Pathology of the connecting joint between the lower jaw and the temporal bone. In the acute stage, the following symptoms are noted:
- intense pain in the affected area;
- swelling of the skin over the joint;
- restriction of movements when opening and closing the jaw;
- increased basal temperature.
To make a diagnosis, the doctor examines the patient’s medical history, conducts an examination, and prescribes computer tests.
Methods of treating the disease:
- jaw immobilization;
- antibiotic therapy;
- local administration of corticosteroids;
- myogymnastics;
- physiotherapeutic measures.
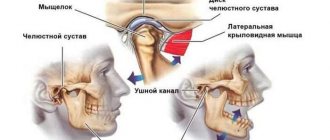
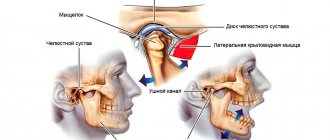
Features of the structure of the temporomandibular joint
The temporomandibular joint is involved in any movement of the jaw
The temporomandibular joint is a complex structure of two pairs of bones, on the left and right sides respectively. The peculiarity of arthritis in this area is that the paired bones are closely interconnected, so damage to the temporal bone on the right will necessarily negatively affect the condition of the mandibular bone, and vice versa.
TMJ arthritis always affects the bones symmetrically. Therefore, with the development of the disease on the right, over time there is a disruption of the joint in the left side of the head.
The temporomandibular joint is characterized by high mobility and is involved in almost any movement of the head and jaw. The process of chewing food, active facial expressions, conversation - the temporomandibular joint is involved in all these simple actions. It works constantly and withstands intense loads every day.
The articulation is formed by the upper part of the mandibular bone and the fossa of the temporal bone. The joint is small in size, but hidden by a large number of strong elastic ligaments. High mobility of the jaw is ensured by a disc hidden in the articular cavity.
Disruption of the normal functioning of the TMJ due to arthritis leads to the development of severe symptoms and significantly worsens the patient’s quality of life. This disease is quite difficult to treat and requires an integrated approach.
Methods for diagnosing arthritis of the jaw joint
Arthritis on x-ray
Diagnosis and treatment of the inflammatory process in the jaw joint area can be carried out by different specialists, which depends on the cause that caused its development. This could be an ENT doctor, a dentist, a traumatologist, an infectious disease specialist, or a dermatovenerologist.
The main diagnostic measures include:
- radiography . During this diagnostic exercise, widening or narrowing of the joint space is detected, which indicates acute or chronic arthritis of the TMJ, respectively;
- magnetic resonance imaging . The method allows you to study the condition of soft tissues, estimate the amount of fluid in the joint cavity;
- CT scan . This method of research makes it possible to differentiate between healthy and damaged tissues;
- ultrasound diagnostics . Using this research method, it is possible to visualize the fluid in the joint cavity. However, it is impossible to fully study the structure of soft tissues in this way.
Note! Acute arthritis of the TMJ is differentiated from such pathologies as acute otitis media, trigeminal neuralgia, gout.
After obtaining the necessary data and making a diagnosis, an individual course of treatment is developed.
What is TMJ arthritis?
Arthritis is an inflammation of the structural elements of a joint. The disease leads to impaired motor function of the affected joint and is accompanied by a number of specific symptoms that require attention.
TMJ arthritis is diagnosed in approximately 15% of cases of joint diseases. This prevalence of pathology is associated with the characteristics of the load to which this joint is exposed daily.
The inflammatory process in arthritis begins with the joint capsule and the tissues around them. The disease progresses slowly, gradually affecting the synovium of the joint. Over time, bone tissue is also involved in the inflammatory process, which leads to deformation of the joint and disruption of its functions. In advanced cases, cartilage tissue is destroyed and connective tissue is formed directly in the cavity of the affected joint. This is the most unfavorable prognosis for arthritis, since such changes entail severe impairment of the motor function of the temporomandibular joint. This can lead to severe contracture, joint deformation, and immobility of the lower jaw.
