Ear pain is a fairly common symptom. Painful sensations in this case give the patient a lot of unpleasant moments, and it is very difficult to simply “endure” such pain. It is noteworthy that pain in the ear is not always associated with diseases of the hearing organ. Such painful sensations can also be caused by other organs that radiate, that is, “giving off,” to the ear. A condition in which the ear hurts, but there is no inflammation in it, is called otalgia.
Otalgia can be caused by many reasons:
Temporal arteritis
The disease is an inflammation of the vessels of the temporal artery.
If the inflammatory process spreads to the ear artery, the patient will also experience pain in the ears. This disease is typical for older women. It causes blurred vision, headaches, pain in the temples, and increased fatigue. Make an appointment right now! Call us by phone or use the feedback form
Sign up
Along the branches of the vagus nerve, pain can radiate to the ear from the esophagus, thyroid gland, and organs of the cardiovascular system.
If you have ear pain, you should definitely consult with an otolaryngologist, since this condition may signal the presence of serious diseases in the body. If the ear is healthy, no abnormalities have been identified, and the pain does not go away, it is necessary to diagnose the nose, larynx, pharynx and, if necessary, other organs to identify the cause of otalgia. Further treatment will depend on the diagnosis.
Primary treatment of pain in temporomandibular joint disorders
An important part of dental treatment is monitoring, diagnosing and treating pain, as well as relieving the underlying causes of pain. However, most dental patients with symptoms of unexplained pain often succumb to inappropriate diagnosis, resulting in misdiagnosis and ineffective treatment. As a result, the patient not only continues to suffer from chronic pain, but also becomes disillusioned with the dental treatment provided.
Pain in the maxillofacial area
By definition, pain in the maxillofacial area (orofacial pain) is associated with localization in the soft and hard tissues of the head, face and neck. With painful stimulation of these zones, through the structure of the trigeminal nerve, impulses reach the corresponding centers of the brain. In the brain, such signals are interpreted “as unpleasant sensory or emotional sensations that arise as a result of actual or potential tissue damage.” The density of tissue in the affected area greatly complicates the procedure for making a correct diagnosis. Quite often, patients describe the location of the toothache away from the actual site of the lesion. The phenomenon of referred pain is based on the interweaving of many sensitive nerve endings that are directed to the nucleus of the trigeminal nerve from the skin and deep tissues of the head and neck.
Toothache is one of the most common forms of pain in the maxillofacial area. The next most frequently reported pain is pain due to dysfunction of the temporomandibular joint (TMJ) and headaches. Often the patient may experience pain of several etiologies at once. The difficulty of diagnosing the main source of pain is also associated with the possible concomitant development of fibromyalgia, chronic fatigue syndrome, or other pathological conditions. In such cases, the best way to make a diagnosis is to use the principle of “peeling the onion” - verifying changes in symptoms one by one.
Temporomandibular joint
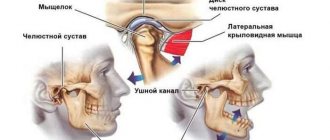
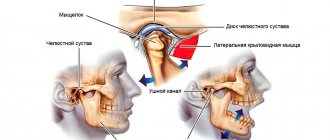
The temporomandibular joint (TMJ) is a complex joint that allows for both rotational and gliding movements of the mandible. Structurally, it consists of the condyle of the lower jaw, which in shape corresponds to the articular fossa of the temporal bone. The articular disc is made of dense fibrous cartilage and prevents direct contact between bone surfaces. The anterior part of the disc lacks blood vessels and nerve endings, while the posterior part, on the contrary, is characterized by an abundance of these structures. The joint is lubricated by a special synovial fluid contained in its composition. The movements of the TMJ are ensured by the masticatory muscles. Another main type of muscle that is not involved in the development of TMJ movements, but is responsible for demonstrating emotions, is the facial muscles. The complex of masticatory muscles includes the masticatory muscles themselves, the temporal muscles, the medial pterygoid muscles and the lateral pterygoid muscles.
