Publication date: March 13, 2022.
Information on this page was updated on December 31, 2021.
TMJ dysfunction is a fairly common pathology these days, as it is largely caused by stress factors. Here it can be difficult to understand what is primary and what is secondary, because people with joint dysfunction usually come with bite pathology, pathology of the musculoskeletal system (curvature of the spine, neck). Therefore, joint treatment is a complex story. It happens that the primary pathology is a pathology of the joint, and sometimes it is the musculoskeletal system.
Comprehensive treatment of TMJ
When the doctor has determined the cause of the joint pathology, or causes, he determines the patient's readiness for a comprehensive treatment plan. In addition to the orthodontist, an osteopath or chiropractor may be involved, or even an orthopedist if more complex correction of the musculoskeletal system is required.
The patient should be aware that it is possible to straighten the jaw using a splint or splint, but this will not solve the problem of malocclusion. Orthodontic treatment will be required to correct the bite. If you have already had orthodontic treatment before, then it is more difficult to decide on repeated treatment.
Therefore, first the problem with the joint is solved using a splint or joint splint, then bite correction is carried out, and, if necessary, prosthetics. In parallel, work is underway with an osteopath to restore the muscular corset of the back and neck.
It happens that a patient refuses treatment with braces after the problem with the joint has been resolved. In this case, we warn him about the need to wear a joint splint constantly in order to avoid the recurrence of old problems with the TMJ. After all, a relapse can happen quite quickly due to stress.
First aid
A joint dislocation or subluxation that occurs for the first time can cause severe pain. Joint dysfunction can also cause pain of the same intensity. Regardless of the cause of the discomfort, you must do the following:
- provide rest to the joint: do not eat, talk as little as possible;
- take a pain reliever;
- Consult a doctor as soon as possible and undergo the necessary examination.
Experts categorically do not recommend heating a sore joint if the cause of the pain is unknown. In case of dysfunction, heat exposure can lead to some relief of the condition, but in case of dislocation, on the contrary, it will cause harm. Under the influence of heat, blood flow to the tissue increases, which contributes to the development of edema and makes reduction difficult. Thus, when trying to help yourself or a loved one, you can unknowingly cause serious harm.
What may be the symptoms of TMJ dysfunction?
- Tenderness or pain in the area of one or both TMJs at rest or when opening the mouth.
- Crunching, clicking, crepitation and other noises in the area of one or both TMJs when opening the mouth.
- History of TMJ injuries (previous), incl. dislocation, subluxation, chronic subluxation.
- Restrictions in the mobility of the TMJ, restrictions in opening the mouth.
- Excessive tone of the masticatory muscles, bruxism (“grinding” of teeth in sleep, at rest).
- Asymmetry of the chin, lips, lip frenulum, asymmetry of mouth opening, S-shaped opening.
- Suspicion of a forced position of the lower jaw.
Structure of the TMJ
The presence of one or more of the above symptoms may indicate TMJ dysfunction.
Traditional orthodontic treatment does not address TMJ dysfunction. During orthodontic treatment, the severity of dysfunction may not change, decrease or increase. At the moment, in the world scientific orthodontic literature there is no convincing data on the connection between orthodontic treatment and the condition of TMJ. Deterioration of the joint after treatment may have nothing to do with this treatment.
Note! Even in the absence of visible clinical manifestations of joint dysfunction, hidden disorders may occur that require special diagnostics to identify them.
If there is a forced incorrect position of the lower jaw, its position may change during the treatment process with changes and complication of the treatment plan (the need to remove individual teeth, increasing the duration of treatment). A reliably forced position cannot be diagnosed by traditional orthodontic methods; to verify its presence, as a rule, a special analysis is required (manual functional analysis, determination of the central relationship of the jaws), the use of a special articular splint for a period of several months, which, however, does not give 100 % guarantees.
To conduct a detailed articular diagnosis, explain the specifics of your case, and further manufacture an articular splint, you can make an appointment with an orthodontist who deals with the issue of TMJ dysfunction.
TMJ dysfunction is a chronic condition that can be compensated, but not cured (i.e., it is possible to eliminate symptoms, however, pathological changes in the joints, if they have already occurred, will most likely persist).