Causes of TMJ dysfunction
Conventionally, we can distinguish 3 main reasons for the development and etiology of the clinic of TMJ jaw joint dysfunction:
- Imbalance and disruption of the nervous coordination of the jaw muscles that raise and lower the lower jaw. Most often, the tone and tension of the muscle fibers in the right and left masticatory muscles are first disturbed, and then their imbalance occurs, irritation of the bilaminar zone and pain when chewing and swallowing.
- Chronic stress, over a long period of time (from a year or more), caused by a disorder of the central nervous system and higher nervous activity.
- Malocclusion and occlusion (closing) of teeth, coupled with non-standard sizes and position of the jaws relative to each other and the base of the skull.
As a rule, all of the above factors, to a greater or lesser extent, occur if a diagnosis of TMJ dysfunction syndrome is made. Reviews from patients and a forum on the Internet confirm this.
A hereditary predisposition to dysfunction of the jaw joints has been proven, with genetic anomalies associated with malocclusion, especially with micrognathia and macrognathia of the lower or upper jaw.
Reasons for the development of the disease
Arthritis of the temporomandibular joint is a severe inflammatory disease
The exact causes of the development of arthritis of the mandibular joint have not yet been established. This form of pathology rarely appears as part of the symptom complex of rheumatoid arthritis due to the specific structure of the joint, while rheumatoid arthritis primarily affects small joints of the extremities.
Arthritis of the temporomandibular joint was assigned the ICD-10 code K07.6. Thus, the international classification of diseases ICD-10 classifies arthritis of the temporomandibular joint as a group of maxillofacial pathologies, but not as a joint disease.
If the trigeminal nerve and lower jaw are affected, TMJ arthritis according to ICD-10 may have a different code - G50. With degenerative-dystrophic changes in cartilage tissue, this pathology is assigned code M19.8 in ICD-10 protocols.
Conventionally, the causes of the development of the disease can be classified into three groups:
- infectious;
- non-infectious;
- specific.
Infectious causes are the penetration of pathogenic agents into the capsule of the temporomandibular joint. Infection occurs against the background of infection with tuberculosis, syphilis, and gonorrhea. Infectious causes may also include the measles virus. Often arthritis is a consequence of serious illnesses, for example, a recent flu that was treated incorrectly.
Infectious arthritis of the TMJ can develop against the background of dental and otolaryngological diseases. In this case, the infection penetrates the joint by hematogenous or contact route. The cause of infection of the joint can be advanced caries, acute otitis media of the middle ear, abscess of the ear canal .
Non-infectious arthritis develops as a result of injuries and bruises. They are a consequence of the lack of necessary treatment for fractures and injuries of the jaw.
Specific arthritis is a disease that develops against the background of another chronic pathology. They may be associated with damage to the facial nerves, as a result of which the functioning of the joints is impaired. TMJ arthritis may be part of the symptom complex of systemic lupus erythematosus or other autoimmune disorders.
In fairness, it should be clarified that damage to the temporomandibular joint against the background of systemic connective tissue diseases is very rare; most often the complication spreads to the small joints of the lower and upper extremities.
Risk factors
A number of reasons can lead to the development of arthritis of the jaw.
Violation of the structure occurs due to the following reasons:
- traumatic factor. The cause in this case may be a blow, a fracture, or a sudden opening of the mouth;
- infectious diseases of the ENT organs or lower jaw. Arthritis of the maxillary joint is caused by streptococci, chlamydia, mycobacterium tuberculosis, and various viruses;
- osteomyelitis;
- untreated caries or periodontitis;
- otitis, mumps. Arthritis is a complication of these pathologies;
- gout;
- reactive arthritis;
- systemic lupus erythematosus;
- metabolic disorders;
- diabetes;
- thyroid diseases;
- rheumatoid arthritis.
Sometimes inflammation is a consequence of hypothermia.
Classification of arthritis
TMJ arthritis is a nonspecific disease, despite its widespread occurrence. The forms and types of the disease are classified according to the nature of development and the nature of the course of the pathology.
