Pathological processes occurring in the 5th paired cranial nerve - the trigeminal nerve - give rise to such complex symptoms that in medicine it is considered not as a single nerve, or even as a plexus, but as an entire system consisting of:
- from one motor and three sensory nuclei;
- sensory and motor roots;
- Gasserian (lunate) trigeminal ganglion, which contains sensory neurons;
- three branches (ophthalmic, submandibular and mandibular).
The trigeminal nerve has mixed functions: it is responsible for the sensitivity of the face, as well as the oral cavity, but in addition, it ensures the functioning of the chewing jaw muscles.
Anatomy of the trigeminal nerve
The trigeminal nerve begins from the sensory and motor roots, anatomically connected to each other and originating from the dorsal horns of the spinal cord and nuclei of the brain. The roots can change their fibers. The diameter of the sensitive root is from 2 to 2.8 mm, the diameter of the motor root is from 0.8 to 1.4 mm. These roots emerge from the base of the middle cerebellar peduncle, which arises from the pons.
The Gasserian trigeminal ganglion (trigeminal plexus, ganglion) is located on the depressed area of the temporal bone in the layers of the dura mater. It reaches a length of up to 30 mm and a height of up to 10 mm.
How the ascending and descending tracts of the trigeminal nerve are formed
- Nerve cells of the Gasserian ganglion have processes that branch into axons (central processes) and dendrites (peripheral processes), in which the first sensory neurons of the T.N.
- The axons form a sensory root that follows three sensory nuclei (pons, spinal tract of the pons and medulla oblongata, midbrain tract), in which the second neurons are located.
- The axons of the second neurons of the sensory nuclei as part of the medial lemniscus along the trigeminal lemniscus are directed to the thalamus, while on the way to it some of the axons pass to the other side.
- On the cells of the ventrolateral nuclei of the visual thalamus there are third neurons, the axons of which follow to the postcentral gyrus of the brain.
- The descending motor root of the trigeminal nerve originates in the first neurons of the postcentral gyrus, located in the cerebral cortex, and goes to the second peripheral motor neurons of the nucleus of the posterior part of the pons, the axons of which form the motor root.
In Fig. Pathways and nuclei of the trigeminal nerve.
The transmission of impulses along the trigeminal nerve is carried out according to the principle of a reflex arc.
From the irritated receptor, the impulse travels through three or four links:
- afferent, transmitting impulses from sensory receptors to the central nervous system;
- central link (brain) - it does not always participate in the arc, since reflex axons do not transmit the signal to the center;
- efferent link - transmits impulse from the center to the executive organ (effector);
- effector - an organ that responds to a reflex.
The peripheral processes of the trigeminal nerve, depending on the nature of the irritation - external or deep, send an impulse to the nucleus of superficial sensitivity, located in the spinal tract, or to the nucleus of deep sensitivity, located in the dorsolateral region of the tegmentum of the pons.
Treatment methods
Inflammation of the trigeminal nerve and neuralgia are treated in a comprehensive manner and only under the guidance of specialists. This is taking antibiotics, NSAIDs, glucocorticoids, muscle relaxants and anticonvulsants, coupled with novocaine blockades. Additionally, a number of physiotherapeutic procedures are prescribed. If these measures do not bring the desired result, surgical intervention is required. Depending on the clinical case, radiofrequency destruction or microvascular decompression is prescribed.
You can read more about the treatment of neuritis and neuralgia in a separate article.
Innervation of the trigeminal nerve
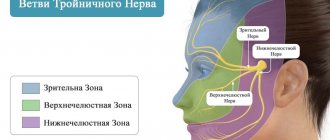
Each of the three branches of the trigeminal nerve also branches into three branches:
- one stretches to the hard shell of the g.m.;
- internal branches are directed to the mucous membranes of the nasal cavity, paranasal sinuses, lacrimal salivary glands, and also to the teeth;
- external medial and lateral branches - respectively to the anterior and lateral surfaces of the face.
Rice. Diagram of the branching of the trigeminal nerve.
Optic nerve
- The optic nerve is mainly composed of sensory neurons.
- The thickness of the optic nerve is up to 3 mm.
- Innervation: frontal region, temporal, parietal, wings of the nose; upper eyelid, eyeball, paranasal sinuses, nasal mucosa (partially).
Maxillary nerve
- Only sensitive.
- Thickness from 2.5 to 4.5 mm.
