If a person feels pain in the jaw, radiating to the ear and temple, we may be talking about arthritis of the mandibular joint. The pathology is not just painful, but also dangerous. If not diagnosed in a timely manner, it can lead to severe complications, including paralysis of the facial nerves. Therefore, the first thing to do when such symptoms appear is to consult a specialist. In 10-18% of cases, diagnosis and treatment of TMJ arthritis is the responsibility of dentists and occurs in people from 25 to 45 years old.
Causes of temporomandibular joint arthritis
Arthritis does not show pronounced symptoms immediately; its development can be asymptomatic for a long time or with minor pain. Out of habit, a person reacts to pain by taking painkillers, which only makes the situation worse. Anesthetics relieve symptoms, but do not remove the cause. The disease “takes over” more and more healthy tissue and, as a result, instead of treatment, the patient receives disability. Let's figure out why TMJ arthritis can develop.
- 1. Mechanical injury. Impact, the habit of clenching teeth tightly, and active chewing of hard food can lead to damage to one or more components of the joint. Articular tissues respond to damage with pain and dilation of blood vessels. Simply put, blood enters from the vessels directly into the tissue, causing swelling, inflammation, and, if treatment is delayed, suppuration.
- 2. Infection. The inflammatory process develops as a result of pathogenic microorganisms entering the joint through the blood or through direct and contact routes. The direct route of infection involves inflammation of the TMJ as a result of an open wound (knife or gunshot wound). If microorganisms have penetrated into the cartilage from infected muscle or bone tissues, then the pathology of transmission is called contact. All diseases of the oral cavity (as well as ear, nose and throat) can lead to arthritis of the temporomandibular joint through the hematogenous route, through the blood.
- 3. Systemic inflammation. Some pathologies of an inflammatory nature (herpes, hepatitis, mycoplasmosis, chlamydia, lupus), if not treated in a timely manner, affect connective tissue throughout the body.
Features of diagnostic measures for TMJ dysfunction
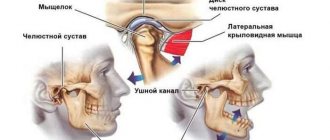
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
Symptoms of TMJ arthritis
Depending on the cause of the disease and the nature of the inflammation, arthritis manifests itself with the following symptoms:
- sharp pain when moving the jaw. Increases in opening/closing of the mouth, strongly radiates to the temple, back of the head, tongue;
- when you try to open your mouth wider, the jaw moves to the side;
- inability to close teeth tightly;
- hearing loss, dizziness;
- crunching when moving the jaw.
If at least 2 signs are detected, we recommend that you do not wait for the consequences, but contact the dentist. Correct diagnosis ensures the necessary treatment and recovery in a short time. In the later stages, the dentist will not help. And treatment will cost much more.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Treatment tactics for arthrosis of the mandibular joint
Ideally, starting treatment for TMJ arthrosis is optimal at stages 1 or 2. First of all, it is important to exclude risk factors - excessive mechanical stress, prolonged opening of the mouth, for example at a dentist appointment, etc. Therapy should be continuous and comprehensive - individual orthopedic measures or diet are not enough.
- Diet. To reduce the mechanical load, the patient is recommended to switch to soft foods, and during an exacerbation - to purees, juices, cereals and fermented milk products.
- Daily routine and lifestyle. It is very important to get enough sleep and limit stress, since any stress causes you to reflexively clench your teeth, which can aggravate the situation.
- Dentist consultation. Provoking factors include dental defects, missing teeth, and malocclusion. These problems are easily solved today, and patients with jaw arthrosis are primarily referred to the dentist and orthodontist.
A dentist and an orthopedist always take part in the treatment of jaw arthrosis.
How is arthritis of the lower jaw joint treated?
If pain and stiffness symptoms occur, it is necessary to ensure the TMJ rests. Move your jaw less, take only liquid food, and do not clench your teeth tightly. Visiting the dentist is a must. Only a qualified specialist will be able to tell why the joint is inflamed and prescribe the optimal treatment. Diagnosis consists of blood tests and x-rays. Depending on the situation, we recommend:
- cold compresses;
- drug treatment (broad-spectrum antibiotics, painkillers);
- physiotherapy.
