Causes of inflammatory damage to the trigeminal nerve
Factors contributing to inflammation of the trigeminal nerve are:
- surgical interventions on the jaw bones;
- fractures of the base of the skull, lower and upper jaws;
- tumors;
- complex tooth extraction;
- hypothermia;
- surgery on the maxillary sinus;
- improperly administered anesthesia;
- incorrectly performed dental prosthetics;
- metabolic disorders;
- the presence of foreign bodies that irritate the nerve trunk or injure nerve endings;
- bacterial or viral infection;
- various types of intoxication of the body;
- hypovitaminosis;
- weakening of the immune system.
Diagnostics
The diagnosis of trigeminal neuropathy is based primarily on the patient's medical history, symptoms, and physical and neurological examination findings. To make a diagnosis of NTN, it is necessary to exclude other diseases that may manifest as pain in the facial area. Some conditions that cause facial pain include: post-herpetic neuralgia, headaches, and temporomandibular joint disorders.
Due to the commonality of symptoms and the large number of conditions that can lead to facial pain, making a correct diagnosis is often difficult, but finding out the exact cause of the pain is very important, since treatment tactics for different types of pain may differ.
Most NTN patients will eventually need to undergo a magnetic resonance imaging (MRI) scan to rule out a tumor or multiple sclerosis as the cause of the pain. This test method can clearly show the compression of a nerve by a blood vessel. Special MRI techniques can reveal the presence and degree of compression of a nerve by a blood vessel.
The diagnosis of classic trigeminal neuropathy can also be confirmed by the positive effect of taking anticonvulsant medications for a short period of time. Diagnosis of T2 is more complex and difficult, but is usually confirmed by a positive response to low-dose tricyclic antidepressants in the same way as other neuropathic pain.
Symptoms of trigeminal neuritis
The maxillary trigeminal nerve consists of three types of nerve fibers:
- vegetative;
- motor;
- sensitive.
The symptomatic picture of neuritis may vary depending on which fibers were affected by the inflammatory process.
Damage to sensory fibers
In particular, with inflammation of the sensory fibers, the patient may complain of a tingling sensation, numbness, and weakened sensitivity in the area innervated by the trigeminal nerve.
Damage to motor fibers
When motor fibers are damaged, there is a partial or complete decrease in strength in the innervated muscles, their atrophy and deterioration of tendon reflexes.
Damage to vegetative fibers
When the vegetative fibers are inflamed, the patient experiences cyanosis and swelling of the skin, dryness and thinning of the skin, and the potential risk of developing a trophic ulcer increases.
Causes
Trigeminal neuropathy can be associated with a variety of conditions. Neuropathy can be caused by blood vessel compression on the trigeminal nerve as it exits the brainstem. This compression causes the protective covering around the nerve (myelin sheath) to wear or become damaged. Symptoms of trigeminal neuropathy can also occur in patients with multiple sclerosis, a disease that damages the myelin sheath of the trigeminal nerve. Rarely, symptoms of neuropathy may be due to nerve compression by a tumor or arteriovenous malformation. Damage to the trigeminal nerve (possibly as a result of oral surgery, stroke, or facial trauma) can also lead to neuropathic pain.
Pain due to inflammation
In addition, a disease such as inflammation or neuritis of the facial trigeminal nerve makes itself felt with attacks of pain of a very diverse nature:
- cutting,
- burning,
- pricking,
- tearing
- shooting, etc.
In this case, the area of pain does not always correspond to the area of innervation and can spread to the lower jaw, cheeks and chin.
Pain may be accompanied by:
- muscle spasms (facial, chewing),
- the appearance of nasal discharge,
- development of hypersalivation,
- increased lacrimation.
Lack of sensation in the tongue, lips and chin
With inflammatory damage to the trigeminal nerve, not only the entire nerve can be damaged, but also its individual branches. This is why numbness and pain can occur in various areas of the face. For example, when the lingual branch of the nerve is inflamed, patients complain of pain and sensitivity disturbances in the anterior part of the tongue, and when the mental branch is damaged, in the area of the lips and chin.
Pain when laughing, chewing, brushing teeth and shaving
Pain due to neuritis of the maxillary trigeminal nerve can intensify with touching, chewing, laughing and with changes in temperature. That is why patients, trying to prevent the recurrence of painful attacks, avoid excessive mobility and prolonged conversations, and refuse brushing their teeth and shaving.
Occipital neuralgia
The article was prepared by a neurologist, the chief physician of our clinic, Pavel Dmitrievich Kovzelev. In this article, in addition to a description of occipital neuralgia and the principles of treatment, you can watch a video with a clinical case from our patient, as well as a video of how an occipital nerve block is performed - one of the most effective methods of treating this pathology.
Anatomy of nerves.
The occipital nerves, 3 in number, are formed at the level of the 2-3 cervical vertebrae, then exit to the posterior surface of the spine and are located between the deep and superficial muscles of the neck.
At the level of the occipital bone, the nerves pierce the superficial muscles and exit under the skin, breaking up into small terminal branches that innervate the skin of the occipital region.
It's best to look at the picture.