- Innervation: dura mater, anterior temporal region; lower eyelid; outer corner of the eye, upper cheek areas, mucous membranes of the maxillary maxillary sinus and upper lip.
- Divided into nodal branches: meningeal branch (goes to the membrane of the g. m.),
- branch going to the wings of the nose and palate;
- zygomatic, hypoglossal and infraorbital nerves.
The infraorbital nerve has a wide branching of the superior and inferior alveolar nerves, external and internal nasal nerves, innervating the upper jaw and teeth, respectively, the skin of the lower eyelid, the skin of the nasal wing, the mucous membranes of the nasal inlets and the upper lip.
Mandibular nerve
- Mixed (both sensory and motor).
- It is the most powerful, its thickness can exceed 7 mm.
- Sensitive innervation: hard shell of the brain, skin of the chin, lower lip, lower cheek area, anterior area of the auricle, ear canal, eardrum, two-thirds of the tongue, lower teeth, mucous membrane of the cheeks and lower oral cavity.
- Motor innervation: muscles of mastication, muscles of the tympanic membrane, palate, mylohyoid and digastric muscles.
- Forms many nerves: meningeal, chewing, temporal, pterygoid, buccal, auriculotemporal, lingual, etc.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Causes and types of damage to the trigeminal nerve
- Damage to the trigeminal nerve can occur at different levels, and the following may be affected: branches (ophthalmic, maxillary, mandibular);
- sensory and motor roots;
- nuclei of the brainstem, spinal and midbrain tracts;
- Gasser knot.
Damage to the trigeminal nerve can be caused by:
- Severe hypothermia of the face and head.
- Infectious and toxic processes.
- Sick teeth.
- Pathologies of the upper and lower jaw, maxillary sinuses, upper cervical region.
- Herpes virus.
- Degenerative, dyscirculatory diseases of the brain (bulbar, pseudobulbar palsy, etc.)
- Endocrine diseases, vascular pathologies, allergies.
- Carotid artery aneurysm.
- Inflammation of the temporal bone.
- Psychogenic factors.
Next, we will consider the symptoms and treatment for damage to the trigeminal nerve.
Possible complications
Doctors call facial paralysis the first complication that appears in the absence of adequate treatment. This means that a person who does not receive medical care in a timely manner is deprived of the opportunity to express his emotions through facial expressions on one side of his face. This condition can no longer be corrected, which will certainly affect the quality of life. Distortion of facial expressions will lead to the development of depression and constant dissatisfaction with one’s appearance. Not every patient can come to terms with irreversible changes in their appearance without deep distress.
One of the most unpleasant manifestations of paralysis is the inability to close the eyelids on the injured side of the face. In this case, the eye will have to be regularly instilled with artificial tears to prevent the cornea from drying out, since natural hydration through blinking becomes unavailable for this eye.
Symptoms of trigeminal nerve damage
Since damage to the trigeminal nerve occurs at different levels of the central nervous system and PNS, it leads to a large number of disorders: motor, sensory, reflex, somatic, autonomic.
Symptoms of damage to the motor root and nucleus
If the root of the third branch is affected:
- Atrophy and paralysis of the masticatory muscles.
- Deviation of the jaw when trying to move it towards paralysis.
- Sensory disturbances.
- With bilateral peripheral lesions, the jaw is completely immobile, it hangs down, and the mandibular reflex disappears.
- Changes in facial contour due to recession of the temporal region.
If the central motor nucleus is affected (in the tegmentum of the cerebral pons), then central paralysis of the masticatory muscles is observed only with bilateral lesions, since the motor impulse comes from both the own hemisphere and the opposite cortex.
Symptoms of central bilateral lesion of the motor nucleus:
- central paralysis of the jaw masticatory muscles;
- absence of muscle atrophy;
- strengthening jaw reflexes;
- the occurrence of a strong tonic convulsion (trismus), which does not go away for a long time: it is impossible to unclench the jaw, and the patient’s facial expressions may be distorted.
In the photo: a patient with a central lesion of the motor nuclei of the trigeminal nerve.
Infections and intoxications, such as tetanus or rabies, can contribute to central motor damage to the trigeminal nerve.
Symptoms of sensory impairment due to damage to the trigeminal nerve
Sensory disturbances can be of a peripheral (superficial) and segmental (deep) type.