Due to their development, the following types of arthritis are distinguished:
- infectious;
- non-infectious;
- traumatic.
Infectious arthritis, in turn, is divided into contact and hematogenous. Contact arthritis develops due to the penetration of pathogenic microorganisms into the joint against the background of infection of organs located in close proximity to the TMJ. Hematogenous arthritis is a consequence of the spread of infection in an ascending direction through the bloodstream. This form of the disease develops in tuberculosis, measles, syphilis, and other severe bacterial pathologies.
The cause of the development of traumatic arthritis of the TMJ are injuries, bruises, fractures, and tendon compression. This form of the disease can occur after severe road accidents or in athletes who have injured their jaw.
Non-infectious arthritis can be traumatic, rheumatoid (autoimmune) or reactive. Reactive arthritis develops against the background of existing infectious diseases, but no pathogenic microorganisms are found in the synovium of the joint.
Separately, dystrophic arthritis is distinguished, which is a consequence of disruption of local metabolic processes. In this case, there is a lack of nutrition of the cartilage tissue, its gradual degeneration and loss of elasticity of the cartilage.
According to the nature of the course, the inflammatory disease is divided into chronic and acute. Acute TMJ arthritis is characterized by pronounced symptoms and a general deterioration in well-being. The disease may be accompanied by suppuration in the joint capsule and infection of the periarticular tissues. Chronic TMJ arthritis is characterized by moderate severity of symptoms, but with periodic exacerbations.
In the absence of adequate therapy, acute arthritis can become chronic, which is difficult to treat.
With arthritis of the temporomandibular joint, symptoms depend on the type of inflammatory reaction and the form of the disease. Regardless of the cause of TMJ arthritis, the symptoms require attention, so you should consult a doctor if you experience the slightest discomfort in the jaw, since the advanced form of the disease is difficult to cure.
Types of deviations in the maxillofacial joint
The clinical picture of this disease depends on the form in which arthritis of the jaw joint occurs.
Types of disease:
| Type of pathology | Characteristics |
| Acute form | The predominant symptoms in this case are severe pain in the affected area and swelling of the soft tissues. Typically, acute arthritis of the jaw joint occurs after traumatic injury. |
| Chronic arthritis | With this form, aching pain is constantly observed in the jaw joint. In the morning, jaw mobility is limited. Body temperature usually does not increase, the general condition of the body is satisfactory. |
| Infectious arthritis of the TMJ | Usually this type of pathology is a consequence of previous diseases - influenza, tonsillitis. In the infectious form of arthritis, severe pain is observed, during which it is impossible to open the mouth freely. Unpleasant sensations radiate to the area of the ear, back of the head, and temple. |
| Traumatic | This is the most common form of arthritis of the maxillary joint. It occurs against the background of an injury. |
| Specific | This type of disease occurs quite rarely. Typically, specific arthritis is a consequence of previous diseases - syphilis, gonorrhea, tuberculosis. |
| Non-specific | In this case, the inflammatory process occurs due to traumatic or rheumatoid factors. |
| Purulent | This form of pathology is a consequence of acute arthritis, which has been neglected. A thickening appears in the area of the mandibular joint, and body temperature rises. |
| Rheumatoid | The disease manifests itself in constant pain localized in the area of the maxillary joint. In this case, the clinical picture is often supplemented by pain that is localized in the area of the knee, hip or elbow joint. |
Depending on what exactly caused the development of the inflammatory process, the following paths are distinguished:
- hematogenous . In this case, the pathogen penetrates the joint area along with the blood flow. This method of infection is possible with tuberculosis, syphilis, gonorrhea, scarlet fever, measles;
- contact . The disease develops against the background of damage to the sections that are located next to the maxillary joints. A similar thing is observed with otitis media, purulent mumps, phlegmon or abscess of the parotid-masticatory area;
- straight . Arthritis of the maxillary facial joint in this case develops due to direct infection, which occurs due to injuries or fractures of the jaw.