Causes of neuralgia/neuropathy of the occipital nerve.
Why occipital neuralgia (also known as neuropathy) occurs is not completely clear.
The most popular hypothesis is that the nerve becomes trapped between the muscle and the fibrous tissue at the exit site and is pinched.
In people who have undergone surgery on the cervical/occipital region, people with Arnold-Chiari malformation, problems in the cervical spine, as well as those who have recently suffered a whiplash injury to the neck, NLDs are more common, which, in principle, fits into the “trap” hypothesis.
Symptoms of occipital neuralgia.
- The pain is severe, shooting, like electric shocks.
- Has a paroxysmal character: from several seconds to several minutes.
— The pain is localized in the back of the head, usually on one side and rarely on both sides.
- Between attacks, a dull, low-intensity pain may persist.
An attack can be provoked by touching certain points of the head, turning the head and any mechanical stimuli.
Sometimes patients note a decrease in sensitivity in these areas, and sometimes patients note dizziness and nausea.
IMPORTANT: Pain with occipital neuralgia can reach the fronto-ocular region through the connections of the occipital nerve with the trigeminal nerve at the level of the spinal cord.
The clinical picture may vary among patients. There are diagnostic criteria that I took from the 3rd International Classification of Headaches.
Let's look at them, but they are more important to me or your doctor.
- Unilateral or bilateral pain in the distribution of the greater, lesser and/or third occipital nerves and fulfillment of BD criteria
- Pain has at least two of the following three characteristics:
- repeated paroxysmal attacks lasting from several seconds to minutes
- heavy in intensity
- shooting, stabbing, or sharp pain
- Pain is associated with both of the following:
- dysesthesia and/or allodynia, manifested during painless stimulation of the scalp and/or hair (this is when normal touch is perceived as painful)
- one or both of the following: a) tenderness when pressing over the affected nerve branches
- b) trigger points at the origin of the greater occipital nerve or in the distribution of the C2 root.
- Pain is temporarily reduced by applying local anesthesia to the affected nerves. (i.e. when performing a blockade).
- Does not fit other diagnoses of the 3rd International Classification of Headaches.
Diagnosis of neuropathy of the occipital nerves. The diagnosis of NMN is made clinically (i.e., upon examination by a doctor), but for this it is necessary to exclude other causes. Taking into account the fact that many pathological processes in the posterior part of the brain and skull, as well as in the cervical spine, can produce similar pain in the occipital region, it is necessary to carry out:
- MRI of the brain
- MRI of the cervical spine, ultrasound examination of the vertebral arteries.
- In our clinic, ultrasound of the vessels of the head and neck is performed by a doctor with extensive experience, Irina Alekseevna Romadova, using an expert-level ultrasound device.
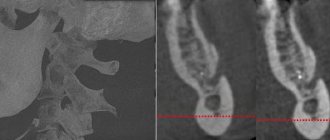
Treatment of neuralgia of the occipital nerves Treatment usually begins with a diagnostic blockade, which often gives a lasting positive result. I prefer to perform this block under ultrasound guidance for more precise and, more importantly, safe insertion. If necessary, the blockade can be repeated, but not more than once every three months. This is what it looks like schematically
This is how everything is visible with ultrasound navigation. I circled the nerve itself and its signature in red. It is very small, it literally looks like a dot. (Image clickable)
Drug therapy (standard drugs for neuropathic pain): gabapentin, tricyclic antidepressants, pregabalin, baclofen, carbamazepine.
of reflexology has proven itself well , which in this case is additional to stabilize and consolidate the effect.
If all of the above methods do not help, then you can: try botulinum toxin.
Also, one of my patients noted the effect of using Cefaly , a device for the treatment of migraines, which can be rented at our clinic to evaluate its effectiveness.
Neuralgia of the occipital nerves is an uncommon but extremely painful pathology. Sometimes people suffer for decades without a diagnosis or adequate treatment. At the same time, neuralgia has relatively clear diagnostic criteria and treatment approaches.
Kovzelev Pavel Dmitrievich
Chief physician, neurologist, vertebrologist
Treatment of neuritis of the maxillary trigeminal nerve
Therapy
The treatment program for trigeminal neuritis is drawn up taking into account the causes of the disease and its clinical signs. The main goals of treatment are:
- achieving a sensitizing effect;
- fight against bacterial and viral infection;
- increasing the body's immune forces;
- elimination of swelling of the nerve trunk;
- restoration of natural adaptive and compensatory reactions;
- normalization of the patency of nerve impulses.
Healing procedures
The set of procedures aimed at blocking the inflammatory process and eliminating all manifestations of neuritis includes:
- antibacterial therapy;
- antiviral therapy;
- elimination of factors contributing to the occurrence of intoxication;
- removal of tumor-like neoplasms or dissection of adhesions compressing the nerve;
- prescribing vitamin and mineral complexes to the patient;
- stimulation of nerves and muscles;
- acupuncture;
- physiotherapy (electrophoresis, phonophoresis, UHF, ultrasound, paraffin therapy).
People suffering from trigeminal neuritis are advised to regularly visit dental clinics and have their oral cavity sanitized.