Pathologies of the first type are possible with lesions of the trigeminal gasserian plexus, branches of the trigeminal nerve, and sensory root.
With peripheral disorders, symptoms appear:
- pain in the half of the face with which the affected nerve is located;
- hypoesthesia (decreased sensitivity), anesthesia (complete loss of sensitivity), less often - hyperesthesia (increased sensitivity);
- decreased jaw reflexes.
Segmental disorder is associated with damage to the nucleus located in the spinal cord near the medulla oblongata and the pons, so its symptoms are similar to those that occur with damage to the posterior horns of the spinal cord (loss of temperature and pain sensitivity), but it does not occur on the trunk and limbs , but on the face. Tactile and deep sensitivity are preserved.
The location of Zelder's concentric zones of sensitivity loss in the diagram below (they are indicated by brackets on the right, on the left - the zones of innervation of T.N.):
- damage to the upper part of the sensory nucleus - the zone of loss of sensitivity is located around the mouth and nose;
- damage to the middle part of the nucleus - the affected area affects the frontal surface, cheeks, area under the lower lip;
- damage to the lower, caudal part of the nucleus - facial lateral and parotid areas.
Segmental disorders caused by damage to the nucleus of the brain stem, at the level of the tegmentum of the pons, occur not on the side of the lesion, but on the opposite side (alternating Wallenberg syndrome).
Autonomic disorders with damage to the trigeminal nerve
Autonomic disorders with damage to the optic nerve, jaw nerves and Gasserian ganglion manifest themselves in dysfunction of the facial glands (lacrimal, salivary, sweat, sebaceous), which leads to:
- to increased dryness in the eye;
- lack of lacrimation;
- impaired salivation and sweating;
- keratitis (with damage to the gasserian node);
- ulceration of the skin in the nasolabial folds and on the wings of the nose;
- swelling and redness on the face.
Reflex disorders with damage to the trigeminal nerve
The trigeminal nerve is involved in the formation of deep (supraglacial, zygomatic) reflexes and superficial (for example, corneal) reflexes: the afferent link is located in the first and second branches, and the efferent link is in the facial nerve.
When the ocular and jaw nerves are damaged, deep reflexes (supraglacial, maxillary and mandibular) and corneal surface reflex (corneal and conjunctival) decrease or disappear: if the corneal reflex is impaired, the corneal reflex disappears and the sensitivity of the nasal mucosa decreases.
With damage to the cortical-nuclear nerve pathways, on the contrary, they intensify.
Trigeminal neuralgia
Trigeminal neuralgia or trigeminal neuralgia is a chronic disease manifested by a variety of symptoms, the main one of which is severe pain.
Neuralgia requires complex treatment, and it is not always possible to cure it, and then you have to resort to surgery. There are two types - central and peripheral, depending on which structures of the trigeminal nerve are affected.
Neuralgia is more common in women after forty years of age, who experience age-related hormonal changes.
Central neuralgia
Causes of central neuralgia T.N.:
- endocrine and vascular diseases;
- metabolic disorders;
- allergy;
- psychogenic factors.
Symptoms:
- a sudden attack of very severe pain in the 2nd or 3rd zone. or simultaneously in both branches of the trigeminal nerve;
- the pain is so strong that the patient literally freezes, grabs his face, rubs it, his facial expressions are distorted;
- the pain lasts a few seconds and also suddenly disappears;
- autonomic disorders are observed (lacrimation and salivation increase, the skin on the face turns red).
The attack may not recur for several months or even years. With chronic long-term central trigeminal neuralgia, the following occurs:
- Trophic disorders: facial skin becomes dry, flaky;
- facial muscles - flabby;
- hair turns grey.
Peripheral neuralgia
Peripheral trigeminal neuralgia is associated with:
- with pathologies of the teeth and jaw (odontogenic neuralgia) - osteomyelitis of the jaw, pulpitis, periodontitis, unsuccessful tooth extraction or prosthetics, etc.;
- with dental plexus neuralgia (dental N.) - in addition to odontogenic factors, it can be provoked by diseases of the neck and sinuses; jaw joint;
- damage to the Gasserian node and nerves of the peripheral system of the T.N.;
- herpes (herpetic N.).
Odontogenic and dental neuralgia manifest themselves in debilitating and dull pain, especially at night, in the teeth and gums, and the pain can be bilateral.
