Home / Articles / Diagnosis and treatment of TMJ osteoarthritis
It has been noted that osteoarthritis of the TMJ can occur either with clinical symptoms or asymptomatically.
Symptoms of TMJ osteoarthritis include:
- pain in the joint area;
- limited mobility in the joint
- noise in the joint;
- change in jaw relationship (occlusion), etc.
Pain is not observed in all cases of osteoarthritis, but can be very severe and localized in the affected joint. The same applies to limited mobility of the lower jaw, as well as clicking and/or a characteristic crunching sound in the TMJ. The degree of disruption of the occlusal relationship may vary. It may also cause or result from symptoms of osteoarthritis.
In the first case, it is extremely important to identify and eliminate occlusal disorders, for example, loss of chewing teeth, premature occlusal contacts, etc. When occlusion is disrupted due to osteoarthritis, an open bite may be observed on the side of the affected joint or on the opposite side. If the height of occlusion is disrupted as a result of resorption of the head of the lower jaw, then an open bite is formed on the opposite side. Conversely, with swelling in the joint area, an open bite is formed on the affected side.
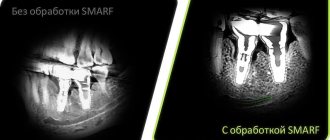
Imaging techniques play an important role in the diagnosis of TMJ osteoarthritis. Unfortunately, the relationship between clinical and radiological symptoms is currently not well understood. Sometimes even pronounced clinical symptoms are not accompanied by radiological changes. In contrast, obvious changes on the TMJ radiograph are often associated with the absence of clinical symptoms.
Traditional radiography can only convey a two-dimensional picture, but computed tomography (CT) allows one to obtain a spatial image of the anatomical structures and assess the density of the bone tissue of the head of the mandible. When performing magnetic resonance imaging (MRI), in addition, soft tissue abnormalities are detected, for example, displacement of the articular disc, joint swelling, as well as changes in the cancellous bone characteristic of TMJ osteoarthritis.
Before starting treatment for TMD, it is recommended to conduct an MRI, which will greatly contribute to correct diagnosis and treatment planning.
A thorough examination of the patient is of great importance in making a diagnosis. At the same time, we must remember that diagnostic information can not only help, but, unfortunately, also confuse. Each patient suffering from TMD is a puzzle that can only be solved if all the necessary data is obtained and interpreted correctly.
The examination of the patient includes determining his self-esteem and clinical examination.
- Patient self-esteem. The patient must fill out a questionnaire indicating personal and anamnestic data, complaints, condition at the time of examination, and medications taken. In addition, he describes in his own words the existing symptoms, warning signs of pain, dental history, general and mental state, habits, duration of pain, presence of noise in the TMJ, limitation of mouth opening and previous treatment.
- Clinical external and intraoral examination.
During an external examination, the doctor determines the maximum possible opening of the mouth without pain, and if pain occurs, the amplitude of various movements, deviation of the lower jaw, the exact location of pain with each movement of the lower jaw. During an intraoral examination, the specialist evaluates the features of occlusion (displacement of the dentition line, cross bite, open bite, etc.).
Treatment of TMJ osteoarthritis
The main task of the doctor in the treatment of this disease is to eliminate the symptoms and achieve a state of the joint in which it can adapt to the load acting on it. The treatment plan, as a rule, depends more on clinical symptoms than on X-ray data. It is recommended to resort to surgical intervention only after confirmation of the ineffectiveness of the main therapy. According to numerous studies, the prognosis after primary treatment is almost always satisfactory. Even despite the persistence of radiological signs of damage to the bone structures of the joint, clinically the condition often improves. After this, proper further management and observation of the patient is very important to stabilize the joint.
In general, treatment should be aimed at restoring protective mechanisms: sufficient blood supply, mobility in the joint, shock-absorbing properties, to ensure the ability of the TMJ to adapt. If necessary, therapy should be carried out aimed at reducing the load on the joint and increasing mobility in it, while eliminating pain and inflammation. Of course, patients who are at systemic risk should receive appropriate treatment under strict supervision.
Already at the stage of diagnosing osteoarthritis, one should try to identify the dominant risk factor. High load on the TMJ is caused by:
- clenching teeth,
- unfavorable changes in occlusion (loss of chewing teeth, premature occlusal contacts and bad habits).
Dental factors must be eliminated during treatment or minimized using occlusal trays and selective grinding. At the same time, it is recommended to switch the patient to soft food and help him get rid of bad habits.
To eliminate inflammation, medications (for example, nonsteroidal anti-inflammatory drugs) are used, which are prescribed orally, intramuscularly, or injected directly into the intraarticular space. Also, to reduce pain and inflammation, it is advisable to carry out physical therapy without stress on the TMJ. Exposure to heat and various compresses can effectively eliminate pain in order to continue to perform physiotherapeutic exercises aimed at strengthening the masticatory muscles, reducing joint contracture and maintaining a normal range of motion in the joint.