The best treatment is prevention
Many patients are interested in whether it is possible to get a cold in their teeth if nothing bad has happened before under the same circumstances? It is possible if you have caries, but you did not cure it in time, and as a result, due to hypothermia, inflammation begins and the nerve hurts greatly. From this it becomes clear that it was caries that served as the root cause of subsequent inflammation, and if it had been cured, then a walk in the cold would not have brought any unpleasant surprises.
Pay closer attention to the health of your teeth, brush them thoroughly twice a day and do not forget to use dental floss and mouthwash. All these measures will help you avoid caries and visit the dentist less often, limiting yourself only to routine examinations.
It is important to take care of your health and choose the right clothes based on weather conditions. Severe hypothermia can cause serious illness.
Here are some simple tips to prevent colds in your teeth or facial nerve:
- Dress according to the weather; if it’s winter, don’t forget about warm clothes. Take care of gloves, a scarf and a warm hat, even if you leave the car for a short time. Sometimes a short stay in the cold wind is enough and a visit to the dentist becomes inevitable;
- Do not ignore even small manifestations of caries; a few unpleasant minutes in the dental chair are better than excruciating, incessant pain from a cold nerve. Do not skip preventive examinations with your doctor;
- A responsible attitude to oral hygiene can save you from many possible dental problems and save a lot of money on dental services;
- You can also get inflammation of the dental nerve in the summer when you are in a strong draft, near a working air conditioner or in a cold wind.
Do not forget that sometimes you need to have your teeth professionally cleaned to remove plaque and tartar, which can cause caries.
Why does pathology occur?
Doctors consider primary and secondary neuropathy. The primary cause is injuries, infectious diseases and hypothermia. The list of reasons that can cause a secondary type of illness is much more extensive. These include:
- disc displacement;
- neoplasms of any nature;
- osteochondrosis;
- protrusion;
- osteophytes;
- spasmodic muscles;
- curvature of the ridge;
- tunnel syndrome;
- intervertebral hernia;
- post-injection suppuration.
Drug therapy
Drug therapy involves the use of the following groups of drugs:
- Anticonvulsants (Lyrica, Neurontin, others). These drugs have shown good effectiveness against neuropathic pain. However, they have a number of side effects, the most common of which are decreased concentration, drowsiness and swelling of the legs;
- Antidepressants. Some antidepressants (Amitriptyline, Duloxetine) affect the production of special brain substances that are responsible for both depressive states and the perception of pain. Doctors often prescribe minimal doses of antidepressants in the complex treatment of postherpetic neuralgia. Their main side effects include: drowsiness, dry mouth, dizziness;
- In cases of severe pain and insufficient effectiveness of other drugs, patients may be prescribed narcotic analgesics.
How to avoid diseases associated with back hypothermia
Recommendations for the prevention of diseases of the spinal column include everything related to a healthy lifestyle. To successfully resist inflammatory diseases and degenerative processes in the joints, you need to lead an active lifestyle, but not overload. General physical training, gymnastics, and swimming are excellent for strengthening joints. When doing running and other sports that create impact loads on the spine, you need to take precautions: buy high-tech shoes designed for these purposes, do not run on hard surfaces, and always warm up your joints. It is also necessary to strengthen the immune system with proper nutrition and hardening, and avoid traumatic situations.
What does treatment of myositis include in our clinic?
Our specialists use the most effective methods in the treatment of myositis. Prescriptions such as:
- A course of anti-inflammatory drugs. Episodic use of medications is not enough; a systematic approach is required in their use.
- Anti-inflammatory and warming topical agents (ointments, gels, compresses).
- Massage using pain-relieving gels.
- Physiotherapeutic procedures - magnetic therapy, etc.
If abnormalities in the structure of the intervertebral discs are diagnosed, then treatment is prescribed to prevent the progression of osteochondrosis and recommendations are given on how to comply with preventive measures.
How to make a diagnosis
The disease is determined by a neurologist based on the results of motor tests that reveal the presence of the syndromes described above. But laboratory and instrumental studies are still necessary. As a rule, they are limited to x-rays in two planes. It may be necessary to obtain a more clear picture of the condition of the spine. In this case, a tomography will be prescribed. A radioisotope scan is done if a tumor is suspected.
When a person has inflammation of the sciatic nerve, treatment at home is not always acceptable, because the disease can manifest itself in such a serious form that the patient is prescribed bed rest in a hospital setting. Nerve-related illnesses must be taken seriously or you may lose your ability to move.
An immediate visit to a doctor is necessary in the following cases:
- severe numbness that prevents you from moving;
- increased body temperature;
- transfer of pain to other locations;
- incontinence of metabolic products;
- swelling in the lower part of the ridge.
Epidural administration of anesthetics and steroid hormones
Spinal epidural block involves the injection of drugs into the epidural space, which leads to loss of sensation in the area of impact. This means that this procedure involves introducing the active substance directly into the source of pain. Achieving a therapeutic effect in this case is possible due to the following factors:
- analgesic properties of the drug;
- the maximum possible concentration in the affected area;
- reflex action at all levels of the nervous system.