It is possible to determine the form in which the pathological process occurs only after carrying out specific diagnostic measures.
Specific symptoms
Treatment for temporomandibular joint arthritis depends on the form of the disease
The following symptoms are characteristic of TMJ inflammation:
- pain in the affected joint;
- limitation of jaw mobility;
- swelling of the skin around the affected area;
- severe hyperemia.
The pain syndrome intensifies when opening the mouth, while chewing food and with any other load on the joint. The pain intensifies in the first half of the day and gradually disappears in the evening. When the TMJ is affected, difficulty opening the mouth is observed. This is due to muscle stiffness due to pressure from the inflamed joint.
When you try to open your mouth wide, there is a noticeable skew of the jaw towards the healthy half. This is one of the characteristic symptoms of TMJ arthritis.
With infectious inflammation, the pain is acute and excruciating. A person may feel a feeling of fullness in the jaw or a pulsating joint. In this case, the skin turns red and the temperature of the epidermis around the inflamed joint rises.
Suppuration in the joint capsule is accompanied by a general deterioration in health. Patients complain of increased body temperature, decreased appetite, and severe fatigue.
Symptoms and treatment of temporomandibular joint arthritis depend on the form of the disease. In acute arthritis, excruciating pain is observed and the patient requires urgent drug therapy. With chronic arthritis, patients experience discomfort when trying to open their mouth, problems chewing food, and aching pain in the jaw. In this case, treatment should be aimed at normalizing metabolic processes in the joint and relieving swelling.
TMJ diseases
Diseases of the TMJ (temporomandibular joint) are characterized by a common symptom - dysfunction of the masticatory apparatus - and are the competence of orthopedic dentistry.
Arthrosis of the TMJ
Arthrosis of the TMJ is a disease that occurs as a result of uneven load on the joint: on the one hand, compression, and on the other, stretching. Increased loads can occur due to malocclusion, occlusion and articulation, as well as if incorrect prosthetics were performed (insufficient examination, poorly fixed fixed prosthesis, incorrectly sized bridge, excessive grinding of the tooth for a crown).
Symptoms of TMJ arthrosis:
- Pain in the joint in a calm state, inactivity;
- Clicking and crunching in the joint;
- Stiffness in the lower jaw after a night's sleep or after prolonged exercise (long conversation, chewing food);
- Limited mouth opening;
- Moving the jaw to the side when opening the mouth.
Treatment
The treatment of arthrosis of the TMJ requires an integrated approach from a group of doctors:
- Orthopedic treatment – corrects malocclusion – straightens the shape of the teeth, corrects the relationship of the dentition, installs or replaces previous dentures;
- Therapeutic treatment – partial grinding of teeth that interfere with the normal closure of the jaws;
- Physiotherapeutic methods – galvanization, massage, electrophoresis.
Arthritis of the TMJ
TMJ arthritis is inflammation of the temporomandibular joint of infectious or non-infectious origin. Initially, it spreads only to the joint capsule, then it can reach areas of the bone, accompanied by the melting of cartilage and the appearance of connective tissue in the joint cavity.
There are two stages of the disease: acute and chronic. When acute pain becomes severe, visible deformation of the face and swelling are observed. The joint is constantly stiff. In the chronic stage, painful sensations increase with movement, and in an immobilized state they are moderate or weakly noticeable. The joint is stiff in the morning.
Symptoms of the disease:
- Acute throbbing pain when moving the joint (talking, chewing), radiating to the temple, back of the head;
- Pain on palpation of the lower jaw;
- Redness of soft tissues and their swelling;
- Feeling of fullness in the jaw.
Treatment
- Immobilization of the diseased joint by applying a sling-shaped bandage to the lower jaw or other methods;
- A diet that excludes chewing food for 3 days;
- Using analgesics and cold compresses for pain relief;
- Taking antibiotics, injections of chondroprotectors and corticosteroids into the joint;
- Physiotherapeutic measures – mud therapy, ultraphonophoresis.