Temporomandibular joint disorders
Temporomandibular joint disorders are a group of musculoskeletal and neuromuscular diseases that primarily negatively affect the function of the joint itself, the masticatory muscles, or the articular disc. The possibility of TMJ disorders should be taken into account when carrying out the differential diagnosis of facial pain, since TMJ dysfunctions are the most common cause of pain in the area of the dentofacial apparatus of non-odontogenic etiology. To make a correct diagnosis, you should carefully study the patient's medical history, taking into account the onset and duration of pain, as well as the effects of factors associated with relief or worsening of pain. Along with constant pain in the jaw projection, patients often complain of ear pain, headache and diffuse facial pain. In addition, they may complain of radiating pain or a feeling of stiffness in the face, jaw or neck, associated with restrictions in jaw movement, painful clicking or cracking sounds when closing or opening the mouth. Patients may also indicate changes in the nature of the relationship of teeth with each other. The above symptoms may be especially severe early in the morning, or worsen throughout the day. The threshold, localization, pain sensitivity and the nature of the description of pain sensations differ in different patients, and if we also take into account the complex mechanism of formation of the pain impulse, then one thing becomes obvious - diagnosis is an extremely important stage for the objectification of painful changes. History remains one of the key aspects of a comprehensive diagnosis, helping to detail aspects associated with the development of pain. In addition, during the collection of anamnesis while talking with the patient, the doctor can visually assess the nature of the movements of the lips and jaw, his facial expressions and posture, as well as his emotional status. Historically, occlusal disorders have been considered the primary cause of TMJ dysfunction. However, according to recent studies, these constitute only a small proportion of cases associated with painful joint dysfunction.
There are many classifications of TMJ dysfunctions. In other words, pain due to TMJ dysfunction can be arthrogenic and myogenic. Arthrogenic (joint and disc) dysfunction of the TMJ is usually caused by disc displacement or develops secondary to degenerative changes in the disc, ankylosis, dislocation, infection or neoplasia. Myogenic dysfunctions occur due to muscle hyperactivity or due to bruxism, hypermobility, or external stimuli. Myogenic joint dysfunctions can cause ischemia of the skeletal muscles of the face. Irreversible damage to myocytes develops after 3 hours of the ischemic state and in parallel with progressive microvascular disorders. All this only complements the pathological cycle of the mechanism of development of facial pain. Patients with myogenic dysfunction of the TMJ are characterized by the development of more complex pathological disorders and more severe pain compared to patients with arthrogenic dysfunctions. That is why the main principle of treating joint dysfunction is focused on treating and stopping the hyperactivity of the masticatory muscles.
Myofacial pain syndrome
According to the National Institute of Dental Research, the most common form of TMJ dysfunction is myofacial pain syndrome (MPS). With this chronic inflammatory disease, damage occurs not only to the muscles, but also to the fascia. The root causes of this disorder are repetitive movements, damage to muscle fibers and excessive tension in the ligaments and tendons. Patients themselves often complain of depression and fatigue, and even during a clinical examination, the doctor may notice some changes in their behavior. A differential sign of MPS is the presence of so-called trigger points, the activation of which provokes the development and irradiation of pain to different parts of the head and neck area. Trigger points (photos 1 - 4) are formed in the projection of excessive muscle contraction and dysfunction of one of the components of the biomechanical complex of the head and neck. This type of muscle spasm differs from physiological tension of the entire muscle: due to local excessive contraction, blood flow directly to the area of contraction is stopped, which consequently leads to the development of ischemia. The buildup of waste products and toxins sensitizes the trigger point, essentially causing it to send pain signals to the brain, causing even more contraction. Thus, the mechanism of trigger point formation includes a vicious circle of metabolic crisis. Clinically, trigger points can be identified by analyzing existing signs of the lesion, reproducing symptoms and performing palpation. Deep palpation almost always allows you to identify the main trigger zones. Often, when pressing on the trigger area, the patient may experience muscle twitching.
Photo 1. Trigger points of the masticatory muscle in the projection of the upper musculotendinous junction of the superficial layer and central trigger points of the superficial layer with corresponding patterns of pain spreading to the area of the lower jaw, teeth and gums.