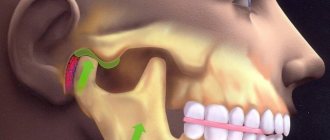
Structure and functions of the temporomandibular joint
The joint is formed by the head of the horn of the lower jaw and the articular surface (fossa) of the temporal bone. Between these bone formations there is a fibrous intra-articular disc, which is fused on all sides with the joint capsule. Ligaments and muscles help keep the joint in the correct position. They limit the range of motion in the joint. Attempting to exceed this functional limitation causes pain and prevents damage to the TMJ.
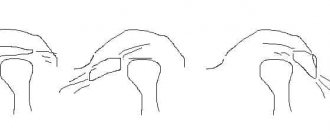
The main function of the joint is to ensure movement of the lower jaw in three directions:
- vertical: opening and closing the mouth;
- horizontal: lateral displacements of the lower jaw relative to the upper;
- sagittal: movement of the lower jaw back and forth relative to the upper.
The combination of movements of one jaw relative to the other allows us to chew, speak, and express emotions through facial expressions.
What happens if TMJ dysfunction is not treated?
If the dysfunction is not treated, the compensatory capabilities of the body may sooner or later be exhausted, the symptoms will worsen, the pathology will begin to progress, causing greater discomfort (sometimes for several years), thereby affecting the deterioration of the function of the dental system.
In order to try to prevent this and carry out treatment taking into account the individual characteristics of the structure and functioning of the temporomandibular joints, patients are usually offered the following approach.
Diagnostics
In order to make a diagnosis, the doctor conducts an examination according to the following scheme:
- Questioning the patient. Of interest to the specialist are complaints, conditions for the appearance of unpleasant symptoms, duration of the disease, previous treatment and its effectiveness.
- External examination and palpation. The gnathologist examines the patient’s face, paying attention to the area where the TMJ is located. By feeling the joints, you can get an idea of its structure and the state of its tissues.
- Dental examination. Anomalies of occlusion and the degree of their severity are identified.
- X-ray examination. The photographs show the bone formations that form the joint. By their relative position one can determine the presence of dislocations and subluxations, and by the thickness of the joint space one can judge the condition of the cartilaginous disc.
Treatment method for TMJ dysfunction
1. Diagnosis of TMJ dysfunction.
- When diagnosing a joint in the clinic, a series of measurements and tests are carried out, all sensations in the joint area are recorded (discomfort, clicks, pain, deviation of the jaw when opening and closing), the difference in sensations in the right and left joint.
- The orthodontist also takes impressions of the jaws and takes photographs of the face and intraoral photographs, and also performs three-dimensional computed tomography of the face (3D CT); if necessary, the doctor can give a referral for an additional study - magnetic resonance imaging of the TMJ (MRI).
- Often, the orthodontist, in addition to manual functional analysis, conducts a visual assessment of: posture, symmetry of the shoulder girdle, shoulder blades, hip bone structures, etc., performs the necessary tests and photographs. Based on the results, it is possible to schedule a consultation with an osteopath or chiropractor to jointly manage the patient. Related specialists (orthopedist, surgeon, periodontist) can also be involved in drawing up a treatment plan.
What exercises are prescribed to patients to normalize the work and relax the masticatory muscles?
Exercise No. 1
Draw a vertical line on the mirror with a marker, stand opposite so that the line divides your face into the right and left halves, place your fingers on the area of the articular heads, lift your tongue up and back, open and close your mouth along the line (it may not work right away), 2-3 times /day 30 repetitions. There is no need to open your mouth wide (a comfortable width), the main thing is symmetrically (so that the jaw does not “move” in any direction). If there is a click, open until it clicks.