If conservative treatment is ineffective, surgery will be prescribed. Traditional methods of treatment are not only ineffective for arthritis of the temporomandibular joint, they are often dangerous. Decoctions, compresses and ointments according to grandmother's recipes can relieve pain and swelling, but they will not remove the cause of the disease; moreover, some of them can inflame the joint even more. The consequences are impossible to predict, especially with the hematogenous method of infection of the joint. 20% of patients who treated themselves develop joint paralysis.
Symptoms of arthrosis of the jaw joint and diagnosis of the disease
The first signs of the disease usually appear between the ages of 32 and 50 years. If the patient is well informed about the symptoms and treatment of arthrosis of the jaw joint, the disease can be recognized in its infancy.
Symptoms of arthrosis of the jaw - a reminder for self-diagnosis!
You should be alert to the following changes:
- regular clicking in the joint when moving the lower jaw - the crunching seems to “send to the head”;
- limited mobility - for example, when yawning, the mouth does not open as wide as before;
- deterioration of hearing - sounds become muffled, the ears are often blocked, a characteristic noise is heard (as if a seashell was applied to the ear), deafness develops over time;
- blurred vision, which is usually accompanied by pain in the eye from the affected joint;
- pressing and bursting headaches, especially in the temporal, parotid-masticatory region;
- frequent cramps, usually painful;
- nasal congestion;
- dizziness and other problems with the vestibular system;
- abnormalities in the functioning of the salivary glands (usually dry mouth);
- facial asymmetry that has not been observed before - caused by misalignment of the jaw, the formation of bone spurs or swelling of the joint;
- fatigue when chewing food, discomfort when chewing hard and tough foods;
- morning stiffness in the jaw joint;
- decreased facial expression and difficulty swallowing food;
- increasing pain in the joint;
- toothache and tooth wear;
- numbness of the skin or mucous membranes near the affected joint;
- a feeling of “jumps” in the joint - sometimes even noticeable from the outside.
Acute piercing pain with arthrosis of the jaw joint can radiate to the ear, temple or back teeth on the affected side. However, more often patients suffer from a dull, aching pain in the jaw. In old age, pain due to arthrosis of the lower jaw may be absent, giving way to aches (including when the weather changes), heaviness and discomfort in the joint.
If, shortly before the onset of symptoms of jaw arthrosis, you have suffered from arthritis of the jaw joint, an acute infection, an exacerbation of chronic otitis, facial trauma or tooth loss, consult a doctor immediately.
Medical diagnosis of arthrosis of the jaw
When diagnosing arthrosis of the lower jaw, the doctor uses X-rays to determine the type of changes in the joint - sclerotic (replacement of normal bone tissue with abnormal one) or deformational (associated with bone abrasion or the growth of bone growths - osteophytes).
Also, x-ray examination allows us to determine the stage of arthrosis of the facial jaw:
1st - onset of the disease without significant changes in the bone;
2nd - destruction of the articular head with noticeable signs of the recovery process;
3rd - pronounced growth of bone tissue, which prevents movement in the joint;
4th - complete immobility of the jaw due to the fact that the elements of the joint are not consistent with each other.
In addition to x-rays of the jaws, the doctor may prescribe a general blood and urine test, a biochemical blood test, zonography of the affected joint, or diagnostic arthroscopy.
Between the onset of the disease and its final stage, 20-30 years may pass, or maybe 6-12 months. Do not ignore the first symptoms of arthrosis of the jaw joint. Arthrosis of the jaw is completely reversible only at the 1st stage!
Orofacial pain is widespread in the population. Patients with facial pain see doctors from many specialties, including dentists, oral surgeons, neurologists, internists, and otolaryngologists. Diagnosing facial pain can be very challenging for a doctor.