Photo 2. Trigger points of the masseter muscle in the lower part of the superficial layer of tissue with corresponding patterns of pain spreading to the lower jaw and superciliary region.
Photo 3. Trigger points of the masseter muscle in the upper part of the deep tissue layer below the TMJ with corresponding patterns of pain spreading to the ear area.
Photo 4. Trigger points of the temporal muscle and projection of the spread of referred pain.
Masseter muscle
The masticatory muscle is the main muscle of the complex of the entire masticatory musculature. The lower jaw is the only movable part of the skull, the movements of which are ensured precisely by the masticatory muscle. It is located in the parotid region along the posterior edge of the jaw, easily visualized and palpated when the jaws are clenched.
The average person can bite with 150 pounds of force, but a bite force of more than 250 pounds is considered normal. This strength of the masticatory muscle is achieved due to specific biomechanical conditions: its lever arm is much shorter than in other muscles. Given the high activity of the masticatory muscle, its tension is visualized even when a person’s emotional state changes. When tension in the muscle continues for too long a period of time, this provokes the formation of those same trigger zones associated with myofacial pain. When trigger points are located in the projection of the masticatory muscle, the patient may experience pain in the eyes, on the surface of the face, in the structure of the jaw and teeth. According to Simons and colleagues, the trigger mechanism of the masseter muscle may even be responsible for the development of pain and itching in the structure of the ear, as well as the development of tinnitus - an unexplained ringing in the ears. Photos 1-3 show trigger points in the masseter muscle and general pain patterns (shown in red). It must be remembered that the facial nerve is motor and is responsible for the innervation of facial muscles. Therefore, when treating trigger points in the deep layers of the masticatory muscle, it is necessary to take into account the specific anatomy of the facial nerve in the projection of the zygomatic arch.
Temporalis muscle
The temporalis muscle is a large, thin, fan-shaped muscle located on the side of the skull above and in front of the ear. Although the masseter muscle is considered the most powerful, the temporalis muscle also plays an important role in the chewing process. It originates from the temporal bone of the skull and passes completely under the zygomatic arch (cheekbone), attaching to the lower jaw, thus assisting the masseter muscle in closing the jaw and retracting it. By placing your fingers just above your ear, squeezing and unclenching your jaw, you can feel the biomechanics of the temporal muscle. Photo 4 shows how strongly trigger points in the temporalis muscle are associated with the possibility of developing pain in the projection of the upper teeth, head, cheeks, eyes and ears. Often, when the nature of pain is incorrectly diagnosed, doctors resort to endodontic treatment, although such treatment may be completely non-odontogenic in nature.
Treatment with botulinum neurotoxin type A
Considering the basic principle of “do no harm,” the treatment of myofacial pain should be carried out through the implementation of non-invasive and reversible intervention methods. To relieve TMJ dysfunction, various palliative approaches and combinations thereof can be used, which include, but are not limited to, splint therapy, massage, physiotherapy, biofeedback, acupuncture, chiropractic, the use of ethyl chloride sprays and stretches, the use of antidepressants, narcotic and non-steroidal anti-inflammatory drugs. In addition, botulinum neurotoxin type A (BoNT-A), which is widely used in cosmetics (Botox, Dysport, Xeomin), and which has been previously approved by the US Food and Drug Administration (FDA) for the treatment of painful conditions potentially associated with disorders in the TMJ area (dystonia of the neck muscles, migraine, etc.). BoNT-A is an injectable pharmaceutical agent that is derived from the bacterium Clostridium botulinum. In small doses, this purified protein can be used to achieve selective skeletal muscle relaxation as it inhibits the release of acetylcholine at the neuromuscular junction. Consequently, due to this, the muscle will not be able to contract with the same intensity, since the amount of available neurotransmitter is markedly reduced. Constant, sometimes dysfunctional contraction of the masticatory muscles may be the main cause of the formation of trigger points in TMJ-associated disorders associated with myofacial pain syndrome. Treatment of TMJ dysfunctions with BoNT-A lasts for a month, allowing the effect to be achieved for 3-4 months. In this case, the physiological functions of chewing, speech, and swallowing remain unimpaired, but the intensity of pain noticeably decreases. Unlike systemic medications, botulinum toxin acts only locally, allowing relief of both active and latent trigger points. Immediately after the injection, the patient may report immediate pain relief as a “dry needling” effect develops. Although this approach cannot cure the cause of pain dysfunction, the effect of BoNT-A injections becomes more and more durable over time. On the other hand, in cases of resistance to other treatment methods, this approach may represent a successful alternative aimed at relieving existing pain. Dentists who are considering using BoNT-A in their practice as an approach for the management of pain associated with TMJ dysfunction may benefit from specialized training. During the latter, the doctor will be able to become familiar with the anatomy, physiology, pharmacological characteristics, as well as adverse reactions and potential complications associated with the use of botulinum toxin. The average price of a bottle with 100 units of active substance for a doctor is about $600. Before using BoNT-A, it is also necessary to take into account the specifics of local legislation regarding the performance of such manipulations.
