of action) allows increasing the effectiveness of treatment with lower dosages of drugs and fewer side effects.
Differentiated therapeutic approaches for paroxysmal and non-paroxysmal trigeminal prosopalgia.
Differentiated therapeutic approaches for paroxysmal and non-paroxysmal trigeminal prosopalgia
| Paroxysmal paroxysmal facial pain Duration of painful attacks: from several seconds (instant pain") to several minutes | Non-paroxysmal (long-lasting) facial pain |
| Clinical forms Trigeminal neuralgia - typical trigeminal neuralgia - trigeminal neuralgia with neuropathic manifestations (after “therapeutic blockades”) - trigeminal neuralgia in multiple sclerosis - symptomatic trigeminal neuralgia in tumors of the base of the skull and brain | Clinical forms Trigeminal neuropathy - odontogenic - traumatic - herpetic (including postherpetic neuralgia) - autoimmune (in systemic rheumatic diseases) Deafferentation trigeminal prosopalgia (high-intensity constant pain) - iatrogenic ("destructive") - postherpetic - tumor |
| Main treatment approaches - carbamazepine - a basic drug that helps suppress pain attacks - Milgamma, Milgamma-compositum Physiotherapy, reflexology - If conservative treatment of typical trigeminal neuralgia is ineffective - neurosurgical decompression of the trigeminal nerve root | Main treatment approaches - NSAIDs (diclofenac, ibuprofen, meloxicam) - gabapentin (Gabamma) - for herpetic and traumatic neuropathy, deafferentation prosopalgia - amitriptyline - for herpetic neuropathy (postherpetic neuralgia) - Milgamma, Milgamma compositum - Physiotherapy, reflexology |
For patients suffering from unbearable pain for a long time, and if conservative therapy is ineffective in the case of classical TN, surgical treatment is recommended. The following approaches are currently used:
- surgical microvascular decompression;
- stereotactic radiation therapy, gamma knife;
- percutaneous balloon microcompression;
- transdermal glycerol rhizolysis;
- Percutaneous radiofrequency treatment of the Gasserian node.
In conclusion, we note that the treatment of TN should be multidisciplinary in nature, and the choice of various treatment methods and the risks of possible complications should be discussed with the patient.
Causes of neuralgia
Unlike neuritis, which is an inflammatory disease, neuralgia is not. Neuritis develops against the background of a virus and infection. Neuralgia occurs due to mechanical effects on the trigeminal nerve, provoked by various factors.
- Head injuries with displacement of the skull bones.
- Tumors of various etiologies, which, as they grow, compress the trigeminal nerve.
- Bite defects and other anomalies of the dentofacial area.
- Diseases of blood vessels located in close proximity to the trigeminal nerve.
- Chronic sinusitis and otitis.
- Medical error during tooth extraction.
- Neuralgia can be triggered by infections, including periodontitis, stomatitis, herpes, and syphilis.
Hypothermia does not cause neuralgia, but makes treatment difficult. Neurosis, metabolic disorders, diabetes mellitus and other chronic pathologies have a negative effect on therapy.
Types of neuralgia
Neuralgia that develops as a result of viruses and other diseases is called secondary. Primary or idiopathic is a disease caused by compression of a nerve. According to localization, it can be unilateral or bilateral. With unilateral neuralgia, one branch of the nerve is affected, with bilateral neuralgia, several.
According to the nature of the disease, it can be acute or chronic. With acute neuralgia, the patient experiences frequent and severe pain. If the pathology is not treated, it goes into a chronic stage, when exacerbation is replaced by periods of remission.
Postherpetic neuralgia develops after herpes and differs from the classic nature of the pain, which may not go away for several hours. An atypical form of neuralgia is a psychosomatic disease, which can be triggered by stress, depression, and nervous exhaustion.
Methods for diagnosing neuralgia
The disease is diagnosed using different methods that make it possible to establish its cause:
- visual examination and questioning of the patient;
- radiography;
- MRI of the head;
- biochemical studies of blood and urine;
- electromyography.
To clarify the diagnosis, the neurologist often turns to doctors of other specialties - otolaryngologist, ophthalmologist, orthodontist. This is done to exclude diseases for which the same symptoms are typical.
Drug treatment of neuralgia
Effective treatment is only possible with the use of a comprehensive drug regimen. Anticonvulsants are prescribed first. Antihistamines and local analgesics are sometimes added to them to relieve acute attacks of pain. The deficiency of gamma-aminobutyric acid will be compensated by phenibut and similar neotropic drugs. In case of exacerbation, antidepressants may be prescribed. If the disease is caused by a viral infection, the patient is prescribed non-steroidal antiviral and antibacterial drugs.