Ankylosis of the TMJ
Ankylosis of the TMJ is a partial or complete loss of mobility of the lower jaw, which is caused by fibrous or bony fusion of the joint surfaces. The danger of this disease is that it can occur for many years without symptoms until the cartilage completely dies. Bone ankylosis develops in childhood, while fibrous ankylosis occurs in adults.
Symptoms of the disease:
- Limitation in opening the mouth;
- Impaired breathing (night apnea and snoring), speech, chewing;
- Distortion of the face to the side;
- Shortened and underdeveloped lower jaw;
- Increased formation of plaque and tartar.
Treatment
The treatment has two goals: restoring joint mobility and facial aesthetics.
In the first stages, treatment may be limited to physiotherapeutic measures in the form of ultraphonoresis, hyaluronodase, as well as hydrocortisone injections into the joint. Sometimes they resort to mechanical expansion of the jaws under anesthesia or surgical dissection of the adhesions.
Persistent deformities and adhesions in late stages of development can only be eliminated surgically. The complexity of the operation should be taken into account due to difficulty breathing in patients with this disease. In some cases, a tracheotomy is required.
Ankylosis can be prevented by timely treatment of diseases of the facial joints and birth injuries in children.
Musculo-articular dysfunction of the TMJ
Impaired coordination of the muscles of the lower jaw and the joint, as well as the placement of the head and disc of the joint relative to the tubercle. Factors that contribute to the development of this disease may be incorrect orthodontic treatment, unprofessional implantation, bone grafting of teeth, sinus lifting, as well as endocrine, articular and other diseases.
Symptoms:
- Painful sensations in the jaw, increasing at night and with movement (in another form, painful sensations may be absent);
- Clicking sounds when moving the jaw;
- Temporary stiffness in jaw movement;
- Tension of the facial muscles, most often one-sided;
- Sleep disturbance.
Treatment
The main task is to create the correct bite for the patient and restore normal jaw closure. These tasks are carried out by grinding protruding contacts on the surface of the teeth, which interfere with the normal closure of the jaws. Advanced stages can only be treated surgically - dissection of adhesions, straightening and installation of the disc in place.
TMJ dislocation
TMJ dislocation is a displacement of the head of the joint beyond its normal location, in which the function of the lower jaw is completely disrupted. There are 2 types:
- traumatic - received as a result of a blow to the jaw, yawning or screaming;
- habitual - which develop as a result of stretching of the joint capsule and ligaments.
Symptoms:
- The lower jaw is displaced downwards, the mouth does not close on its own;
- Excessive salivation;
- The appearance of depressions in the area of the tragus of the ear and protruding heads of the joint in the area of the cheekbones;
- Strong pain.
Treatment
- Reduction of the joint;
- Immobilization of the TMJ.
Diagnostics
The first manifestation and sign of arthritis of the temporomandibular joint are symptoms of limited jaw mobility and pain. This should prompt the patient to see a doctor as soon as possible. In this case, a dentist, otolaryngologist or rheumatologist can make a diagnosis. To accurately determine the nature of inflammation, the following tests and examinations are necessary:
- blood analysis;
- X-ray of the jaw;
- CT, MRI or ultrasound of the jaw.
A blood test reveals the very fact of the inflammatory reaction, and also shows the level of rheumatoid factor, which is necessary to exclude the rheumatoid nature of the disease. X-ray allows you to accurately visualize changes in bone tissue and determine the localization of the inflammatory process. MRI, CT and ultrasound must be performed to exclude the oncological nature of the disease. These studies also show the condition of the cartilage and tissue around the joint, as well as the accumulation of fluid in the joint cavity.
Clinical picture (symptoms)
Arthritis is accompanied by pain and discomfort.
The disease manifests itself in the following characteristic symptoms:
- pain in the jaw area, which radiates to other parts of the face and intensifies with movements and opening the mouth;
- dizziness;
- sleep disorders;
- limited movement in the joint;
- feverish condition;
- inflammation of the skin and soft tissues around the joints;
- elevated temperature;
- clicking in the jaw area when it moves;
- temperature rise up to 38 degrees, sometimes higher;
- pain when palpating the affected area (joint pain);
- deformation of the contours of the face due to the fact that the chin “goes” to the side;
- feeling of weakness, increased fatigue;
- hearing impairment.