Bruxism and Dental Sleep Medicine
Dental parafunction is a habit due to which certain organs of the oral cavity or the dentition do not function correctly. Moreover, it is not associated with the processes of drinking water or food, or with the function of speech. The most common parafunction remains bruxism, clenching and pathological abrasion. All of them can potentially be associated with TMJ dysfunctions. Physiological pressure applied to a tooth ranges from 20–80 psi (0.14 to 0.55 MPa), while with bruxism it can reach 300–3000 psi (2.07–0.55 MPa). 20.7 MPa). It is logical that under such conditions the load on the masticatory muscles increases significantly, and their overload, in turn, leads to the development of myofacial pain syndrome.
Masseter muscle hypertrophy
When examining patients with facial pain syndrome associated with TMJ dysfunction, the dentist often identifies the presence of trigger points in the projection of the masticatory muscle. In addition, such patients may experience such strong hypertrophy of this muscle that it provokes a distortion in the appearance of the face. Hypertrophy of this kind can be treated with the same BoNT-A used according to the injection protocol in cases of TMJ dysfunction. Botulinum toxin injections reduce the intensity of muscle contractions and allow the muscle to relax, eliminating the possibility of clenching the teeth with excessive force. But it should be remembered that the goal of such treatment is not only to relieve pain, but also to normalize the visual shape of the face, the distortion of which was caused by hypertrophy (photo 5-6).
Photo 5. View of a patient with hypertrophy of the masseter muscle before treatment.
Photo 6. View of the patient after treatment of masseter muscle hypertrophy using botulinum toxin.
Obstructive sleep apnea
Obstructive sleep apnea (OAE) occurs when repeated episodes of complete or partial blockage of the upper airway occur during sleep. During an episode of OAE, the diaphragm and chest muscles begin to work harder to open blocked airways and allow air into the lungs. Patients with OAE often experience TMJ dysfunction and signs of nocturnal bruxism. The American Academy of Dental Sleep Medicine classifies sleep bruxism as a movement disorder. To record data on bruxism and OAE, it is advisable to use a home monitoring device. Important indicators are the level of oxygenation, pulse, airway patency, the presence of snoring, the specifics of chest movements and body position during sleep. Once an apnea-hypopnea index score has been recorded in a patient with signs of bruxism, which could potentially indicate the presence of OAE, the dentist should contact the patient's physician for a more detailed diagnosis. If UAE is mild or moderate in severity, a customized intraoral device can be made for the patient, which will prevent tongue retraction and dislocation of the lower jaw, thus ensuring patency of the upper respiratory tract.
Headache
The connection between sleep bruxism, TMJ dysfunction and headaches is well established. Headaches provoke the development of significant discomfort, disruption of normal daily activities and possible further chronification of painful sensations. About 30% of patients with headache suffer from associated functional impairment and do not seek medical help. Patients may describe signs of headache during a history taking during a dental examination.