Facial pain can be caused by a number of reasons. In the International Classification of Headache and Facial Pain, 3rd revision (ICHD-3 beta), pain syndromes in the facial area are given in Chapter 11 “Head or facial pain associated with pathology of the bones of the skull, neck, eyes, ears, nose, sinuses, teeth , oral cavity or other structures of the face and neck” and in Chapter 13 “Painful cranial neuropathies and other facial pain” [1]. It should be noted that in Chapter 11, almost all sections use the term “headache”; only one section mentions facial pain per se (11.8). In Chapter 13, pain syndromes are referred to as “neuralgia” or “neuropathy.”
Most of the syndromes listed in the ICHD are not often encountered in the practice of a neurologist. One of the common mistakes in interpreting the cause of facial pain is overdiagnosis of trigeminal neuralgia (TN) followed by long-term and ineffective treatment with carbamazepine. At the same time, it has been shown that TN is a relatively rare cause of facial pain [2].
This article will focus on temporomandibular joint dysfunction (TMD). Today, TMD is considered the most common cause of chronic facial pain not associated with dental diseases [3]. Facial pain associated with pathology in the temporomandibular joint (TMJ) occurs in 19–26% of the adult population, and in women it is observed 1.5 times more often than in men [4, 5].
Clinical picture
Patients with TMD may experience pain in the face, upper and lower jaw, neck and shoulders, and in and around the ear. The pain may be constant or appear when chewing, talking, or opening the mouth. Often the pain is also accompanied by a feeling of facial fatigue and swelling.
In addition to facial pain, patients may experience headaches, neck pain, ear pain, toothache, burning and stabbing pain in the face, as well as shooting and puncture sensations. In addition to pain, there are also more rare and therefore even more difficult to diagnose symptoms: noise, ringing or congestion in the ears, non-systemic dizziness and even itching or tingling in the head and neck area. Pain may develop gradually, but many patients report an abrupt onset of pain and associated symptoms.
The occurrence of difficulties with chewing, the inability to open the mouth wide, the appearance of crunching/clicking when opening or closing the mouth, as well as blocking of the lower jaw - all this indicates damage to the TMJ itself and facilitates diagnosis.
Diagnosis and differential diagnosis
Previously, TMD was considered exclusively as a pathology of the TMJ and as a consequence of subluxation of the lower jaw, arthritis, arthrosis or trauma to the TMJ, as well as occlusal disorders [6, 7]. However, in 2014, the Diagnostic Criteria for TMD for Use in Clinical Practice and Research (DC/TMD), developed by the International RDC/TMD Consortium Network and Orofacial Pain Special, was adopted Interest Group). In accordance with these criteria, TMD is divided into two groups: pain and intra-articular pathology; their combination is also possible [8].
A large number of patients with TMD experience a painful form, that is, pain in the area of the masticatory muscles, while no pathology of the joint itself is detected. The literature describes facial pain associated with myofascial dysfunction of the facial muscles [7, 9]. The authors indicate that when palpating the muscles on the side of pain, attention was paid to the dense consistency and tension of the muscles, especially the masticatory and facial muscles, as well as severe pain and myofascial trigger points. When palpating the masticatory muscle, pain spreads to the upper and lower jaws, upper and lower molars, ear, frontal region, TMJ, and neck. When palpating the temporal muscle, pain radiates to the corresponding half of the head, forehead, upper teeth, and orbit. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form [10], most patients can and should receive effective care from a neurologist. Thus, facial pain in a patient is most often caused by hypertonicity and myofascial pain syndrome in the masticatory muscles without pathological changes in the structures of the joint itself.
When a patient presents with facial pain, the neurologist needs to conduct a proper examination (palpation) in order to diagnose and optimally treat such patients. This will avoid unnecessary referral of patients to dentists and ENT doctors and unnecessary and often painful examinations.
New criteria for the correct diagnosis of TMD are presented in the table.