Postherpetic neuralgia often coincides with damage to the trigeminal (Gasserian) ganglion. Its symptoms:
- sharp burning pain in the first (ophthalmic) zone;
- when there is an exacerbation in the area of pain, small blisters appear on the skin, after healing of which scars and spots remain;
- asymmetric swelling of the face (only half is swollen).
Neuralgia of smaller nerves of the T.N. is also possible:
- Nasociliary (symptoms: unilateral runny nose, conjunctivitis, keratitis, neurotonic pupillary reflex): the cause is most often associated with inflammation of the nasal paranasal sinuses.
- Lingual (burning pain in the larger anterior area of the tongue): causes - trauma, irritation of the tongue by the edges of a tooth or denture, infection, pathology of blood vessels and brain.
- Auriculotemporal (acute throbbing pain in the area of the femur, ear, temporomandibular joint): neuralgia is caused mainly by inflammation in the parotid gland.
Trigeminal neuritis
Inflammation of the nerve (neuritis) can begin due to injuries, infections, intoxications, tumors, abnormalities of the facial part and opening of the skull.
Neuritis is sometimes confused with neuralgia, although these are different pathologies: neuralgia is a symptom complex that occurs with various nerve lesions, and neuritis is an inflammatory disease: it is diagnosed only if the nerve is inflamed.
Very common factors in the development of neuritis:
- fracture of the base of the skull, affecting the exit of the trigeminal nerve from the opening of the skull and the superior pyramid of the temporal bone and leading to damage to the 3rd branch;
- unsuccessful removal of lower teeth - third molars;
- sinusitis and otitis.
Symptoms of neuritis: pain, paresthesia, sensory disturbances. Depending on the damage to individual branches, the signs are as follows:
- If the first branch of the trigeminal nerve is damaged: constant pain and loss of sensitivity in the frontal, ocular area and in the bridge of the nose;
- hypoesthesia of the cornea and conjunctiva;
- keratitis;
- decreased or absent superciliary and corneal reflexes.
In addition to inflammation of the main branches of the trigeminal nerve, neuritis is possible:
- Lower and upper alveolar nerve (pathologies are associated mainly with the removal of molars or unsuccessful treatment, when the filling protrudes beyond the surface of the tooth, as well as pulpitis, periodontitis, sinusitis, and sometimes diffuse osteomyelitis): manifested by pain, numbness in the gums, teeth, on the surface lower or upper lip and chin, mucous membranes of the cheek.
- Lingular or palatal nerve (most often caused by tooth extraction): pain, as well as paresthesia of the ⅔ anterior region of the tongue; dryness, burning, loss of sensitivity in half the palate.
- Buccal nerve - a violation of superficial sensitivity in the corner of the mouth and the mucous membrane of the cheek.
Damage to the Gasserian ganglion (ganglionitis)
Ganglionitis occurs for the same reasons as trigeminal neuritis.
Among infections, a special place among all etiological cases belongs to herpes: the gasserian ganglion of the trigeminal nerve is its favorite place. Other reasons why the Gasserian ganglion may be affected are cerebellopontine angle syndrome and intracranial tumors (neurinomas, sarcomas, meningiomas, etc.).
Symptoms of damage to the trigeminal ganglion:
- pain, loss of sensation,
- herpetic rash and ulcerations in the areas of all three branches;
- complications such as keratitis or conjunctivitis.
For gasserian node tumors, the signs are as follows:
- superficial paresthesia of the face;
- moderate pain in the areas of the first and second branches;
- pain, first in the eye or orbit, and later on the entire half of the face, nasal cavity, upper and lower jaw;
- weakness of the masticatory muscles;
- decreased corneal reflex.
As the tumor grows, symptoms of damage to other cranial nerves are added: first, oculomotor, abducens, trochlear, and then glossopharyngeal, hypoglossal, vagus and accessory.
Diagnosis of trigeminal nerve damage
The trigeminal nerve on the face is affected for many reasons, and therefore a thorough diagnosis must first be carried out:
- electroneuromyography;
- angiography;
- X-ray of the skull;
- if necessary, do an MRI or CT scan of the brain.
To exclude infectious inflammation of the nerve (and the trigeminal nerve, as is known, often becomes inflamed due to deep abscesses in the gums, poor condition of teeth, sinusitis, sinusitis, herpes), you must first undergo examination by a dentist and otolaryngologist.