Important! With arthritis of the jaw joint there is a risk of the formation of purulent inflammation. In this case, the joint swells and the skin becomes red and hypersensitive. A lump is felt in the area of the mandibular joint. The shade of the skin changes, speech and chewing functions are impaired.
Treatment principle
For arthritis of the temporomandibular joint, medications are prescribed
For temporomandibular joint arthritis, treatment includes medication and physical therapy.
Therapy includes:
- immobilization of the diseased joint;
- relief of inflammation;
- pain relief for an inflamed joint;
- improvement of local metabolic processes.
First of all, it is necessary to fix the jaw in such a way as to minimize traumatic loads on the inflamed joint. Further therapeutic measures depend on the type of inflammatory process.
Infectious TMJ arthritis is treated with antibiotics. It is first necessary to perform a puncture to obtain a sample of fluid from the joint, which is examined under a microscope. This allows you to accurately identify the causative agent of the disease. Antibiotics are prescribed in various forms, including tablets and intra-articular injections. In case of suppuration in the joint capsule, it is necessary to use the technique of installing drainage to cleanse the cavity of purulent exudate.
For acute non-infectious arthritis, corticosteroid therapy is practiced. These drugs stop the inflammatory reaction and reduce pain.
To reduce pain, taking non-steroidal anti-inflammatory drugs is indicated - Ibuprofen, Diclofenac, Ketoprofen, Nimesulide. These drugs are taken in tablets or intramuscular injections.
Chronic arthritis of the temporomandibular joint is treated with physiotherapy, treatment is aimed at restoring normal blood flow and nutrition of cartilage tissue.
After relief of inflammation, chondroprotectors and dietary supplements for joints are prescribed. This is necessary to maintain the elasticity of cartilage tissue and accelerate the regeneration of the affected joint.
Treatment options
Pathology is treated in the following ways:
- Fixation
fixation . The first thing that is done when arthritis of the jaw joint is diagnosed is to ensure the immobility of the affected structure. To do this, apply a bandage. On the side of the diseased joint, between the teeth, a special plate is placed, which should remain there for 2-3 days;
- taking medications . The patient is prescribed analgesics to suppress pain and reduce temperature (Nurofen, Analgin), antibacterial drugs (Tetracycline, Amoxicillin), non-steroidal anti-inflammatory drugs (Celecoxib, Nimesulide). Immunosuppressants may be prescribed, which is required for rheumatoid arthritis. The group of such drugs includes Etanercept, Leflunomide;
- drug blockade . The goal of therapy is to relieve pain in the affected joint. Novocaine injections may be prescribed;
- ointments, compresses . For pain in the affected joint, topical agents are prescribed, for example, ointments containing bee or snake venom. Ointments, by heating the affected area, restore joint mobility and suppress muscle spasms;
- sanitation of the oral cavity . This method is required for rheumatoid arthritis.
Drug blockade
Exercise is another way to restore the mobility of an inflamed joint at home. The specialist prescribes a course of therapeutic exercises for the patient. The most effective and common exercise is to open the mouth using only the upper part of the jaw.
Physiotherapy helps with TMJ arthritis. Effective measures include:
- magnetic therapy;
- laser therapy;
- mud therapy;
- ultrasound therapy;
- cryotherapy.
Therapeutic massage sessions are also available .
Surgical intervention is carried out in case of development of a purulent process, rupture of the joint capsule, fractures of the articular surfaces. During the operation, the specialist installs a drainage system.