In general, treatment should be aimed at restoring mobility in the affected joint, which is an essential condition for complete rehabilitation.
Clinical picture
The development of osteoarthritis of the TMJ begins in patients with degeneration of intra-articular cartilage tissue. As the pathology becomes more complex, it spreads to bone tissue. Dystrophy leads to severe thinning of cartilage tissue and a decrease in its performance.
After complete destruction of cartilage, the disease spreads to hard tissues, which is due to their constant friction. As a rule, the destruction of soft and hard tissues is chronic. Pathological changes lead to increased mobility of the TMJ, and osteoarthritis becomes more pronounced.
General symptoms:
- uncharacteristic noises and crunching sounds;
- aching or dull pain, aggravated by jaw movements;
- decreased joint mobility;
- spread of pain to the peritemporal tissues;
- difficulty eating due to deformities of the affected joint;
- facial asymmetry associated with swelling and inflammation (observed in advanced cases).
Patients often do not realize the seriousness of the consequences, feeling minor discomfort in the TMJ area and consult a doctor with complaints of stiffness and severe pain. It is the lack of timely treatment that leads to the destruction of cartilage tissue.
Non-surgical treatment of TMD
Nonsurgical treatments for painful and dysfunctional TMD include patient education, joint stress reduction, medications, and physical therapy. Of course, the patient cannot control nighttime chewing activity, which is precisely the main source of excess load on the TMJ. To control this activity and reduce the load on the joint, various occlusal devices (for example, mouthguards) are used. According to research, they can reduce the load on the TMJ when clenching teeth in 82% of patients. During the daytime, the load on the joint is reduced by increasing the patient’s attention to his condition, switching to soft foods, and taking anti-inflammatory painkillers. A physical therapist can teach the patient specific exercises to increase mobility in the TMJ and relieve pain and stress on the joint.
Causes
Risk factors for developing osteoarthritis:
- people aged 40-60 years;
- injuries;
- bite defects;
- partial or complete loss of teeth;
- genetic predisposition;
- infectious processes of the ears.
It is difficult to determine the exact cause of the development of the disease, since the cause may be minor injuries that are left unattended.
Pathology can occur in adolescents with rapid growth, which is associated with anatomical features and accelerated growth of bone tissue against the background of underdevelopment of cartilage and muscles. Joint deformity can be diagnosed due to a lack of vitamins and an improper diet. If the body does not receive sufficient trace elements, this leads to deterioration of the cartilage.
Intense load on weakened temporomandibular muscles entails various microtraumas, the consequences of which are difficult to predict.
Surgical treatment of TMD
Surgical intervention in the treatment of TMD does not play a major, but very important role. Surgery is indicated for approximately 5% of patients suffering from TMD. Moreover, the range of surgical interventions is very wide. Despite the many supporters of each individual surgical method, there are currently no strict clinical data substantiating the indications for a specific operation in a specific clinical case. Therefore, when deciding on any surgical intervention, the doctor uses criteria to assess the stability of the patient's condition.
Symptoms, causes, classification
A separate problem associated with the development of pathology is the absence of pronounced symptoms in the early stages of development. Characteristic signs, such as extraneous sounds (clicks or crunches when chewing), a feeling of stiffness, a slight decrease in mobility, are not considered by patients as a reason to immediately consult a doctor. Usually the first visit is a consequence of the occurrence of pain, which manifests itself under mechanical stress and indicates the spread of the disease. In situations where the pain becomes aching or sharp, we can confidently speak about the formation of synovitis, which is the main factor in the increase in joint sensitivity.
Deforming arthrosis of the temporomandibular joint causes not only a decrease in the mobility of the lower jaw, but also changes in the structure of the articular head. A shift in the department towards the development of pathology is the cause of impaired facial symmetry, hearing problems, pain and tissue damage.
Factors that can cause the disease include:
- Presence of genetic prerequisites;
- Abnormal bite development;
- Long-term edentulousness of the lower jaw;
- Enamel wear and bruxism;
- Technical defects made during treatment;
- Operations performed and mechanical injuries received.
The current classification adopted in dentistry differentiates the general course of development of pathology into four stages:
- Early manifestation, expressed in narrowing of the joint space and loss of stability;
- Significant changes accompanied by characteristic symptoms;
- Late stage of development - characterized by TMJ dysfunction and cartilage destruction;
- An advanced stage at which arthrosis develops into the form of fibrous ankylosis.
A timely visit to a doctor for a comprehensive examination allows you to avoid serious consequences requiring surgical intervention.
Indications for surgery for osteoarthritis
The most common indication is severe pain and/or dysfunction of the TMJ of articular origin, which is aggravated by activity of the lower jaw. The more severe the pain and dysfunction, the better the prognosis for surgical intervention. The lack of effectiveness of arthrocentesis (sampling fluid from the joint) also became an indication for further surgical treatment. This low effectiveness of the procedure is explained by adhesions, which, in the absence of bone deformation, are not visible on an x-ray.