Diagnostic criteria for TMD DC/TMD for use in clinical practice and research (adapted from [8])
Thus, according to the diagnostic criteria for TMD for clinical use, pain disorders are not associated with the pathology of the TMJ itself and can be represented by myalgia, arthralgia and headache associated with TMD. The given criteria are based on anamnesis and clinical examination (palpation of the temporal and masticatory muscles) and do not require mandatory imaging studies. In myalgia, pain may be felt in the jaw, temple, ear, or anterior to the ear and usually changes with jaw movement, chewing, or parafunctional activities. This means that pain in the face, ear, anteriorly and near the ear, as well as noise in the ear may be symptoms of TMD and do not indicate the presence of an ENT pathology.
In the case of local myalgia, the pain felt by the patient is reproduced by palpation of the temporal and masticatory muscles within their palpable area. In myofascial pain syndrome, pain extends beyond the palpable area within or beyond the palpable muscle (myofascial pain syndrome with referred pain).
It should be noted that for a complete diagnosis, it is necessary to follow the correct muscle palpation protocol: 3 points in the temporal muscle (anterior, middle and posterior sections) and 3 points in the area of the masseter muscle (the beginning of the muscle, its body and its insertion) [11]. Palpation is carried out with one or two fingers on each side separately or on both sides at once (depending on the patient’s convenience), the duration of pressing to determine myalgia should be at least 2 s, if it is necessary to determine the subtype of myalgia - at least 5 s. In practice, it is also possible to palpate the masticatory muscle by pressing it with the examiner’s thumb in the patient’s oral cavity and with the rest of the fingers outside.
To determine the presence of arthralgia, it is necessary to confirm that the pain felt by the patient in the face is localized in the TMJ area and is reproduced with provocative tests: palpation in the area or around the condylar process of the mandible or with maximum active or passive opening of the mouth, lateral movement or protrusion of the mandible.
When pain is localized in the parotid region anterior to the pinna, identifying the specific structure involved may be challenging for the clinician. In this case, it is necessary to determine whether the pain is localized in the area of the condylar process of the mandible (arthralgia) or the masticatory muscle. In the latter case, one of the types of myalgia will be diagnosed. To determine the location of the condylar process of the jaw and confirm the source of the pain felt by the patient, it is necessary to palpate the preauricular area with the mouth closed. In case of difficulty, palpation should be performed when opening the mouth or moving the lower jaw forward (Fig. 1).
Rice. 1. Palpation to determine the location of the condylar process of the mandible. a - with comfortable closing of the mouth; b - with protrusion of the lower jaw.
To find the points of palpation of the masticatory muscle, it is necessary to ask the patient to clench and then unclench his teeth. In this case, determining the boundaries of the palpated muscle is greatly simplified (Fig. 2).
Rice. 2. Palpation of the masticatory muscle to determine the shape of the TMD. a — the origin of the muscle; b - muscle body; c — muscle attachment zone.
Palpation of the temporal muscle is much simpler. It is necessary to palpate at least 3 points in the anterior, middle and posterior portions of the muscle (Fig. 3). If there is difficulty in finding the boundaries of the temporal muscle, the patient should be asked to clench his teeth.
Rice. 3. Palpation of the temporal muscle to determine the shape of the TMD. a - anterior portion of the muscle; b - middle portion of muscle; c - posterior portion of the muscle.
Another type of painful form of TMD is TMD-related headache. In ICHD-3, beta headache associated with TMD is classified as a secondary cephalalgia and is described as “tension caused by a disorder involving structures in the region of the TMJ” [1]. The first two points are nonspecific criteria confirming the secondary nature of the pain; only point 3 contains characteristics specific to TMD: headache is provoked or aggravated by active movements of the jaw, passive movements in the usual range of jaw mobility and/or during provocative tests with temporomandibular structures, for example, by applying pressure to the TMJ and surrounding masticatory muscles. However, the comments to the diagnostic criteria contain a recommendation from the International Headache Society to use newer and more accurate criteria developed by the International Network Consortium RDC/TMD and the Orofacial Pain Study Group to fully diagnose and clarify the causes of pain associated with TMD.