Traditional methods of treatment include the following:
- cabbage leaf compress . You need to take one sheet, iron it with a heated iron, and apply it to the affected area. Carry out the procedure 1-2 times a day;
- compress with sea salt . It is necessary to calcinate natural sea salt in a frying pan, then wrap it in a piece of linen cloth. Apply to the affected area. Repeat application up to two times a day;
- infusion of yarrow . Pour 4 tablespoons of raw material into 400 ml of boiling water. The product should sit for 2 hours. You need to take it 4 times a day, 50 ml each time.
The condition must be corrected with the help of a doctor.
Prevention and prognosis
Symptoms of inflammation in TMJ arthritis appear quite quickly, the disease progresses rapidly, so the prognosis depends on how quickly the disease is detected and treatment is started. Timely adequate therapy will allow you to completely get rid of the disease in 2-3 weeks. At the same time, TMJ arthritis almost never develops again. Treatment of a chronic disease will take about 1-1.5 months, taking into account a long course of physiotherapy.
There is no specific prevention for TMJ arthritis. It comes down to being attentive to your own well-being and timely treatment of any infectious diseases. It is important to prevent the presence of chronic foci of infection in the body, especially in the oral cavity.
Related Articles
Osteoporosis of the jaw: causes, symptoms and methods of treating pathology
How is arthritis determined according to ICD-10: codes for different types of disease
Arthrosis-arthritis of the knee joint: features of the disease and treatment methods
Undifferentiated arthritis: features of the disease, causes of development, ICD-10 code and treatment
Synovitis of the knee joint: causes of development, ICD-10 code, symptoms and treatment
Arthrosis-arthritis of the hip joint: ICD-10 code, treatment methods, therapeutic exercises
Prevention
To minimize the risk of developing a pathological process, it is recommended to follow the following rules:
- promptly treat diseases in which the formation of purulent foci occurs;
- protect yourself from traumatic factors;
- avoid hypothermia;
- promptly treat nasopharyngeal pathologies;
- treat acute infectious processes;
- eliminate dental problems.
To prevent the pathological process from worsening, it is important to seek help from a medical facility as quickly as possible.
Classification
TMJ arthritis can be:
- Spicy;
- Chronic;
- Bilateral;
- Unilateral;
- Infectious;
- Rheumatoid;
- Purulent;
- Deforming osteoarthritis;
Infection may result from direct spread or hematogenous spread. The area becomes inflamed, movement is limited, and pain appears. Bone destruction may be diagnosed. Acute traumatic arthritis can sometimes be associated with severe removal of the masticatory organ. Creaking and stiffness can occur in old age when bones rub against each other. Common manifestations of rheumatism are pain, swelling, and limited movement. Secondary degenerative pathology most often develops after injury. The patient has difficulty opening his mouth, and the pain is usually one-sided. The disease code according to ICD-10 (International Classification of Diseases) is K07.6.
Diagnosis, treatment and prognosis
| Click to sign up for a FREE consultation |
Diagnosis of the disease includes a number of radiological, clinical, and functional methods. When visiting a doctor, the oral cavity will be examined, complaints will be collected, and the existing range of motion will be determined. The examination also uses a diagnostic jaw model.
X-rays can detect pronounced signs of the disease; CT scans can identify early signs, which is important for timely treatment. In addition, consultations with an orthodontist, endocrinologist, rheumatologist and other related specialists will be scheduled. Among the prescribed studies are rheography, arthrophonography, axiography, and gnathography.
After receiving the diagnostic results, the patient will be prescribed physiotherapeutic, orthodontic, therapeutic and other procedures. During the entire treatment period, it is necessary to follow a gentle diet, which will help reduce the load on the joint. In addition, heavy loads on the jaws, including speaking and chewing, are eliminated.
At the initial stage, factors that lead to joint overload are eliminated to relieve pain, NSAIDs are used in the form of ointments and tablets. In later stages, measures such as removal of the articular head or disc and subsequent installation of a graft are indicated.
A favorable prognosis can be given only in case of timely treatment of the disease, rational prosthetics, normalization of the bite, and elimination of concomitant diseases. At an advanced stage, it will not be possible to completely restore lost functions without surgery. But even after a successful operation, regular follow-up with a dentist is recommended.