Exercise No. 2 (cycle)
Do it whenever possible, for example, in front of the TV, at the computer, or in a traffic jam while driving. Open and close your mouth without closing your teeth for 30 seconds, then alternately reach your right and left cheeks with your tongue for 30 seconds. Open - close your mouth again, then for 30 seconds move your tongue in a circle inside the vestibule (behind the lips), first in one direction, then in the other direction (clockwise - counterclockwise), open again - close your mouth, etc.. For this a half-hour cycle, the teeth should not touch, the lips should be closed. If you want to close your mouth or swallow, place your tongue between your teeth. Repeat the cycle for 20-30 minutes 2-3 times/day
How dangerous is the disease?
TMJ arthrosis is silent and unnoticeable; people live with the disease for years without even knowing about the problem. But in vain.
Degrees of TMJ arthrosis
In the Russian Federation, the Kosinskaya classification of arthrosis has been adopted, which takes into account both symptoms and radiographic data. However, the TMJ is an exception to the rule: the joint “hangs”, held by muscles and ligaments, and does not experience weight loads comparable to other joints.
When at stage 1 according to Kosinskaya the joint space narrows, the pressure on the jaw simultaneously increases, which leads to problems with the teeth, but maintains the distance. The process is gradual, so this moment can be recorded on an MRI, but since there are no symptoms characteristic of the disease in the initial stage, it cannot be said unequivocally that this is stage 1 arthrosis. Only at stage 2, when symptoms appear (pain, facial asymmetry, etc.), and the patient finally consults a doctor, is a diagnosis made.
Stage 3 according to Kosinskaya: absence of joint space, sclerosis, necrosis, inability to open the mouth, chew and speak.
Damage to the TMJ by arthrosis
Possible complications
Arthrosis is not only a problem of the joint. Compensatory, in an effort to maintain chewing function, the body redistributes the load, which leads to tooth loss and rapid wear.
The previous diseases will be reflected in TMJ synovitis, and then the inflammatory process will affect the ear and nose (with decreased hearing, nasal congestion on one side), a headache will appear, which can radiate to the neck, back of the head and not stop.
The face will lose symmetry and become pasty (the skin appears loose, finely swollen, and grayish in color). Feeding is possible only through a tube; already at the second stage the ability to fully open the mouth is lost
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Exacerbations
Osteoarthritis is not arthritis; a chronic disease does not have periods of exacerbation. But this does not mean that the pain will be equally aching. The inflammatory process (cold, infection, virus) spreads to the joint with the development of synovitis. Swelling and pain appear, which can appear at any radial point (from the teeth to the back of the head). The source of inflammation expands, the oral cavity, ears, and breathing through the nose are at risk.
You need to understand that the brain is located nearby. And you shouldn’t wait for necrotic tissue to give rise to oncology.
Occlusive therapy for TMJ dysfunction
After diagnosis, the patient is scheduled for an appointment with the orthodontist to determine the central relationship of the jaws (“true” position of the lower jaw, the position in which your joint and chewing muscles will be most comfortable).
In order to more accurately establish and fix this position, an occlusal splint (splint) will be individually made for the patient from a special plastic, which is erased as it is worn. The splint must be worn constantly (sleeping, talking, eating in it if possible) - this is the meaning of occlusion therapy, which will help the joint and masticatory muscles rebuild into the most comfortable functional state.
Cleaning and caring for the splint is very simple - after eating (as well as while brushing your teeth), brush with a soft brush with toothpaste or soap.
Approach to treating the disease in our clinic
Our clinic is an example of integrative medicine: a synthesis of Eastern and Western approaches to treatment. In addition to neutralizing the causes of the disease and restoring the functionality of the HFNS, we restore the disturbed energy balance of the body and the integrity of its structure. Therefore, patients have the strength to cope with the disease and recover much faster than using only the usual medical protocol. All patients are different, so the appointment after the examination is individual.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
Installation of a brace system for a patient with TMJ dysfunction
Installation of a brace system on the upper jaw is carried out on average after 3 months of occlusion therapy. The splint is adjusted once every 1-2 weeks, or at the discretion of the doctor, until the main complaints from the TMJ are eliminated (in parallel with the alignment of the teeth in the upper jaw), then a brace system is installed on the lower jaw with partial reduction (grinding) of the interfering parts of the occlusal tires, or complete removal. Here the patient needs to be patient - the process may take several months.