Tension headaches and migraines
Tension headache (TTH) is the most common form of primary headache, affecting most of the population at least once in their lives. Pain that develops from trigger points in the projection of the masticatory muscle can be either episodic or chronic, and clinically it is quite difficult to differentiate them from migraine pain. Therefore, it is necessary to remember that tension-type headache, as well as TMJ dysfunction, can be characterized by the presence of pain, which is a variant of migraine, although they themselves consist of a migraine-like component. Sometimes there is an overlap of symptoms of several pathologies, which can be interpreted both as diagnostic criteria for TMJ dysfunction and as diagnostic criteria of the International Headache Society. The relationship between TMJ dysfunction and headaches has been described in detail in the literature. Patients with an established diagnosis of tension-type headache or migraine, which can be triggered by temporalis muscle myalgia, may also present with symptoms characteristic of TMJ dysfunction.
On the other hand, patients who have undergone treatment for TMJ dysfunctions also experience a decrease in headache intensity levels. Recent evidence suggests that among patients with signs of vascular pain and migraines, there is an increased prevalence of TMJ dysfunction, since the latter can be interpreted as components of a complex of pain sensations with a specific localization. We should also not forget about the potential role of disorders of the facial nerve and facial muscles, which can also provoke the development of pain.
On October 15, 2010, the FDA approved BoNT-A injections for the prevention of headaches in adults with chronic migraine. The treatment protocol includes selective relaxation of hyperfunctional muscles of mastication or facial expression. The treatment approach is to use the lowest effective dose needed to relieve pain; The dosage of the drug depends on the individual response of each individual patient to the therapy. Again, dentists considering the use of BoNT-A injections are strongly advised to undertake appropriate practical training and follow the principles of existing legislation. However, the mechanism by which BoNT-A relieves migraine pain is not entirely clear. It is believed that botulinum toxin, by turning off muscle tension, reduces the load placed on them, and thus relieves pain associated with bruxism or clenching. However, the release of neuropeptides, especially calcitonin gene-related peptide (CGRP), is considered an integral component of the pathophysiological mechanism of migraine. It was found that BoNT-A not only affects the autonomic nervous system, but also directly reduces the amount of CGRP released by trigeminal neurons. Based on this, it can be assumed that BoNT-A relieves headaches through a direct effect on the central nervous system.
Cervicogenic headaches
Neck pain and neck muscle soreness are common symptoms of primary headaches. The diagnosis of cervicogenic headaches (CHH) refers to cases where the headache develops due to bony structures or soft tissues localized in the neck. The pathophysiology of this condition most likely involves disturbances in one or more muscular, neurogenic, osseous, articular, or vascular structures of the neck. Such lesions are often the result of head or neck trauma, but can develop in the absence of a history of trauma. Clinical signs of CDH may mimic those of primary headache, tension-type headache, and migraine. The diagnosis of CDH can only be made after a thorough history and physical examination. Diagnostic criteria include one or more of the following symptoms: moderate or severe pain in the occipital, frontal, temporal, orbital region of the head, neck and back; intermittent or chronic pain, usually deep and not throbbing; headache triggered by neck movements; or restriction of neck movements. Patients with CDH are usually characterized by a slight forward head tilt. Muscle trigger points are localized in the projection of the suboccipital, cervical and brachial muscles, and with physical or manual stimulation they can provoke the development of headaches in the head area. Studies show that 44.1% of patients with CDH have myofacial pain syndrome associated with TMJ dysfunctions. Moreover, when treating TMJ dysfunctions in patients with CDH, a more effective outcome of pain relief is noted, which allows patients to increase the range of motion of the neck as a whole. Like other pain symptoms associated with myofacial pain syndrome, they also respond well to BoNT-A injections.