Differential diagnosis of headache associated with TMD includes other forms of primary and secondary cephalgia. When carrying out differential diagnosis, it is necessary to rely on the known diagnostic criteria for these cephalgia. In the case of strictly unilateral headache, it is necessary to exclude migraine and cervicogenic headache. Patients with migraine are characterized by provocateurs of a painful attack that are not typical for TMD, migraine symptoms accompanying the attack (nausea, vomiting, phono- and photophobia), and often a hereditary history of G.B. To confirm the diagnosis of cervicogenic headache, rotation tests and diagnostic blockades of cervical structures are used [1]. In the case of bilateral localization of pain, it may be difficult to differentiate from tension headache combined with tension in the pericranial muscles. In this case, inspection and palpation shown in Fig. 1-3 are of key importance for diagnosis.
Somewhat less common in neurologist practice are intra-articular forms of TMD. It should be noted that in many cases, the identified intra-articular pathology is combined with the painful form of TMD, and is not isolated.
When there is damage to the TMJ itself, there are several forms of TMD. With various forms of displacement of the intra-articular disc with reduction, different intracapsular sounds are noted during palpation of the joint and movements of the lower jaw: crunching, crackling, clicking. Disc displacement without reduction is usually caused by spasm of the lateral pterygoid muscle [12]. When the disc is displaced without reduction, there is a pronounced limitation in mouth opening and impaired ability to eat. In the case of degenerative disc pathology, a rougher (grinding-like) and longer sound can be noted - crepitus, caused by friction of the damaged intra-articular disc. Locking of the TMJ with the mouth open and the inability to close the mouth without an auxiliary maneuver indicate subluxation of the mandible.
The examination rules for diagnosing the intra-articular form of TMD are shown in Fig. 4. To confirm the diagnosis of various intra-articular forms of TMD, an MRI examination of the joint is necessary.
Rice. 4. Palpation aimed at detecting sounds in the TMJ. a - when opening/closing the mouth; b - lateral movement of the jaw to the right; c - lateral movement of the jaw to the left; d - protrusion of the lower jaw. Palpation is carried out sequentially on each side.
Etiology and pathogenesis of TMD
The etiology of TMD is multifaceted and is a combination of psychological, postural, orthopedic, genetic, biopsychosocial and occlusal factors that disrupt the functional balance in the structures of the TMJ itself and the muscles surrounding it [6, 13, 14].
The view on the pathophysiology of TMD cannot be considered fully formed. In 1934, James Costen first gave a systematic description of this group of diseases, citing malocclusion as the main cause. For many years, it was believed that the cause of myogenic and joint disorders in TMD were malocclusion (occlusal disorders, missing teeth, suboptimal prosthetics, chewing on one side and other causes) and parafunctional activity (night and/or daytime bruxism), which leads to increased load on the TMJ and muscles that provide chewing (temporal, masticatory, medial and lateral pterygoid). Facial and jaw injuries and emotional disorders also played a significant role. In particular, the presence of symptoms of depression doubles the likelihood of developing the arthralgic form of TMD, and anxiety disorders more often accompany myalgia in TMD [15, 16]. Some authors [7] point to the role of orthopedic disorders (for example, short leg syndrome) in the genesis of TMD. During an orthopedic examination, a significant number of patients (66%) reveal asymmetries of the shoulders, shoulder blades, and shortening of one leg, which causes a compensatory change in posture and muscle imbalance throughout the entire spine. The “forward head posture” also has a serious influence on the occurrence of the myogenic form of TMD [17].
However, in recent years, a number of authors have expressed doubts about the exclusive role of dental pathology in the development of TMD. Indicate a frequent combination of TMD and various types of headache. In patients with TMD, the most common primary form of headache is migraine (55.3%), the prevalence of tension-type headache is 30.2% [18]. According to other authors [19], the prevalence of TMD in patients with chronic daily headache is 58.1%.
In recent years, the works of leading Russian and foreign researchers of chronic pain [20-22] have for the first time suggested the possible central causes of TMD, in particular the role of possible dysfunction of pain control systems. Thus, it has been shown that the prevalence of the painful form of TMD in chronic migraine is significantly higher than that in episodic migraine. The authors suggested that pain and myofascial pain syndrome in TMD may be caused by impaired processing of pain impulses in the central nervous system and are not related to peripheral/dental factors.