Treatment
Effective treatment of TMJ osteoarthritis requires an integrated approach.
In particular:
- taking medications;
- physiotherapeutic procedures to relieve symptoms.
Drug treatment
- The patient is prescribed non-steroidal drugs and anti-inflammatory drugs. In case of serious violations, the treatment protocol includes chondoprotectors that have a restorative effect.
- To relieve acute pain, potent analgesics are prescribed in various forms.
- In combination, the patient is recommended to install orthopedic structures (braces, mouth guards).
- It is recommended to limit your intake of solid foods.
Physiotherapeutic manipulations
- Ultrasound procedures.
- Laser therapy.
- Impact of dynamic currents.
- Electrophoresis.
- Microwave.
Surgery
If conservative methods do not bring the expected result, the patient is prescribed surgery. As a rule, surgical elimination of the problem is indicated only in complex cases when strong medications are ineffective. The operation is performed as an emergency if there is a purulent focus in the joint.
Instead of a conclusion
Statistics show that every third resident of the country has one or another joint pathology. Limitation of motor functions can lead to general complications, such as disruption of the metabolic and endocrine systems, hernias, limited mobility, etc. The earlier treatment is started, the higher the likelihood of recovery.
After successful treatment, a period of remission begins. The patient needs to remember that TMJ osteoarthritis is a chronic disease, so after the therapeutic course it is important to follow a diet and listen to the state of the body. Even minor infections can cause an exacerbation of the disease.
Diagnosis and treatment methods
The specificity of the diagnosis is due to the complex structure of the TMJ, as well as a wide list of factors that can act as a cause of the development of pathology. High-quality treatment is focused on eliminating not only the consequences, but also the original source, which helps avoid relapses. In addition to the standard visual inspection, the procedure includes:
- Instrumental diagnostics;
- Computer and radiographic scanning;
- Taking samples for laboratory tests.
The treatment plan is formed based on the identified indicators, and may not only be limited to conservative methods, but also include surgical intervention.
Prognosis and prevention
The outcome of the treatment course aimed at getting rid of the consequences of the development of arthrosis of the temporomandibular joint depends on the severity of the pathology, the timeliness of taking prophylactic and preventive measures, as well as the general condition of the oral cavity. Successful treatment requires the patient to strictly adhere to medical instructions regarding various aspects, including hygiene standards and adherence to a certain diet. In the event that the inflammatory process has led to the formation of exudate, surgery is a prerequisite to prevent general infection of the body.
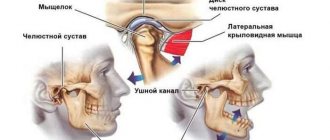
How does the TMJ function?
The TMJ is a unique joint in the human body. The peculiarity is that its two articular spaces are separated by an articular disc. In addition, only in the intra-articular space of the TMJ there is vascularized tissue, while in other joints of the body it is absent.
The TMJ is a trochlear-ball-and-socket synovial joint, so it can perform rotational and sliding movements. It is surrounded by a joint capsule, which is filled with synovial fluid. The head of the mandible is capable of moving in almost all directions within the mandibular fossa. In this case, there is no direct contact of the head of the lower jaw with the bone structure of the fossa due to the anatomical structure of the articular structures, including cartilage, fibrous disc and ligamentous apparatus. Because the TMJ articular disc is poorly supplied with blood and poorly innervated, joint pain is most often caused by inflammation or tissue damage.
Diagnostics
To cure the disease, a number of studies are necessary. Only an integrated approach to diagnosis will help make the correct diagnosis.
- First, the patient’s oral cavity is examined, an anamnesis is collected, complaints are identified, and the node is palpated.
- The muscles of the head and neck are examined.
- X-ray examinations are being carried out. Most often, TRH is prescribed in the lateral projection.
- A full neurological evaluation may be required.
- Artography, computed tomography, and MRI have a high degree of information content.
An x-ray shows defects in the affected area and degenerative bone pathologies. Areas of osteoporosis may appear. If the doctor is in doubt, it is recommended to undergo a morphological zonal analysis. According to indications, cartilage cells are studied, fatty degeneration is detected, EMG and orthopantomography are performed. The amplitude of movement must be assessed.
Prevention
It is better to prevent arthrosis of the jaw than to treat it. Preventive measures are based on regular sanitation of the oral cavity, purulent chronic foci, and treatment of acute infectious diseases. It is important to prevent injury to the node. For a favorable prognosis of the disease, rational prosthetics, timely normalization of bite defects, and treatment of concomitant pathologies are used.
Patients diagnosed with arthrosis of the TMJ are registered at the dispensary. Dentists provide the necessary therapeutic courses. The doctor may prescribe oral irrigation with antiseptic solutions. It is necessary to adjust the splints daily and change the intermaxillary traction. It is necessary to cure endocrine and somatic diseases that become provoking factors of pathology. Patients should lead a healthy lifestyle, protect themselves from stress, and eat a balanced and healthy diet.