Also, if the trigeminal nerve hurts, it is necessary to establish:
- in what form does the pathology occur (neuralgia, neuritis, damage to the Gasserian node, etc.);
- what are the affected areas on the face;
- which branches, roots and nuclei of the trigeminal nerve are affected.
How to treat the trigeminal nerve
The disease is so complex that it is impossible to give any general, “from the light” recommendations. Treatment should eliminate the cause that caused the damage to the trigeminal nerve: for example, with trauma, tumor, cerebellopontine tract syndrome, treatment regimens will be different. The treatment of neuralgia, neuritis, damage to the gasserian ganglion or nuclei also differs.
Treatment of trigeminal neuralgia
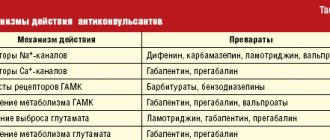
For neuralgia T.N. First of all, they prescribe:
- Antiepileptic drugs (carbamazepim, oscarbazepine, baclofen, gabapentin, phenytoin, clonazepam).
- Antispasmodics, vasodilators, antihistamines, sedatives, vitamins B12.
- Physiotherapy (Ural irradiation, UVT, electrophoresis, phonophoresis with the use of analgesics), acupuncture)
If treatment does not have an effect, intraosseous blockade or radiosurgery (irradiation of the affected area) is performed.
Treatment of trigeminal neuritis
- If the neuritis is traumatic, they usually limit themselves to conservative treatment with analgesic drug therapy, or resort to surgery.
- Infectious neuritis due to inflammation in the mouth or face must be treated by removing the inflammatory focus (anti-inflammatory drugs, antibiotics, opening an abscess, removing a diseased tooth, pumping out pus from the maxillary sinuses, etc.). To make the illness go away faster, auxiliary agents are prescribed to help remove toxins (glucose, drinking plenty of fluids, isotonic NaCl solution).
- For chronic sluggish neuritis, tonic drugs and agents (caffeine, strychnine, vaccine therapy) are prescribed.
- If severe pain does not go away, despite drug treatment, part of the nerve is excised and pieces of tissue (fascia, muscles) are placed between its segments.
Treatment of ganglionitis
- Eliminate the process that led to this: herpes, infections, tumors.
- Benign tumors are removed surgically, and malignant tumors are treated with radiation therapy.
How to treat damage to the trigeminal nerve nuclei
Damage to the nuclei of the spinal tract can occur due to circulatory diseases, cervical pathologies, hypertension, and atherosclerosis.
Treatment is very similar to therapy for cervical osteochondrosis:
- anesthesia;
- vasodilators (dibazole, nicotinic acid);
- means for improving cardiovascular activity (aminophylline);
- physiotherapy, massage of the cervical-collar area.
With specific lesions of the nuclei (tumors, tick-borne encephalitis, amyotrophic sclerosis, syringomyelia), central and peripheral muscle paresis occurs, and in these cases etiotropic treatment is carried out.
What to do with lesions of the trigeminal nerve
Consequences of the defeat of T.N. can be serious, and “grandmother’s recipes” are unacceptable here. It is necessary to treat the disease only in a neurological office.
- For neuralgia T.N. The doctor will prescribe anticonvulsants.
- If the neurologist diagnoses trigeminal neuritis, damage to the Gasserian ganglion, specific nuclear lesions (tumor, infectious, etc.), it will be necessary to continue treatment with other doctors (dentist, oncologist, therapist, dermatologist, etc.).
- Surgical treatment of trigeminal nerve lesions is performed by a neurosurgeon.
Prevention of trigeminal nerve diseases
It is very simple to catch a cold in the trigeminal nerve and create unfavorable conditions for it: for example, it is enough not to treat chronic sinusitis, not to pull out the remaining root in the gum for years, not to pay attention to constant trifling wounds on the lip (a sign of herpes). But it is very difficult to cure it. Sometimes no medicine can save you from severe pain, especially when the nuclei of the brain stem are damaged.
Take care of your trigeminal nerve:
- Do not sit in a draft, do not remove your hat ahead of time.
- Visit your dentist regularly.
- Avoid chronic purulent inflammatory processes in the nasopharynx and ears.
- Treat cervical osteochondrosis in a timely manner.
- Be examined immediately by a neurologist if you have pain in the temporal, frontal, nasal, or jaw areas of the face.
It is better to prevent damage to the trigeminal nerve than to treat it.