conclusions
TMJ dysfunctions are characterized by a set of clinical manifestations that are often painful and lead to limitations in physical activity. However, they are self-limiting and usually respond to conservative treatment, such as BoNT-A injections. The basic principles of treatment are aimed at reducing pain and restoring the range of muscle motion, which helps reduce existing physical limitations and relieve pain of associated etiology. Treatment of TMJ dysfunctions also helps prevent the development of tooth damage and chipped restorations, pathological tooth mobility and periodontal tissue pathologies, which can be associated or caused by bruxism. During the treatment of dysfunctions, some patients manage to simultaneously get rid of night bruxism and relieve chronic pain in the neck and shoulders. If a patient is suspected of having signs of nocturnal bruxism, they should undergo home monitoring for potential obstructive sleep apnea. Despite the generalized nature of pain in the head and neck area, patients with chronic orofacial pain often initially seek help from a dentist. Therefore, the clinician must be theoretically and practically prepared to treat TMJ dysfunctions and relieve associated pain during their daily dental practice.
Authors: Lisa Germain, DDS, MScD Louis Malcmacher, DDS, MAGD
Functions of the TMJ
TMJ
or
temporomandibular joint
is a joint located above the ear that connects the temporal bone to the lower jaw and the lower jaw to the skull. The muscles that are attached to this joint are actively involved in speaking, facial expressions, chewing, and swallowing. Together, muscles, ligaments, cartilage and joints make up the apparatus, thanks to which we can generally open and close our mouth, move our jaw back and forth and left and right, and the load on this apparatus is significant - comparable to the load, for example, on the knee joint.
The temporomandibular joint is the only paired and symmetrically moving joint in the human body, and problems with its functioning lead to numerous unpleasant diseases. TMJ dysfunction—limited work and mobility of the jaw joint—occurs when the joint on the right and left sides of the skull does not move synchronously or evenly. For example, to open the mouth, the patient must first move the lower jaw from side to side, “until it clicks.” Or when you open your mouth, you feel pain in your jaw or temples.
This disease has many names: arthritis (arthrosis) of the TMJ, myofacial syndrome, myoarthropathy of the TMJ, chronic dislocation of the lower jaw, Costen's syndrome (named after the American doctor who first identified this disease). This pathology is difficult to diagnose and treat, and at the same time it can cause a wide variety of pain - from headaches to neck pain.
Statistical fact: from 30% to 70% of dental patients suffer from functional pathology of the temporomandibular joint. And these are not always older people, as one might expect. On the contrary, people of all ages, including children, suffer from TMJ pain and related pain.
TMJ dysfunction was first described by otolaryngologist (ENT doctor) Kosten in 1934. Kosten studied pain and noise in the ears and burning in the nose, which intensified during or after eating, and was the first to think of linking them with malfunction of the temporomandibular joint. Subsequently, his colleagues and other doctors who examined this problem expanded and supplemented the list of symptoms. Now this list is quite extensive, and often not all symptoms can be associated specifically with TMJ problems.
Treatment of the temporomandibular joint
Complex treatment of TMJ is possible only in dentistry, and is possible thanks to:
- surgery on the lower jaw;
- orthodontic treatment
(prescribing special trainers that will be worn at night and reduce pain by adjusting the load on the joint - the same trainers are recommended for bruxism) and bite correction with braces;
- orthopedic treatment
and
implantation
(insert a suitable prosthesis to restore the correct closure of the jaws).
Treatment is always prescribed individually, based on the results of an examination by an orthodontist, and is most often carried out comprehensively. It is dangerous to neglect TMJ diseases: this can lead to arthrosis, in which connective tissue grows in the joint cavity, which, in turn, threatens complete immobilization of the joint (ankylosis).
Severe pain and joint spasms can be relieved with compresses and painkillers; Stresses that provoke tension in the joint can be relieved with sedatives, but all these are half measures that do not treat the root cause of the pain.
Pain in the jaw joint: causes
- Defects in the dentition - lack of teeth, overestimation of fillings;
Pathological abrasion of teeth;- Broken bite
;
- Overload of the masticatory muscles (for example, if you chew on only one side for a long time);
- Inaccurate prosthetics, errors in orthodontic treatment;
- Other anomalies of the oral cavity and jaw structure;
- Bruxism, involuntary grinding of teeth.