Other treatments
To eliminate pain, physiotherapeutic procedures are prescribed: acupuncture, magnetic therapy, ultraphonophoresis. A good addition to drug treatment is head and face massage. If conservative treatment methods do not bring the desired effect, the patient may be prescribed a minimally invasive operation - microsurgical decompression, radiosurgery or percutaneous destruction.
Trigeminal neuralgia is not only painful, but also causes problems with the patient’s communication abilities. Constantly expecting attacks of pain, a person isolates himself from others, withdraws into himself, becomes irritable and depressed. The prognosis for treatment is favorable. The chances of a full recovery increase when the patient consults a doctor at an early stage of the development of neuralgia, when the first symptoms appear.
Trigeminal nerve lesions
Trigeminal neuralgia - there are two forms of neuralgia: primary (idiopathic, typical, essential), secondary (symptomatic). Primary trigeminal neuralgia develops independently, without any dependence on a pathological process or condition already existing in the body. Secondary neuralgia is essentially a complication of an existing disease, i.e. is a symptom complex of the disease.
CLINICAL PICTURE
Trigeminal neuralgia is characterized by the appearance of intense pain attacks. The localization of pain is determined by the zone of innervation of the affected branch of the trigeminal nerve. The duration of a painful attack ranges from several seconds to several minutes. The attack occurs suddenly, just as it stops. The interictal period is characterized by the absence of pain. Typically, a painful attack is accompanied by a reflex contraction of the facial muscles (facial and chewing) and vegetative manifestations, such as hypersalivation, lacrimation, facial hyperemia. During a painful attack, patients can take forced positions that bring relief, sometimes holding their breath, or breathing heavily. To reduce the intensity, patients squeeze or rub the painful area with their fingers. Mechanical or thermal irritation of trigger zones innervated by the branches of the trigeminal nerve can provoke the development of a pain attack. These areas include areas of the facial skin, mucous membranes, and teeth. In most cases, trigger areas are located in the gum area and around the mouth.
Optic neuralgia occurs in very rare cases. This disease is usually confused with other diseases that present with similar symptoms. Such diseases can be a local inflammatory process, frontal sinusitis, etc. More often, trigeminal neuralgia involves the maxillary or mandibular nerves. During a painful attack, or immediately after the last one, pain points located at the exit points of the branches of the trigeminal nerve are determined. In addition, areas of hyperesthesia are found in places of innervation in some cases. An objective examination in the interictal period does not reveal any organic symptoms of the disease. During an attack, the pain can be of a different nature: burning, tearing, cutting, shooting, stabbing, “electric shock”. Painful attacks may not be isolated, but follow each other at short intervals.
The duration of remission ranges from several months to several years. It can occur spontaneously, but more often as a result of treatment. One of the treatment methods is alcoholization of the peripheral branches of the trigeminal nerve. In this case, remission occurs quickly. With repeated alcoholism, the effectiveness of treatment decreases and the duration of the remission period is reduced. A complication of alcoholism is the addition of iatrogenic neuritis of the trigeminal nerve, which develops as a result of destructive changes in this nerve.
SYMPTOMS
When the nucleus of the spinal tract is damaged or damaged, a segmental type of sensitivity disorder develops. In some cases, loss of pain and temperature sensitivity is possible while maintaining deep types of sensitivity, such as the feeling of vibration, pressure, and others. This phenomenon is called dissociated sensory disorder.
In case of irritation of the motor neurons of the trigeminal nerve, trismus develops, i.e., tonic tension in the masticatory muscles. Trismus is characterized by strong compression of the teeth of the upper and lower jaw, and strong tension in the masticatory muscles. On palpation, the masticatory muscles are very hard. In addition, the presence of pronounced neuropsychic stress is characteristic. Long-term persistent trismus leads to exhaustion of the patient.
In the case of inflammation of the facial nerve, a characteristic symptom is the appearance of pain in half of the face, corresponding to the side of development of inflammation. In most cases, the pain is localized in the ear area and behind the mastoid process. In more rare cases, the pain is localized in the upper and lower lips, forehead, and lower jaw. Unilateral paresis or paralysis of the masticatory muscles occurs when the motor nucleus of the trigeminal nerve or the motor fibers of the mandibular nerve on the same side are damaged. This pathology is characterized by the opening of the mouth from the masticatory muscles with impaired motor innervation. In the case of bilateral damage to the same nerve formations, the lower jaw sag.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable. For short duration of the disease, patients are prescribed anticonvulsants. If drug therapy is ineffective, surgical treatment methods are used.