Treatment
Based on the current understanding of the pathophysiology of TMD, a number of treatment options have been developed. In neurological practice, treatment of TMD includes a wide range of non-drug and pharmacological approaches:
1. Patient education.
Educating patients about the causes and form of TMD and the importance of behavior modification (eg, actively focusing on not clenching teeth) is important. In case of acute pain, it is necessary to recommend a temporary refusal to eat solid foods and open the mouth wide.
2. Nonsteroidal anti-inflammatory drugs
(NSAIDs) are often the first choice drugs and are effective in relieving TMD pain. Among the large group of NSAIDs, the drug nimesulide (Nise) deserves special attention. The difference in clinical efficacy and tolerability of different NSAIDs may be due to different selectivity for COX-1 and COX-2 inhibition. Nimesulide is primarily a COX-2 inhibitor with a wide range of additional effects, which helps explain its specific anti-inflammatory and analgesic activity. More than 200 clinical studies have assessed the effectiveness of nimesulide in a wide range of pain syndromes (tooth extraction and other dental operations, hypertension, back pain, joint pain, dysmenorrhea). In these studies, nimesulide systematically demonstrated a reduction in inflammatory pain that was significantly superior to that of placebo and at least equal to or in some cases more effective than other NSAIDs [23].
The main clinical benefit of nimesulide is the time to onset and duration of pain relief. Compared to other NSAIDs, nimesulide has a faster onset of analgesic action, namely 15 minutes after oral administration [24]. It should also be noted that a rapid onset of action was noted in patients with chronic pain syndrome.
A significant advantage of this drug is the lower relative risk of complications of the upper gastrointestinal tract compared with non-selective NSAIDs due to its predominant effect on COX-2. However, a single dose of nimesulide provided higher efficacy and a faster onset of analgesic action than comparable single doses of selective COX-2 inhibitors such as celecoxib and rofecoxib [25]. When comparing nimesulide with the non-selective NSAID diclofenac, the drug showed comparable efficacy, but better overall tolerability [26].
The overall risk of severe liver reactions associated with NSAID use is low. The incidence of liver injury associated with the use of nimesulide is within the frequency range for other NSAIDs [23].
The use of all NSAIDs is associated with some cardiovascular risk and in patients with hypertension, hypercholesterolemia and cardiovascular disease, all NSAIDs should be used with caution, especially in the elderly. Risks and benefits should be assessed on an individual basis and the lowest effective dose recommended for the shortest possible period of time. Many data indicate that nimesulide demonstrates a low overall risk of cardiovascular events such as myocardial infarction or congestive heart failure [27].
An international panel of experts concluded that, when used appropriately, nimesulide remains an extremely important and safe treatment option for a variety of conditions characterized by acute inflammatory pain due to its rapid onset of analgesic action and proven positive benefit/risk profile [23].
For TMD, Nise is recommended to be used at a dose of 100 mg 2 times a day. The duration of its use, like other NSAIDs, should be limited to the minimum necessary time.
3. Gymnastics
. After applying a cold compress, exercises are performed to stretch the masticatory muscles, then a warm towel must be applied.
4. Cognitive behavioral psychotherapy and biofeedback
communications are also highly efficient.
For chronic TMD, it is recommended:
1. Prescription of the tricyclic antidepressant amitriptyline (up to 75 mg/day). The choice of amitriptyline as a first-line drug is due to the relatively high risk of developing bruxism while taking selective serotonin reuptake inhibitors [28].
2. Referring the patient to a dentist to select a special muscle relaxant splint (especially in the case of night bruxism) and assess the presence and correction of occlusal disorders.
3. In the case of myofascial pain syndrome, it is possible to inject anesthetic into trigger points in the masseter, temporal and pterygoid muscles.