- Birth trauma, trauma to the skull and jaw;
- Osteochondrosis and scoliosis of the spine;
- Severe constant stress
;
- An infection in the joint cavity that provokes inflammation of the TMJ.
Causes of jaw pain not related to dental disorders
Neuralgia
When the trigeminal nerve, which is responsible for the sensitivity of the face and oral cavity, is damaged, the pain is strong, sharp, reminiscent of the pain of pulpitis. Often patients with trigeminal neuralgia undergo unnecessary dental treatment with depulpation or tooth extraction, but the pain syndrome persists.
Sialolithiasis
Salivary stone disease is characterized by the formation of stones in the ducts of the large salivary glands. Since the salivary glands are located in the mouth, pain during their inflammation also affects other nearby organs of the oral cavity, in particular the jaw.
Sinusitis
When the mucous membrane of the maxillary cavity becomes inflamed, increasing swelling and accumulation of exudate cause pain spreading to the upper jaw area from the side of the affected sinus.
Otitis
Sometimes the symptoms of otitis media are similar to toothache. With inflammation of the middle ear, pain often radiates to the jaw. The pain is sharp, shooting, aggravated by chewing and swallowing.
Submandibular lymphadenopathy
Enlargement of the submandibular lymph nodes is observed in diseases of the tonsils, acute respiratory viral infections, stomatitis, and oncological tumors. Pain under the jaw is often accompanied by limited range of motion - it is difficult for the patient to bend and turn his head, or open his mouth wide.
Diseases of the cardiovascular system
Irradiation of pain into the lower jaw can be observed during an attack of angina and myocardial infarction. A characteristic symptom of coronary heart disease is burning, pressing pain behind the sternum. But with an atypical course of a heart attack, retrosternal pain may be completely absent, only reflected pain comes to the fore: in the left arm, in the neck, in the face, in the jaw.
What to do if your ear and right side of your head hurt
Treatment is selected individually, depending on the nature and intensity of the pain syndrome, the exact diagnosis, the patient’s age and other factors. The scheme may include several stages that are combined with each other.
- Drug treatment: in the first stages, non-steroidal anti-inflammatory drugs (Ibuprofen, Meloxicam and others) are prescribed. They affect inflammatory processes of any origin, not complicated by bacterial infection. To relieve episodic pain, analgesics are used - painkillers (Analgin).
- Antibacterial therapy: antibiotics are indicated for purulent inflammation, as well as to prevent its development. These drugs are often prescribed for otitis media.
- Muscle relaxants are used in addition to the main treatment regimen (Mydocalm). These drugs help relax muscles and relieve vascular spasms.
- Nootropics are a group of drugs to improve blood supply to the brain (Glycine, Phenibut). The decision about their effectiveness for various disorders is made by the attending physician.
- Surgical treatment - surgery is prescribed only if conservative methods do not bring results. It may be necessary for purulent otitis, some pathologies of the cervical spine, and the consequences of injuries.
The Clinical Brain Institute specializes in the diagnosis and treatment of headaches. The center is equipped with the necessary technical facilities for a full examination of patients. Treatment is carried out both on an outpatient basis and in a hospital, with constant supervision by competent specialists. Doctors recommend not to endure pain in the ear and head, especially if it is intense or occurs frequently - timely diagnosis and initiation of treatment will prevent dangerous consequences.
Diagnostics
When there is pain in the jaw, the patient first seeks advice from a dentist.
A dental examination includes the following steps.
- Clarifying patient complaints and collecting anamnesis. Since the main complaint is pain in the jaw, the time of its appearance (at night, during the day), the nature of the pain (sharp, dull, pulsating, aching), and duration (constant, paroxysmal) are specified.
- Examination of the oral cavity with assessment of the condition of the mucous membrane, tongue, gums, determination of the type of bite.
- Examination of the surfaces of all teeth using a probe and mirrors, identifying the integrity of the dentition, detecting defects in the hard tissues of the teeth.
- The percussion method is used to determine caries complications.
- Thermodiagnostics is used to identify pain reactions.