At the same time, the new position of the lower jaw is monitored: repeated manual functional analysis, photometry, bite registration is possible, computed tomography of the face during treatment, continuation of orthodontic treatment with a brace system.
Upon completion of orthodontic treatment, final monitoring of the position of the lower jaw follows (manual functional analysis, photometry, bite registration, 3D CT scan of the face upon completion (after) treatment).
Joint splint
Joint splint with braces
Dissatisfaction with facial aesthetics, limitations in mouth opening
Before
Frontal photograph of the bite. Cross occlusion is noted on the right side. Absence of contacts of the premolar group on the left side. Tilt of the occlusal plane of the lower jaw to the left
Lateral photograph of the bite (right). Incorrect inclination of the frontal group of teeth in the upper jaw is noted. The lower jaw occupies a posterior (retracted) position
Lateral photograph of the bite (left). The incorrect inclination of the anterior group of teeth in the lower jaw is clearly expressed. Lack of closure of teeth in the lateral region
MRI slice of the right TMJ in the closed mouth position. The normal position of the articular disc is noted. Articular head of regular shape
MRI slice of the Left TMJ in the closed mouth position. There is a pronounced structural deformation of the articular head
MRI slice of the right TMJ in the open mouth position at 34mm. The normal position of the articular disc is noted
MRI slice of the left TMJ in the open mouth position 34mm. There is a limitation in the movement of this deformed joint. The articular disc is not in the correct position
After
Frontal photograph of the bite. Patient with a splint in the postoperative period
Lateral photograph of the bite (right). Ensures uniform contacts in the lateral sections
Lateral photograph of the bite (left). Ensures uniform contacts in the lateral sections
Specialists:
Nazaryan David Nazaretovich
Description:
The main complaints of the patient in this clinical case were dissatisfaction with facial aesthetics (the lower jaw is shifted to the right side) and limitations in mouth opening with pain in the area of the left TMJ. The entry MRI of the TMJ shows a pronounced deformation of the head of the left condyle with unreducible displacement of the articular disc.
The patient was recommended to undergo surgical treatment of the TMJ with preliminary production of Splint in preparation for the operation and subsequent use of this mouth guard in the postoperative period to support the joint structures during the healing period. The second stage of treatment for this patient will be orthodontic treatment in preparation for orthognathic surgery aimed at changing the position of the jaw bones and eliminating asymmetry.
Pain syndrome and restrictions in movements of the lower jaw
Before
Frontal photograph of the bite
Lateral photograph of the bite (right). Absence of tooth 4.5, absence of tooth 1.4 are noted with replacement of the defect with a removable partial apparatus
Lateral bite photograph (left)
MRI slice of the left TMJ. There is a structural change in the shape of the joint head. Anterior disc dislocation without reduction (without restoration)
After
Frontal photograph of occlusion after joint surgery
Lateral bite photograph (right)
Lateral photograph of the bite (left). There is a rise in the height of the bite on the operated side
MRI section of the left TMJ after surgical reduction of the articular disc. The correct position of the disc is noted
Frontal photograph of the bite in the mouthguard (Splint)
Lateral photograph of the bite in the mouth guard (Splint) (right view)
Lateral photograph of the bite in the mouthguard (Splint) (left view)
Specialists:
Nazaryan David Nazaretovich
Description:
A typical complaint for patients with TMJ problems is pain and restrictions in the movements of the lower jaw. Such complaints were also present in this clinical case. The entry MRI of the TMJ shows a pronounced structural change in the shape of the head of the left joint and an articular disc displaced forward without the ability to restore its position.
We carried out preliminary Splint therapy in preparation for joint surgery (we made a transparent rigid mouthguard for the lower dentition) and assessed the result over time with a series of control MRIs of the TMJ. Using the example of a section from one of these studies, one can clearly compare the picture before and after surgery. The patient also noted positive dynamics regarding pain symptoms already at the stage of wearing a mouth guard. In the postoperative period, pain was no longer observed. The range of movements of the lower jaw was restored. Of course, the closure of the teeth changed after placing the disc in the correct position. We will require orthodontic and orthopedic treatment to support the stability of the TMJ.