4. Treatment with botulinum toxin type A for the painful form of TMD, which has demonstrated high effectiveness in a large volume of studies [9, 29]. Such therapy can allow not only to achieve long-term and sustainable relaxation of the muscles of the masticatory group and relief of pain associated with myofascial pain syndrome in these muscles, but also temporary remission of nocturnal bruxism, which will reduce the risk of developing an intra-articular form of TMD.
5. Conducting comprehensive treatment of comorbid diseases, in particular depression, anxiety disorders, chronic pain.
6. In case of proven presence of intra-articular form of TMD, impaired jaw function and lack of effect of conservative therapy, the patient should be referred to a maxillofacial surgeon [30].
TMD is considered today to be the most common cause of chronic facial pain not associated with dental disease. It has been shown that facial pain in many cases is caused by hypertonicity and myofascial syndrome in the masticatory muscles without pathological changes in the structures of the joint itself. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form, most patients can and should receive effective care from a neurologist. To fully diagnose the nature of TMD, one should rely on the DC/TMD diagnostic criteria for clinical use. These criteria are based on history and clinical examination (correct palpation of the temporal and masticatory muscles) and do not necessarily require imaging studies. If typical symptoms of intra-articular pathology (primarily sound) are detected, an MRI of the joint is indicated to confirm the diagnosis.
Currently, TMD is considered a disease with a multifactorial etiology. Myofascial pain syndrome in the muscles of the masticatory group can be considered as a manifestation of a violation of antinociceptive functions, i.e., it is a reflection of central sensitization and a violation of descending pain control.
Treatment of the painful form of TMD at the first stage should be carried out by a neurologist. Recommendations for the treatment of TMD include patient education, NSAIDs, cognitive behavioral therapy, and biofeedback. For chronic pain, it is also possible to prescribe amitriptyline, administer injections of anesthetics and botulinum toxin type A, as well as referral to a dentist and maxillofacial surgeon.
The authors declare no conflict of interest.
Pathogenesis
The study of the mechanisms of development of pathology allowed us to come to conclusions about their progression associated with a lack of physiological endurance of the joint.
The resulting injuries and the appearance of inflammation lead to improper distribution or excessive load on the tissue, which causes disruption of the synchronization of the joints, causing loss of functionality of the muscular system. The result of the development of such unpleasant processes is a disruption of the nutrition of cartilage tissue, as well as a gradual loss of their elasticity, which inevitably leads to destruction.
Simultaneously with all of the above, serious transformations of bone tissue develop, which provokes the formation of growths that modify the elements of the joint: the head of the lower jaw changes shape, and signs of osteoporosis are visible.
As a result of the uncontrolled course of pathological processes, severe deformation and serious disruption of the tissue structure occur.
Diagnostic methods
Medical diagnosis is carried out using x-ray examination, the results of which make it possible to determine the type and stage of changes occurring.
In addition to radiographic diagnostics, in order to make the most accurate diagnosis, laboratory tests of urine and blood, as well as additional instrumental research methods, can be used.
Self-diagnosis reminder
Changes such as:
- the appearance of crunching/clicking sounds when performing various types of movements;
- decreased jaw mobility, manifested when eating, yawning, etc.;
- hearing impairment;
- decreased visual ability;
- pain of a pressing or bursting type, localized mainly in the temporal or parotid-masticatory region of the head;
- periodic convulsions accompanied by painful sensations;
- dysfunction of the vestibular apparatus;
- increased fatigue when chewing food, difficulty eating solid foods;
- partial loss of facial expression;
- numbness of the skin and mucous membranes in the area of the affected joint.
There are two main types of TMJ dysfunction:
- Myogenic (source: muscle pain);
- Arthrogenic (associated with TMJ condition).
Myogenic TMJ dysfunction usually occurs due to fatigue or tension in the masseter or accessory muscles. Leads to facial pain, headaches, and sometimes neck pain.
Arthrogenic dysfunction of the TMJ, as a rule, is the result of inflammation, degenerative changes in hard and soft tissues in the joint. It most often occurs due to capsulitis or synoviitis (inflammation), slipped discs, and degenerative arthritis.